Editor’s note:
“Palliative Radiotherapy Column” features articles emphasizing the critical role of radiotherapy in palliative care. Chairs to the columns are Dr. Edward L.W. Chow from Odette Cancer Centre, Sunnybrook Health Sciences Centre in Toronto and Dr. Stephen Lutz from Blanchard Valley Regional Cancer Center in Findlay, gathering a group of promising researchers in the field to make it an excellent column. The column includes original research manuscripts and timely review articles and perspectives relating to palliative radiotherapy, as well as editorials and commentaries on recently published trials and studies.
Debate: Single-fraction treatment should be standard in the retreatment of uncomplicated bone metastases
Pro argument
Despite multiple randomized controlled trials (RCTs) and systematic reviews (1) that have shown equivalent pain control between single-fraction and multiple-fraction radiotherapy schedules for first treatment of painful bone metastases, there remains considerable use of multiple-fraction regimens (2) and much debate around this topic (3-6). Within this context, a new frontier has opened in the palliative radiotherapy realm: should single-fraction treatment be standard in the retreatment of uncomplicated bone metastases? We emphatically believe so. Evidence in support of this will be reviewed, and how this information can be applied to day-to-day practice in palliative radiation oncology will be discussed.
There are two RCTs examining retreatment of painful bone metastases. The first trial, although small, deserves mention. In a single-institution, prospective RCT, Sayed et al. randomized 60 patients to 8 Gy single-fraction retreatment or 20 Gy in multiple fractions (five to eight, depending on site) (7). Although the study was underpowered to detect small differences and an a priori sample size calculation was not reported, the authors found no statistically significant difference in pain response between the two treatment groups.
The second trial, coordinated by the NCIC Clinical Trials Group (CTG), provides the bulk of the high-quality evidence available to answer our question. Also termed the SC.20 trial, Chow et al. randomized 850 patients to receive 8 Gy single-fraction retreatment or 20 Gy in multiple fractions (8). The trial was designed as a non-inferiority study with a pre-specified non-inferiority margin of 10%. The primary analysis was based on the intention-to-treat population, which found that overall response rate was inferior in the single-fraction arm by 4% (absolute difference) as compared with multiple-fractions (P=0.21, not statistically significant). The upper 95% confidence interval (CI) was 9.2%, thus excluding the possibility that single-fraction treatment was 10% worse. A per-protocol sensitivity analysis was performed, which demonstrated a 6% absolute decrease in response rate and an upper 95% CI of 13.2%, suggesting a possibility that single-fraction treatment could have up to 13.2% reduced pain response.
A brief discussion about clinical trial interpretation and analysis is in order. In superiority clinical trials, intention-to-treat analysis is considered a gold standard of data analysis, as it reduces the chance of a type I error (9-11). In non-inferiority trials, it has traditionally been favoured to use a per-protocol analysis as this reduces the chance that an inferior treatment appears equally efficacious to the comparator treatment due to methodological issues such as treatment non-adherence or missing data (10-12). Missing data negatively affects both intention-to-treat and per-protocol non-inferiority analyses (11), and is inherent to research in palliative oncology because patients with metastatic disease have short life expectancies. However, it has been argued that intention-to-treat plays an important role in interpretation of non-inferiority trials due to preservation of the integrity of randomization (missing data may not be missing in a randomized manner), as well as providing a representative, real-world estimate of effectiveness (or isoeffectiveness) (11). The proportion of patients with missing data was balanced between treatment groups in the SC.20 trial (31% and 33%), which reduced the chance that missing data acted as a source of bias in the analysis (8). Therefore, excluding the considerable proportion of missing patients from final analysis could preclude establishing a realistic picture of benefit or lack thereof. External validity is a major concern in applying any clinical trial result to day-to-day practice, particularly in palliative oncology. An intention-to-treat analysis provides clinicians and patients with data that mirrors reality in the clinic, whereas a per-protocol analysis can obfuscate and confuse.
Let us suppose, for a moment, that 6% is the actual absolute point estimate of improved pain control with multiple-fraction retreatment. The number needed-to-treat (NNT) is 16.7 patients; therefore, 16.7 patients would receive an excess of 67 radiotherapy fractions (16.7×4 fractions) to provide a single patient with improved pain control. To put this into context, use of multiple-fraction retreatment means almost 3 person-months of time that palliative oncology patients need to spend in the radiotherapy clinic. Indeed, this is a conservative estimate given that the intention-to-treat point estimate is 4.0% (NNT =25) and many patients receiving multiple-fractions would receive not five, but eight fractions.
