
A systematic review and meta-analysis of the factors associating the willingness of Chinese community residents to receive COVID-19 vaccine
Highlight box
Key findings
• This study found the associated factors of the willingness of Chinese community residents to vaccinate COVID-19 vaccination. Male, community residents who think COVID-19 vaccine is effective, community residents who think COVID-19 vaccine is safe, and community residents who think COVID-19 infection risk is high are more likely to take COVID-19 vaccination.
What is known and what is new?
• Some factors affect the willingness of Chinese community residents to take COVID-19 vaccination.
• Male, community residents who think COVID-19 vaccine is effective, community residents who think COVID-19 vaccine is safe, and community residents who think COVID-19 infection risk is high are more likely to take COVID-19 vaccination.
What is the implication, and what should change now?
• Vaccination strategies need to be formulated according to the gender of community residents, propaganda of vaccination information, and dissemination of epidemic information.
Introduction
Coronavirus disease of 2019 (COVID-19) is a highly infectious disease that has become one of the leading causes of death worldwide and has posed a serious challenge to global public health in recent decades. Pneumonia caused by COVID-19 is the most common high-risk symptom, which can cause fever, cough and shortness of breath in humans. Mortality from COVID-19 is also associated with its complications, such as acute respiratory distress syndrome, septic shock and sepsis. At present, “prevention is better than treatment” is the consensus on this disease (1). As one of the effective means to prevent COVID-19, vaccination of people around the world is the best way to deal with this epidemic. After a period of vaccination, people’s enthusiasm for COVID-19 vaccination decreased with the temporary control of the epidemic and the occurrence of adverse reactions to COVID-19 vaccine (2). Recently, a study has provided factors associated with the uptake of COVID-19 vaccines, such as the correlation between vaccination and the race of the people and the recommendation of medical institutions, but these factors are incomplete and difficult to classify due to their small sample size (3). Due to different vaccination policies in different regions, the COVID-19 vaccination situation varies from region to region. An increasing number of studies have shown that there is a correlation between the prevalence of COVID-19 vaccination in different provinces in China and people’s willingness to be vaccinated (4-15), but the willingness of residents to be vaccinated is not consistent across regions, which may be due to complex sociodemographics. Based on this, this study mainly conducted a meta-analysis on the associated factors of willingness to get COVID-19 vaccination in available studies, in order to evaluate the associated factors affecting people’s willingness to vaccinate against COVID-19. We present the following article in accordance with the MOOSE reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-22-1099/rc).
Methods
Search strategy
The Chinese databases of China National Knowledge Infrastructure (CNKI), Chinese Biomedical Literature (CBM), Wanfang, and VIP and the English databases of PubMed, Web of Science, and Cochrane Library were searched by computer to collect the relevant original data on the factors affecting the COVID-19 vaccination willingness of Chinese community residents. The English search terms included the following: COVID-19 vaccines, COVID-19, COVID-19 virus vaccines, including factors, related factors, willingness, acceptability, acceptance, China, and so on; the Chinese key search words included the following: novel coronavirus pneumonia, COVID-19, novel coronavirus, coronavirus, vaccine, vaccination, associated factors, related factors, and willingness.
Literature screening and exclusion criteria
Screening criteria
We included studies met the following criteria: (I) Chinese community residents; (II) vaccination willingness with accurate figures odds ratio (OR) and 95% confidence interval (CI); (III) cross-sectional studies (IV) article language was English and/or Chinese; (V) the participants were Chinese community residents over 16 years old.
Exclusion criteria
(I) Literature unrelated to the purpose of the study; (II) duplicate literature; (III) literature for which valid data could not be obtained.
Data extraction
Three researchers extracted the data and checked it repeatedly. In the case of disagreement, an authoritative tutor was consulted for judgment. The content of data extraction mainly included the following: the first author, publication time, survey area, sample size, quality evaluation score, associated factors, and demographic characteristics, COVID-19 vaccination rates, OR values and 95% CIs for multiple logistic regression analysis. The primary outcome was to aggregate associated factors related to the willingness of Chinese community residents to receive COVID-19 vaccination.
