Whole brain radiotherapy for patients with poor prognosis: possibilities for the impact of the QUARTZ trial
Whole brain radiotherapy (WBRT) has been a standard treatment in the management of patients with brain metastases since the initial report on the utility of WBRT by Chao in 1954 (1). However, the benefit of WBRT for patients with poor prognosis continues to be debated (2). The Medical Research Council’s (MRC’s) QUARTZ study (Quality of Life after Treatment for Brain Metastases) was designed to provide data regarding the impact of WBRT on quality of life for patients with metastatic non-small cell lung cancer and brain metastases with a poor prognosis and for whom benefit or lack of benefit of WBRT cannot be clearly defined (3). The trial has completed accrual, and results are expected to be reported in the coming months. However, the MRC took the unique step of releasing interim results in 2013 that did not show any hint of difference between quality of life and survival among patients who received WBRT, dexamethasone and optimal supportive care (OSC) versus dexamethasone and OSC alone (4); as we anticipate final results of this trial, it is worth reviewing the interim analysis in more detail and exploring the potential impact this study will have on the management of patients with poor prognosis and brain metastases.
The QUARTZ trial was a randomized, phase III, non-inferiority trial designed to determine the impact of WBRT in addition to OSC on quality of life as measured by quality adjusted life years (QALYs) determined by the EQ-5D quality of life scale. However, this multi-center trial was in danger of early termination due to poor accrual. There were multiple concerns that were thought to be impacting accrual: a lack of phase II data that supported the study hypothesis; strong patient preferences for or against WBRT and strong clinician preferences for or against WBRT.
The interim analysis reported on results of 151 patients (of 534 planned accrual) who underwent randomization, 75 to the WBRT arm and 76 to the OSC arm. The interim analysis showed no statistically significant differences in average quality of life, symptom scores or overall survival. The interim analysis was surprising, though, in that the median survival of patients on both study arms was shorter than might have been expected. Median survival for patients on the WBRT arm was 49 days versus 51 days with OSC alone (hazard ratio 1.11; 95% confidence interval 0.80-1.53).
It is interesting to put these survival data in context of historical cohorts from the recursive partitioning analysis (RPA) from thousands of patients with brain metastases treated by the Radiation Therapy Oncology Group (RTOG) (5). Patients on the QUARTZ trial were divided primarily between RPA class II and RPA class III, with a few patients with RPA class I. Table 1 shows median survivals of patients with RTOG RPA class I, II and III compared with the patients enrolled on the WBRT arm and OSC arm of the QUARTZ trial. It is unclear why there are such differences in survival between QUARTZ and RPA, but unless the median survival of patients in the final analysis of the QUARTZ trial more closely approaches that of the RPA, there will be outstanding questions about which patients may not benefit from WBRT if survival is shorter than anticipated.
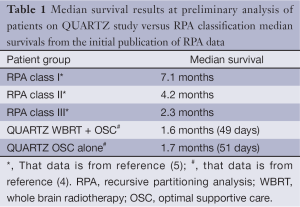
Full table
However, questions that focus only on overall survival among patients with brain metastases fundamentally miss the primary question of the QUARTZ trial: what is the impact of WBRT on quality of life, particularly for patients with short anticipated survival? This question is much harder to define. As the authors of the interim analysis suggest, both patients and clinicians approach WBRT with preconceived notions of what treatments are acceptable to them. Although some studies assessing WBRT have shown that certain parameters of quality of life decline after radiotherapy, other studies have shown improvements in quality of life, particularly for patients with better prognoses, perhaps since progressive brain metastases have been associated with increased risk of death from neurological causes and decreased quality of life (6). However, perhaps hair loss near end of life or daily trips to the radiotherapy center for 1 week have a greater impact on quality of life than the symptoms from progressive brain metastases. Perhaps the simple act of continuing treatment brings peace of mind to patients and families, in spite of any side effects of radiotherapy. These factors, and others that play into treatment decisions, are highly individualized and suggest that, regardless of the final results of the QUARTZ trial, a nuanced approach to patients with brain metastases is of utmost importance, one that is personalized and focuses on the patient and his or her wishes for care near the close of life.
In this context, it is important to ask questions fundamental to the palliative care of all patients with serious illness: what is the patient’s (and family’s) understanding of the clinical situation? What are the patient’s (and family’s) hopes and fears? What tradeoffs are the patient and family willing to make in care? As described in the qualitative study of patients with brain metastases undergoing WBRT, some of these factors include hope, knowledge, expectations for radiotherapy and current symptoms (7). The final analysis of the QUARTZ trial will hopefully help to inform these conversations. For patients who continue to struggle to define goals and evaluate tradeoffs of WBRT, it is possible that a joint palliative care/radiation oncology clinic (8) could help with decision-making, allowing patients and families to make choices that are based on the most up-to-date data and on personal and family preferences for care. Regardless of the results of the QUARTZ trial, it is through innovative programs like the one Jung and colleagues describe, that we will be best able to care for patients with brain metastases with poor prognosis.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Chao JH, Phillips R, Nickson JJ. Roentgen-ray therapy of cerebral metastases. Cancer 1954;7:682-9. [PubMed]
- Nieder C, Norum J, Dalhaug A, et al. Radiotherapy versus best supportive care in patients with brain metastases and adverse prognostic factors. Clin Exp Metastasis 2013;30:723-9. [PubMed]
- Dexamethasone and Supportive Care With or Without Whole-Brain Radiation Therapy in Treating Patients With Non-Small Cell Lung Cancer That Has Spread to the Brain and Cannot Be Removed By Surgery. [Accessed May 1, 2015]. Available online: https://clinicaltrials.gov/ct2/show/NCT00403065?term=QUARTZ&rank=6
- Langley RE, Stephens RJ, Nankivell M, et al. Interim data from the Medical Research Council QUARTZ Trial: does whole brain radiotherapy affect the survival and quality of life of patients with brain metastases from non-small cell lung cancer? Clin Oncol (R Coll Radiol) 2013;25:e23-30. [PubMed]
- Gaspar L, Scott C, Rotman M, et al. Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys 1997;37:745-51. [PubMed]
- Wong J, Hird A, Kirou-Mauro A, et al. Quality of life in brain metastases radiation trials: a literature review. Curr Oncol 2008;15:25-45. [PubMed]
- Sze J, Marisette S, Williams D, et al. Decision making in palliative radiation therapy: reframing hope in caregivers and patients with brain metastases. Support Care Cancer 2006;14:1055-63. [PubMed]
- Jung H, Sinnarajah A, Enns B, et al. Managing brain metastases patients with and without radiotherapy: initial lessonsfrom a team-based consult service through a multidisciplinary integrated palliative oncology clinic. Support Care Cancer 2013;21:3379-86. [PubMed]