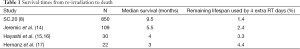
Clinicians should keep in mind that the life expectancy of patients requiring re-irradiation for painful bone metastases is limited. In SC.20, the median survival of patients was between 9.3 to 9.7 months (8); this is likely an overestimate given the inherent bias against enrolling clinical trial participants with comorbidities or advanced age (13). Three other studies have reported survival of patients receiving re-irradiation; these results are summarized in Table 1. Just under 5% of a person’s remaining lifespan could be spent waiting in, and travelling to and from a radiotherapy clinic in a multiple-fraction regimen; this represents a substantial burden upon palliative oncology patients and families that could be reduced with single-fraction re-irradiation. It should be noted, however, that estimation of overall survival was not a primary endpoint of the cited studies and may be subject to bias from patients lost to follow-up.
Full table
The SC.20 trial did find statistically significant increases in adverse effects with multiple-fraction treatment, including a 10% absolute increase in dermatitis at 2 weeks, anorexia, and vomiting (8). Patients also express a preference for single-fraction radiotherapy (in the first-treatment setting) when information is presented in a clear manner to them (18). Finally, numerous cost-effectiveness analyses are available for first-treatment of bone metastases, demonstrating reduced cost to health care systems with single-fraction treatment (19-22).
Effectiveness of single-fraction treatment is described by the randomized SC.20 trial, but also corroborated in a meta-analysis by Bedard et al. (23). In a pooled estimate from a radiotherapy retreatment systematic review (1), the overall response rate was identical between every combination of single-fraction and multiple-fraction treatment and retreatment. For example, overall response rate with single-fraction initial treatment followed by single-fraction or multiple-fraction retreatment was 71% and 72%, respectively; overall response rate with multiple-fraction initial treatment, followed by single-fraction or multiple-fraction retreatment, was identical (73%). Despite these benefits, why do some clinicians continue to offer multiple-fraction retreatment?
A common argument for patients who were initially treated with a single-fraction is that if the initial treatment did not provide pain relief, then retreatment with a single-fraction would be ineffective as well. This is not supported by the evidence (23). Clinician bias to retreatment after initial single-fraction treatment is well documented. In a Radiation Therapy Oncology Group trial (RTOG 9714), patients who received single-fraction treatment had the same pain response as multiple-fractions but ended up receiving more retreatment (24). The Dutch Bone Metastasis Study found single-fraction patients were re-treated sooner, despite having less pain prior to retreatment (25). Other arguments for multiple-fraction treatment include better re-mineralization (26) and potentially reduced fracture rate, but a meta-analysis of first-treatment has not found a statistically significant increase in pathologic fracture or spinal cord compression with single-fraction treatment, even with inclusion of more than 2,000 patients in pooled analysis (1).
There likely exist subsets of patients who may benefit from alternative therapies. Patients with complicated bone metastases or impending pathologic fracture should receive surgery followed by post-operative, fractionated radiotherapy (with attention to cumulative dose-tolerance of organs at risk in retreatment). Cancer patients with painful vertebral compression fractures due to their spine metastasis may benefit from balloon kyphoplasty to provide pain relief (27). Bone metastases arising from radioresistant histologies, such as renal cell carcinoma or melanoma, may benefit from high radiation doses that can be delivered with stereotactic body radiotherapy (SBRT) or fractionated radiation (28). Individuals with oligometastatic disease or expected long survival may also benefit from higher dose with SBRT (5,29) or fractionated radiotherapy to provide local control and pain relief. Thus, fractionated radiotherapy should be considered in post-operative patients, oligometastatic disease, radioresistant histology, or patients with good performance status and expected long survival. Nonetheless, clinicians should be aware of the tendency to over-estimate life expectancy of palliative oncology patients (30), which would then over-estimate the potential benefit of any prolonged fractionation schedule.