Methodological quality evaluation
The quality assessment was performed using the Newcastle-Ottawa scale (NOS) (16). The scores range from 0 to 9 (≥6 as high quality). There are 11 items in the evaluation, including cohort representability, selection of non-exposed cohort, ascertainment of exposure, outcome not present at baseline, comparability of cohorts for important factors, comparability of cohorts for other variables, assessment of outcome, follow-up long enough for outcome to occur, adequacy of follow-up.
Statistical analysis
The software packages of RevMan 5.3 (The Cochrane Collaboration, The Nordic Cochrane Center, Copenhagen, Denmark), Stata (Stata Corp., College Station, TX, USA), and R (The R Foundation for Statistical Computing, Vienna, Austria) were used for statistical analysis. (I) According to the requirements of this research analysis, the data of the included documents were extracted and integrated. (II) The OR value and 95% CI of the associated factors on the willingness of Chinese community residents to receive COVID-19 vaccination were used to describe the effect amount, and then a forest map was made. (III) Heterogeneity check refers to the I2 value and P value of the included literature. When I2≤50% and P>0.1, no statistical heterogeneity was indicated, and the fixed effects model was used to merge the data; if there was statistical heterogeneity, we first analyzed the reasons for the heterogeneity, and then used sensitivity analysis, subgroup analysis, and other methods to re-process the data. If there is heterogeneity remained after this treatment, the random effects model was used to merge the data. (IV) Statistical significance was indicated when P<0.05. (V) Egger tests were used to detect the publication bias of the included literature. (VI) We used sensitivity analyses for covariate factors to test for effects on pooled results.
Results
Basic information of literature inclusion and flow chart of literature screening
According to the search strategy, a total of 1,152 documents that met the requirements were retrieved. After the initial screening, according to the inclusion and exclusion criteria of this meta-analysis, a total of 12 documents (4-15) were included for the final meta-analysis, including 7 Chinese documents and 5 English documents. The flow chart of document inclusion is shown in Figure 1. A total of 29,278 patients were involved. The data and quality evaluation of the included literature are shown in Table 1.

Table 1
| No. | First author | Ref. | Year | Study type | Research factors | Survey area | Sample size | Quality evaluation score |
|---|---|---|---|---|---|---|---|---|
| 1 | Lu Zhang | (4) | 2021 | Cross sectional study | Awareness of effectiveness and safety of COVID-19 vaccine | Sichuan (Zigong) | 1,703 | 5 |
| 2 | Qiangqiang Fu | (5) | 2022 | Cross sectional study | Education background, COVID-19 infection risk awareness, vaccine safety and effectiveness awareness | Anhui (Wuhu); Zhejiang (Hangzhou); Shanghai (Jinshan) | 2,859 | 5 |
| 3 | Mingfang Xiao | (6) | 2021 | Cross sectional study | Education, awareness of COVID-19 vaccine effectiveness and adverse reaction | Ganzhou | 1,860 | 7 |
| 4 | Suhang Song | (7) | 2022 | Cross sectional study | Education background, COVID-19 infection risk awareness | Nanjing, Chizhou | 2,241 | 7 |
| 5 | Jinhua Pan | (8) | 2022 | Cross sectional study | Gender and safety awareness of vaccines | Shanghai; Zhejiang; Qinghai | 2,169 | 7 |
| 6 | Yinliang Tan | (9) | 2022 | Cross sectional study | Risk perception of COVID-19 infection | Shanghai; Chengdu; Fuzhou | 8,990 | 7 |
| 7 | Yu Ma | (10) | 2022 | Cross sectional study | Awareness of safety and adverse reactions of vaccines | Changsha | 1,076 | 6 |
| 8 | Da Huo | (11) | 2022 | Cross sectional study | COVID-19 infection risk awareness, vaccine safety awareness, and convenience of vaccination | Beijing | 406 | 5 |
| 9 | Musha Chen | (12) | 2021 | Cross sectional study | Awareness of effectiveness of COVID-19 vaccine, awareness of COVID-19 infection risk, gender | Guangdong; Hunan; Hebei; Neimenggu; Fujian; Henan; Jiangsu; Anhui; Sichuan; Shandong; Hubei | 3,195 | 7 |
| 10 | Jie Shao | (13) | 2022 | Cross sectional study | Adverse reaction cognition of COVID-19 vaccine | Shanghai | 2,570 | 5 |
| 11 | Yujun Zhang | (14) | 2022 | Cross sectional study | Gender, awareness of COVID-19 vaccine effectiveness | Wulumuqi | 335 | 7 |
| 12 | Huilin Shi | (15) | 2022 | Cross sectional study | Risk perception of COVID-19 infection | Lanzhou, Shanghai, Wuhan | 1,874 | 7 |
COVID-19, coronavirus disease of 2019.
Systematic evaluation results of associated factors of COVID-19 vaccination willingness of Chinese community residents
The heterogeneity test of the research results included in the literature was used as the judgment standard, and the fixed effects model (I2≤50%) or the random effects model (I2>50%) was selected. The results showed that the effectiveness and safety awareness of COVID-19 vaccine, the risk awareness of COVID-19, gender were the associated factors of COVID-19 vaccination uptake among Chinese community residents (P<0.05) (see Table 2). Among the included literature, 11 articles covered the willingness rate of COVID-19 vaccination (willing to be vaccinated includes already vaccinated and willing to be vaccinated). The results showed that there was a large heterogeneity (P<0.1 in Q test, I2=99.52%), so a random effects model was used for meta-analysis. The willingness rate of Chinese community residents to receive COVID-19 vaccination was 80% (95% CI: 71% to 87%) (Figure 2).
Table 2
| Research factors | Case group | Control group | Number of references | Heterogeneity test | OR (95% CI) | Combined effect size test | ||
|---|---|---|---|---|---|---|---|---|
| I2 (%) | P value | Z | P value | |||||
| Gender | Male | Female | Pan (8), Chen (12), Zhang (14) | 15 | 0.31 | 1.48 (1.23–1.76) | 4.27 | <0.0001 |
| Awareness of vaccine effectiveness | Think the vaccine is effective | Think the vaccine ineffective | Zhang (4), Fu (5), Xiao (6), Chen (12), Zhang (14) | 60 | 0.004 | 4.10 (3.08–5.46) | 9.64 | <0.00001 |
| Vaccine safety awareness | Think the vaccine is safe | Think the vaccine is not safe | Zhang (4), Fu (5), Ma (10), Huo (11) | 75 | 0.08 | 1.82 (1.42–2.33) | 4.72 | <0.00001 |
| Risk perception of COVID-19 infection | High cognitive level | Low cognitive level | Fu (5), Song (7), Tan (9), Huo (11), Chen (12), Shi (15) | 86 | <0.00001 | 1.65 (1.33–2.04) | 4.64 | <0.00001 |
COVID-19, coronavirus disease of 2019; OR, odds ratio; CI, confidence interval.
Sensitivity analysis and publication bias
Sensitivity analysis of the included associated factors showed that the OR values of the two models were close to the 95% CI, indicating that the stability of this study is good. According to the number of included documents, the Egger test was used. The results were greater than 0.05, indicating that there is no bias in this study (Table 3).
Table 3
| Influence factor | Effect model OR (95% CI) | Bias test | ||
|---|---|---|---|---|
| Fixed effect | Random effect | P value | ||
| Gender factor | 1.48 (1.23, 1.76) | 1.49 (1.22, 1.82) | 0.105 (Egger test) | |
| Cognitive factors of vaccine effectiveness | 4.38 (3.77, 5.09) | 4.10 (3.08, 5.46) | 0.403 (Egger test) | |
| Cognitive factors of vaccine safety | 1.67 (1.52, 1.83) | 1.82 (1.42, 2.33) | 0.301 (Egger test) | |
| Cognitive factors of COVID-19 infection risk | 1.53 (1.43, 1.64) | 1.65 (1.33, 2.04) | 0.369 (Egger test) | |
COVID-19, coronavirus disease of 2019; OR, odds ratio; CI, confidence interval.