In summary, the available data support the feasibility, effectiveness, safety, cost-effectiveness and convenience of single-fraction retreatment. Single-fraction retreatment relieves pain from painful bone metastases, is associated with fewer adverse effects, and minimizes patient and caregiver burden. Although treatment choice and dose-fractionation should always be tailored to the individual patient, single-fraction retreatment should be the default and standard option for most patients with uncomplicated, painful bone metastases.
Con argument
Bone metastases are common manifestations in many types of malignancies and may be associated with adverse consequences such as pain, pathological fractures, and neurological compromise. Radiotherapy is an effective treatment modality for palliation of painful bony metastases (5,8). With advances in systemic therapy, the average life expectancy of cancer patients has been prolonged (15). Consequently, increased numbers of patients survive to develop recurrent pain after previous radiation treatment (8). Repeat treatment of bony metastases has been shown to be feasible and effective in alleviating pain (17,31,32).
Radiation dose and fractionation are important considerations in the retreatment setting, and normal structure tolerances need to be considered in the context of previous irradiation. A variety of fractionation schedules were identified in a recent systematic review of retreatment (15). Our esteemed colleagues arguing for the pro position purported that a single 8 Gy should be the standard of care in the retreatment of uncomplicated bony metastases. However, we believe that while a single 8 Gy is an option, it has not been shown to be superior to fractionated regimens.
The legal definition of “standard of care” is “the caution that a reasonable person in similar circumstances would exercise in providing care to a patient” (33). There is no clear medical definition for this standard of care; however, it is widely considered to be the “conscientious, explicit, and judicious use of the current best evidence in making decisions about the care of individual patients” and the term should be used only if “supported by confirmatory RCTs or meta-analysis that are unchallenged”. We believe that there is insufficient evidence to support the statement that a single 8 Gy should be the sole standard fractionation for the retreatment of uncomplicated bone metastases.
To our knowledge, the only strong randomized evidence in this regard is NCIC SC.20 (8), a well-designed non-inferiority trial comparing a single 8 Gy fraction to 20 Gy fractionated radiotherapy. Patients with spinal cord compression, pathological fractures, or impending fractures were excluded. The primary endpoint was pain response at two months and secondary endpoints included quality of life and toxicity. The study failed to demonstrate non-inferiority for the primary endpoint on per-protocol analysis and the authors concluded that there may be trade-offs between efficacy and toxicity.
The reported increased “toxicities” in the fractionated group were: skin reddening at days 7 and 14, and GI symptoms at day 14 (lack of appetite, vomiting, and diarrhea). Unfortunately, details regarding treatment techniques and the use of steroids and anti-emetics were not reported. We must highlight that the only serious adverse event, myocardial infarction, was reported in a patient treated with a single 8 Gy whose heart was in the exit beam. Furthermore, the only quality of life domain which showed significant difference between the two groups (intention-to-treat analysis) was fatigue, in favor of the fractionated group (P=0.03).
The American Society for Radiation Oncology (ASTRO) evidence-based clinical practice guideline on palliative radiotherapy for bone metastases, published in the Red Journal, was the most-downloaded article in the year it was published (5,34). Although the guideline was published in 2011, predating the SC.20 study, this seminal paper does not recommend a specific dose and fractionation for retreatment. It does report higher rates of repeat treatment in patients with single-fraction (20%) compared to patients with fractionated courses (8%). In fact, this has been shown in multiple studies (35,36). In the Dutch Bone Metastasis study, there were almost four times as many retreatments observed in the single-fraction group (19,25). Interestingly, some patients seemed to respond more quickly to a fractionated retreatment schedule. On re-analysis of re-treated patients who previously were non-responders to a single 8 Gy, time to symptom response was 3 weeks for fractionated retreatment compared to 5 weeks for single-fraction retreatment. However, when considering all re-treated patients, there was no difference in time to response (25).
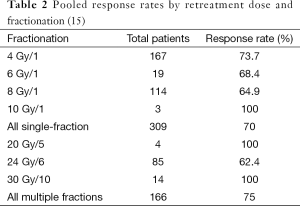
An in-depth systematic review of re-irradiation for painful bone metastases by Wong et al. (15) recommended re-irradiation for patients with ongoing pain regardless of the response to initial irradiation. Supplementary data summarizing the response rate stratified by retreatment dosage and fractionation was also provided. Some of these results are summarized in Table 2. There is some difficulty in this comparison due to the different measures of response rate; however, single-fraction retreatment regimens in this analysis are not clearly superior to the others.