Discussion
A total of 14 articles were included in this meta-analysis, among which 8 were of medium quality and 6 were of high quality. The meta-analysis results of different effect models were stable, and the Egger test showed no publication bias. In addition, the analysis results of this study showed heterogeneity in the cognition of the effectiveness and safety of COVID-19 vaccine, the cognition of the risk of COVID-19 infection. Therefore, random effect models were selected for meta-analysis. There was no statistical heterogeneity in gender factors, so fixed effects models were selected for meta-analysis. To sum up, gender factors (Table 4, Figure 3), the effectiveness (Table 5, Figure 4) and safety (Table 6, Figure 5) awareness of COVID-19 vaccine, and the risk awareness of COVID-19 (Table 7, Figure 6) are the associated factors of COVID-19 vaccination willingness of Chinese community residents.
Table 4
| Author | OR | ORLL | ORUL |
|---|---|---|---|
| Jinhua Pan 2022 | 1.49 | 1.12 | 1.98 |
| Musha Chen 2021 | 1.35 | 1.05 | 1.74 |
| Yujun Zhang 2022 | 2.16 | 1.25 | 3.732 |
Gender factor I2=15%, fixed effects model was used for analysis. OR, odds ratio; ORLL, odds ratio lower limit; ORUL, odds ratio upper limit.
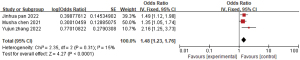
Table 5
| Author | OR | ORLL | ORUL |
|---|---|---|---|
| Musha Chen 2021 | 4.545 | 3.704 | 5.556 |
| Qiangqiang Fu 2022 | 6.317 | 4.481 | 8.907 |
| Yujun Zhang 2022 | 2.935 | 1.413 | 6.1 |
| Lu Zhang 2021 | 3.13 | 2.17 | 4.54 |
| Mingfang Xiao 2021 | 2.88 | 1.39 | 5.99 |
OR, odds ratio; ORLL, odds ratio lower limit; ORUL, odds ratio upper limit.

Table 6
| Author | OR | ORLL | ORUL |
|---|---|---|---|
| Jinhua Pan 2022 | 7.14 | 5.00 | 10.00 |
| Qiangqiang Fu 2022 | 2.36 | 1.838 | 3.03 |
| Lu Zhang 2021 | 1.449 | 1.053 | 2.041 |
| Da Huo 2022 | 2.188 | 1.493 | 3.206 |
| Yu Ma 2022 | 1.541 | 1.377 | 1.727 |
OR, odds ratio; ORLL, odds ratio lower limit; ORUL, odds ratio upper limit.

Table 7
| Author | OR | ORLL | ORUL |
|---|---|---|---|
| Musha Chen 2021 | 1.887 | 1.667 | 2.174 |
| Suhang Song 2022 | 1.950 | 1.119 | 3.398 |
| Qiangqiang Fu 2022 | 1.498 | 1.17 | 1.918 |
| Da Huo 2022 | 1.587 | 1.202 | 2.096 |
| Huilin Shi 2022 | 2.046 | 1.685 | 2.495 |
| yinliang Tan 2022 | 1.24 | 1.12 | 1.37 |
COVID-19, coronavirus disease of 2019; OR, odds ratio; ORLL, odds ratio lower limit; ORUL, odds ratio upper limit.

This study shows that the willingness of male residents in Chinese communities to be vaccinated is 1.48 times that of female residents in Chinese communities. The gender difference reflected by this vaccination may be related to the higher mortality rate of COVID-19 in men than in women, which is consistent with previous research results in China and internationally (17-19); a study (20) has reported that in the COVID-19 pandemic, women generally implement non-drug intervention measures such as wearing masks and washing hands frequently, so it can be summarized that men tend to vaccinate and women tend to use non-drug intervention to prevent COVID-19.