Another randomized study demonstrated retreatment rates of 2% vs. 28% (P=0.001) in fractionated and single treatment groups, respectively (35). Given that a third course of radiotherapy may not be feasible or desirable, we would extrapolate that fractionated radiotherapy may potentially maximize the duration of pain response and minimize the risk of recurrent pain.
Lastly, while NCIC SC.20 demonstrated no statistically significant difference in the rates of in-field pathological fractures and spinal cord compression/cauda equina syndrome between the two groups, there is evidence that fractionated treatment may be advantageous in increasing remineralization. A randomized trial demonstrated significantly more bone recalcification in patients with fractionated treatment, compared to single-fraction (26). The authors concluded that fractionated treatment leads to “better stabilization”, which theoretically may lead to decreased rates of subsequent fractures. Similarly, in the Dutch Bone Metastasis Study, more pathological fractures were observed in the single-fraction group (19).
Overall, there does not seem to be consistent evidence regarding response rates, durability, and toxicity which would support holding one dose-fractionation scheme over another in the setting of retreatment of uncomplicated bone metastases. Though NCIC SC.20 suggested that 8 Gy in a single-fraction was non-inferior to a fractionated 20 Gy schedule, there are scenarios in which fractionation may be preferable. Therefore, both patient and tumour factors need to be considered when determining dose and fractionation in the retreatment setting. For example, fractionated treatment may be preferred in patients who have a longer life expectancy as it may result in a longer duration of response. Similarly, fractionated treatment may increase bone stabilization in weight-bearing regions and minimize the risk of pathological fractures. A patient who was treated with single-fraction radiotherapy as first-treatment, now needing retreatment, may prefer a different dose-fractionation, electing to receive multiple-fraction retreatment. Furthermore, in cases where local control is important (radioresistant tumours or oligometastatic disease), single-fraction 8 Gy treatment may be inappropriate. Thus, there are a variety of situations where single-fraction retreatment is not preferred: patient preference, long anticipated survival, oligometastatic disease, critical weight-bearing bone, or radioresistant histology. Therefore, a single-fraction of 8 Gy should not be considered the sole standard of care.
Discussion
Strauss and Thomas (33) indicated that there is no medical definition of standard of care. However, it was recommended that the term “standard of care” be used when there is support from confirmatory RCTs or meta-analysis that are unchallenged. Therefore, the term standard of care should be used with caution. The authors note, that the use of standard of care can be abused with the intention of providing impact and authenticity to a point of view that may be self-rewarding, without support from strong evidence.
Although the NCIC SC.20 trial concluded that, “In patients with painful bone metastases requiring repeat radiation therapy, treatment with 8 Gy in a single-fraction seems to be non-inferior and less toxic than 20 Gy in multiple fractions”, it should be noted that “the findings were not robust in a per-protocol analysis”. When choosing between single or multiple retreatment regimens, the authors concluded that trade-offs between efficacy and toxicity might exist. As such, single-fraction repeat radiation for painful bone metastases is an option as is multiple fractions. Both single and multiple fractions for re-irradiation of uncomplicated painful bone metastases are supported from this RCT.
In the absence of strong, randomized evidence demonstrating superiority of one treatment over another, other factors may be used by clinicians to decide between single and multiple fraction retreatments. However, reimbursement patterns should not be a factor in determining a dose-fractionation regimen of choice, even though remuneration is hypothesized to be a factor that influences variation in fractionation choice between countries (2). Instead, decisions regarding which fractionation regimen to use should depend on patient, tumour and treatment factors. In a patient with good performance status, quiescent systemic disease and in a patient who would not find it too burdensome to return for fractionated radiotherapy, multiple fractions for retreatment may be favoured with the possibility of more durable pain relief. However, these patients could also be re-treated with a single 8 Gy, which was found not to be inferior in the SC.20 trial.
On the other hand, if a patient has poor performance status and returning for multiple fractions would be a significant burden to the patient, single-fraction repeat radiotherapy would be favored. So, with respect to the debate statement: single-fraction treatment should be standard in the retreatment of uncomplicated bone metastases. The answer is yes, it is a standard of care. But multiple fractions are also a standard of care for these patients. The choice among the different fractionation schemes depends on an assessment of individual patient factors, tumour factors and unique patient circumstances.