In addition, the Strategic Advisory Group of Experts on Immunization (SAGE; WHO immunization strategy committee), established in 2012, put forward the “3C” model that affects vaccination according to the complex factors behind the hesitancy of vaccination: (I) trust in the effectiveness, safety, and adverse reactions of vaccines; trust in the reliability and ability of medical personnel (confidence dimension); (II) low awareness of disease infection risk or belief that vaccination is not necessary preventive measures (complacency dimension); (III) physical accessibility, affordability and willingness to pay, geographical accessibility, understanding ability (language and health literacy) and attractiveness of immunization services (convenience dimension) required by vaccination. The model shows that the implementation of individual vaccination behavior is closely related to the “3C” factor (21). However, the effectiveness, safety cognition of COVID-19 vaccine, and the risk cognition of COVID-19 infection in the results of this study belong to the confidence dimension, the complacency dimension, which again demonstrates the scientific robustness and credibility of the results of this study.
Efficacy, safety cognition of COVID-19 vaccine
This study shows that Chinese community residents who believe that COVID-19 vaccine can effectively prevent COVID-19, think that COVID-19 vaccine will not cause disease are more willing to receive COVID-19 vaccine.
In this study, the willingness of Chinese community residents not worried about vaccine safety was 1.82 times higher than those worried about vaccine safety. According to the research and investigation (22), novel coronavirus vaccine is divided into virus inactivated vaccine, adenovirus vector vaccine, and recombinant subunit vaccine. The adverse reactions caused by the vaccine of the Sinopharm group and Beijing Kexing vaccine used in China are fever and pain at the injection point. The adverse reactions of adenovirus vector (kweisa) vaccine are fever, fatigue, and muscle pain. Regardless of which vaccine is selected, the safety and adverse reactions are mild and moderate. In general (3), inactivated vaccine and recombinant protein vaccine have stable structure, high safety, and need to be vaccinated multiple times; RNA vaccine is a new technology with high vaccination cost and good effectiveness. Therefore, the Chinese community residents who do not know about the safety of the vaccine should more widely disseminate the vaccine information to them to eliminate their unnecessary concerns.
The cognitive factors of COVID-19 infection risk were included in this study. There were many articles (n=6) and there was medium and high heterogeneity (I2=86%), so subgroup analysis was conducted based on the year of literature survey. The results showed that the survey year affected the results of meta-analysis. Among them, the two groups of survey sites covered 20 provinces, cities, and autonomous regions in China, and there was no heterogeneity in the group in 2020 (I2=40%). There was heterogeneity within the group in 2021 (I2=60%). Finally, the heterogeneity between groups was high, which reflects that with the passage of time and the efforts of the Chinese government to control the epidemic situation, the epidemic situation is slowly controlled throughout the country, and the cognition of Chinese community residents on the risk of COVID-19 infection is changing year by year. Research has shown that (23,24) during the outbreak of COVID-19, people generally pay attention to their own health status and infection risk; during the COVID-19 abatement period, when social order returns to work and production, people often pay attention to the information such as “health code” and “isolation” brought by the population flow across provinces and cities; during the normalization prevention and control period, people pay attention to vaccination and other information to prevent the next wave of epidemic. This study can show that the change of public concerns is regular, and relevant departments can provide positive information to the public to affect the public’s mood and then affect the public’s behavior intention.
Conclusions
Our meta-analysis indicated that male, community residents who think COVID-19 vaccine is effective, community residents who think COVID-19 vaccine is safe, and community residents who think COVID-19 infection risk is high are important predictors to take COVID-19 vaccination. In addition, the willingness rate of Chinese community residents to receive COVID-19 vaccination was 80%.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the MOOSE reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-22-1099/rc
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-22-1099/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rehman SU, Rehman SU, Yoo HH. COVID-19 challenges and its therapeutics. Biomed Pharmacother 2021;142:112015. [Crossref] [PubMed]
- Barranco R, Rocca G, Molinelli A, et al. Controversies and Challenges of Mass Vaccination against SARS-CoV-2 in Italy: Medico-Legal Perspectives and Considerations. Healthcare (Basel) 2021;9:1163. [Crossref] [PubMed]
- Reiter PL, Pennell ML, Katz ML. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine 2020;38:6500-7. [Crossref] [PubMed]
- Zhang L, Hong P, Nan Y, et al. Analysis of novel coronavirus vaccination willingness and influencing factors of Zigong residents. Chinese Journal of Preventive Medicine 2021;22:862-7.