Conclusions
Randomized trials have demonstrated feasibility, effectiveness, cost-effectiveness and convenience of single-fraction retreatment of painful bone metastases. At the same time, questions exist regarding non-inferiority of pain response and durability of pain relief with single-fraction retreatment. Without definitive data supporting one fractionation scheme over another, both 8 Gy in a single fraction or 20 Gy in multiple fractions are valid, standard options for patients. Choice of a dose-fractionation regimen should be made in discussion with the patient, their family, as well as oncologists and palliative care physicians in the circle of care. Factors important in this discussion include the patient’s performance status, projected life expectancy, social situation, and treatment philosophy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Chow E, Zeng L, Salvo N, et al. Update on the systematic review of palliative radiotherapy trials for bone metastases. Clin Oncol (R Coll Radiol) 2012;24:112-24. [PubMed]
- Fairchild A, Barnes E, Ghosh S, et al. International patterns of practice in palliative radiotherapy for painful bone metastases: evidence-based practice? Int J Radiat Oncol Biol Phys 2009;75:1501-10. [PubMed]
- Culleton S, Kwok S, Chow E. Radiotherapy for pain. Clin Oncol (R Coll Radiol) 2011;23:399-406. [PubMed]
- Zhu YJ. Palliative radiotherapy for painful bone metastases: short-course or long-course? Ann Palliat Med 2012;1:78-80. [PubMed]
- Lutz S, Berk L, Chang E, et al. Palliative radiotherapy for bone metastases: an ASTRO evidence-based guideline. Int J Radiat Oncol Biol Phys 2011;79:965-76. [PubMed]
- Hahn C, Kavanagh B, Bhatnagar A, et al. Choosing wisely: the American Society for Radiation Oncology’s top 5 list. Pract Radiat Oncol 2014;4:349-55. [PubMed]
- Sayed MM, Abdel-Wanis ME, El-Sayed MI. Single Fraction Compared with Multiple Fraction Re-Irradiations in Patients with Painful Bone Metastases. J Cancer Sci Ther 2013;5:089-93.
- Chow E, van der Linden YM, Roos D, et al. Single versus multiple fractions of repeat radiation for painful bone metastases: a randomised, controlled, non-inferiority trial. Lancet Oncol 2014;15:164-71. [PubMed]
- Detry MA, Lewis RJ. The intention-to-treat principle: how to assess the true effect of choosing a medical treatment. JAMA 2014;312:85-6. [PubMed]
- Mulla SM, Scott IA, Jackevicius CA, et al. How to use a noninferiority trial: users’ guides to the medical literature. JAMA 2012;308:2605-11. [PubMed]
- Wiens BL, Zhao W. The role of intention to treat in analysis of noninferiority studies. Clin Trials 2007;4:286-91. [PubMed]
- Oczkowski SJ. A clinician’s guide to the assessment and interpretation of noninferiority trials for novel therapies. Open Med 2014;8:e67-72. [PubMed]
- Townsley CA, Selby R, Siu LL. Systematic review of barriers to the recruitment of older patients with cancer onto clinical trials. J Clin Oncol 2005;23:3112-24. [PubMed]
- Jeremic B, Shibamoto Y, Igrutinovic I. Single 4 Gy re-irradiation for painful bone metastasis following single fraction radiotherapy. Radiother Oncol 1999;52:123-7. [PubMed]
- Wong E, Hoskin P, Bedard G, et al. Re-irradiation for painful bone metastases - a systematic review. Radiother Oncol 2014;110:61-70. [PubMed]
- Hayashi S, Hoshi H, Iida T. Reirradiation with local-field radiotherapy for painful bone metastases. Radiat Med 2002;20:231-6. [PubMed]
- Hernanz R, Montero A, Fernandez-Lizarbe E, et al. Retreatment with radiotherapy for symptomatic bone, brain or visceral metastases. Clin Transl Oncol 2013;15:72-8. [PubMed]
- Szumacher E, Llewellyn-Thomas H, Franssen E, et al. Treatment of bone metastases with palliative radiotherapy: patients’ treatment preferences. Int J Radiat Oncol Biol Phys 2005;61:1473-81. [PubMed]
- Steenland E, Leer JW, van Houwelingen H, et al. The effect of a single fraction compared to multiple fractions on painful bone metastases: a global analysis of the Dutch Bone Metastasis Study. Radiother Oncol 1999;52:101-9. [PubMed]
- Konski A, James J, Hartsell W, et al. Economic analysis of radiation therapy oncology group 97-14: multiple versus single fraction radiation treatment of patients with bone metastases. Am J Clin Oncol 2009;32:423-8. [PubMed]
- Pollicino CA, Turner SL, Roos DE, et al. Costing the components of pain management: analysis of Trans-Tasman Radiation Oncology Group trial (TROG 96.05): one versus five fractions for neuropathic bone pain. Radiother Oncol 2005;76:264-9. [PubMed]
- van den Hout WB, van der Linden YM, Steenland E, et al. Single- versus multiple-fraction radiotherapy in patients with painful bone metastases: cost-utility analysis based on a randomized trial. J Natl Cancer Inst 2003;95:222-9. [PubMed]
- Bedard G, Hoskin P, Chow E. Overall response rates to radiation therapy for patients with painful uncomplicated bone metastases undergoing initial treatment and retreatment. Radiother Oncol 2014;112:125-7. [PubMed]
- Hartsell WF, Scott CB, Bruner DW, et al. Randomized trial of short- versus long-course radiotherapy for palliation of painful bone metastases. J Natl Cancer Inst 2005;97:798-804. [PubMed]
- van der Linden YM, Lok JJ, Steenland E, et al. Single fraction radiotherapy is efficacious: a further analysis of the Dutch Bone Metastasis Study controlling for the influence of retreatment. Int J Radiat Oncol Biol Phys 2004;59:528-37. [PubMed]
- Koswig S, Budach V. Remineralization and pain relief in bone metastases after after different radiotherapy fractions (10 times 3 Gy vs. 1 time 8 Gy). A prospective study. Strahlenther Onkol 1999;175:500-8. [PubMed]
- Berenson J, Pflugmacher R, Jarzem P, et al. Balloon kyphoplasty versus non-surgical fracture management for treatment of painful vertebral body compression fractures in patients with cancer: a multicentre, randomised controlled trial. Lancet Oncol 2011;12:225-35. [PubMed]
- Expert Panel on Radiation Oncology-Bone Metastases, Lo SS, Lutz ST, et al. ACR Appropriateness Criteria ® spinal bone metastases. J Palliat Med 2013;16:9-19. [PubMed]
- Kim H, Rajagopalan MS, Beriwal S, et al. Cost-effectiveness analysis of single fraction of stereotactic body radiation therapy compared with single fraction of external beam radiation therapy for palliation of vertebral bone metastases. Int J Radiat Oncol Biol Phys 2015;91:556-63. [PubMed]
- Zhou M, Holden L, Lao N, et al. Accuracy of Clinicians’ Prediction of Survival and Prognostic Factors Indicative of Survival: a Systematic Review. Hong Kong J Radiol 2013;16:168-182.
- Mithal NP, Needham PR, Hoskin PJ. Retreatment with radiotherapy for painful bone metastases. Int J Radiat Oncol Biol Phys 1994;29:1011-4. [PubMed]
- Grosu AL, Andratschke N, Nieder C, et al. Retreatment of the spinal cord with palliative radiotherapy. Int J Radiat Oncol Biol Phys 2002;52:1288-92. [PubMed]
- Strauss DC, Thomas JM. What does the medical profession mean by “standard of care?”. J Clin Oncol 2009;27:e192-3. [PubMed]
- Zietman A. The red journal’s top 10 most downloaded articles of 2011. Int J Radiat Oncol Biol Phys 2012;83:1073-4. [PubMed]
- Foro Arnalot P, Fontanals AV, Galcerán JC, et al. Randomized clinical trial with two palliative radiotherapy regimens in painful bone metastases: 30 Gy in 10 fractions compared with 8 Gy in single fraction. Radiother Oncol 2008;89:150-5. [PubMed]
- 8 Gy single fraction radiotherapy for the treatment of metastatic skeletal pain: randomised comparison with a multifraction schedule over 12 months of patient follow-up. Bone Pain Trial Working Party. Radiother Oncol 1999;52:111-21. [PubMed]