- Fu Q, Li J. analysis on the vaccination willingness and influencing factors of adults with novel coronavirus pneumonia in some areas of the Yangtze River Delta. China Primary Health Care 2022;36:64-7.
- Xiao M, Yu A, Luo W, et al. Analysis of novel coronavirus vaccination willingness and influencing factors of Ganzhou residents -- Based on the questionnaire survey in the central urban area of Ganzhou. Jiangxi Medicine 2021;56:2388-94.
- Song S, Zang S, Gong L, et al. Willingness and uptake of the COVID-19 testing and vaccination in urban China during the low-risk period: a cross-sectional study. BMC Public Health 2022;22:556. [Crossref] [PubMed]
- Pan J, A K, Liu Z, et al. Factors That Impact Acceptance of COVID-19 Vaccination in Different Community-Dwelling Populations in China. Vaccines (Basel) 2022;10:91. [Crossref] [PubMed]
- Tan Y, Xie Z, Qian Y, et al. Accelerate the process of getting vaccinated: factors associated with consideration of and accessibility to COVID-19 vaccination in metropolises of China. BMC Public Health 2022;22:1182. [Crossref] [PubMed]
- Ma Y, Fan R, Yan S, et al. Investigation on the willingness and influencing factors of novel coronavirus vaccination among different occupational groups. Practical Preventive Medicine 2022;29:281-5.
- Huo D, Zhou T, Wang C, et al. Study on vaccine hesitation and related influencing factors before the marketing of novel coronavirus pneumonia vaccine. Practical Preventive Medicine 2022;29:27-31.
- Chen M, Li Y, Chen J, et al. An online survey of the attitude and willingness of Chinese adults to receive COVID-19 vaccination. Hum Vaccin Immunother 2021;17:2279-88. [Crossref] [PubMed]
- Shao J, Tang L, Huang Q, et al. Analysis on the influencing factors of covid-19 vaccination among residents in Pudong New Area of Shanghai. Preventive Medicine Forum 2022;28:405-10.
- Zhang Y, Zhu L, Diliyar W, et al. Analysis of influencing factors and hesitation reasons of novel coronavirus vaccination intention. Henan Journal of Preventive Medicine 2022;33:343-6.
- Shi H, Wu Q, Chen Z, et al. Study on the willingness and influencing factors of COVID-19 vaccination among the general population and medical workers in China. Practical Preventive Medicine 2022;29:671-7.
- Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603-5. [Crossref] [PubMed]
- Galbadage T, Peterson BM, Awada J, et al. Systematic Review and Meta-Analysis of Sex-Specific COVID-19 Clinical Outcomes. Front Med (Lausanne) 2020;7:348. [Crossref] [PubMed]
- Azizi Z, Shiba Y, Alipour P, et al. Importance of sex and gender factors for COVID-19 infection and hospitalisation: a sex-stratified analysis using machine learning in UK Biobank data. BMJ Open 2022;12:e050450. [Crossref] [PubMed]
- Wu G, Deng T, Zhang M, et al. Investigation on attitude towards covid-19 vaccination and its psychosocial factors. Chinese Journal of Clinical Psychology 2021;29:622-5. [PubMed]
- Li Z, Sun X. Research on the influencing factors of public vaccine hesitation based on health belief model. Modern Preventive Medicine 2021;48:4331-4334+4376.
- MacDonald NESAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015;33:4161-4. [Crossref] [PubMed]
- Zheng N, Zhao M, Tian X, et al. Current situation and trend of global research and development of novel coronavirus vaccine and therapeutic drugs. Chinese Journal of New Drugs 2022;31:69-76.
- Dong C, Shen Q, Guo Y, et al. Analysis on the information demand of the public during the COVID-19 epidemic. China Public Health 2022;38:800-3.
- Yang K, Yang C, Zhu Q. Research on public information demand and crisis management of Public Health Emergencies Based on social media. Information Theory and Practice 2021;44:59-68.



