Superior mesenteric artery (SMA) syndrome: an unusual cause of intestinal obstruction in palliative care
Introduction
Superior mesenteric artery (SMA) syndrome is an uncommon cause of intestinal obstruction with a reported incidence of 0.1−0.3% (1). SMA syndrome is caused by compression of the third, or transverse portion of the duodenum between the aorta and the superior mesenteric artery resulting in chronic, intermittent, or acute complete or partial duodenal obstruction (2). This condition is typically caused by an angle of 6°−25° between the abdominal aorta and the SMA, in comparison to the normal range of 38°−56°. In addition, the aorto-mesenteric distance in SMA syndrome is 2−8 mm, as opposed to the typical 10−20 (3). Other possible mechanisms of SMA syndrome include peritoneal adhesions, a low origin of superior mesenteric artery and a high insertion of the duodenum at the ligament of Treitz (4).
Case presentation
A 68-year-old Chinese man was admitted to palliative care unit in March 2016 for poor intake, abdominal discomfort and psychosocial support (5). He has background history of congestive heart failure due to severe coronary artery disease and opted for conservative management. He has multiple cardiovascular risk factors including hypertension, hyperlipidemia and atrial fibrillation.
Upon arrival to our palliative unit, he presented with 1 day history of diffuse abdominal cramps and constipations for 3 days. He has bilateral lower limb swelling and dyspnea on mild to moderate exertion for 3 days. On examination of the patient, he was noted to be in distress with markedly distended abdomen and diffuse abdominal tenderness. Bowel sounds were inactive. His vital signs were normal.
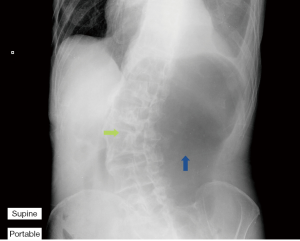
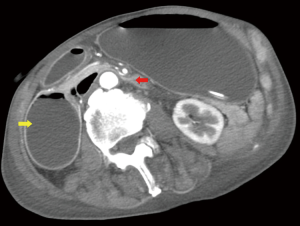
Urgent abdominal X-ray revealed grossly distended stomach (Figure 1). A provisional diagnosis of upper intestinal obstruction was made. A computer tomography (CT) scan was arranged (Figure 2). Grossly distended stomach with dilated esophagus is noted. The duodenum is dilated with transition zone seen at D3, at a narrowing between the SMA and the aorta. The aorto-mesenteric angle measures 20 degree and the aorto-mesenteric distance measures 4 mm. Features are suggestive of SMA syndrome.
Surgeon was consulted and suggested conservative management for his intestinal obstruction due to high operative risk. Nasogastric tube was inserted via endoscopic guidance for decompression and aspiration of gastric fluid. And he was started on parental nutrition and then transferred back to our unit. Subsequently he was able to tolerate tube feeding and partial oral feeding. Nasogastric tube was then removed because of most of his symptoms subsided. However, the patient developed profuse vomiting afterwards leading to aspiration pneumonia and finally succumbed.
Discussion
Common differential diagnosis in palliative patient with intestinal obstruction includes mechanical obstruction (e.g., malignant tumors), paralytic ileus, electrolyte imbalance, constipation and drug induced.
In our patient who has strong cardiovascular risk factors and atrial fibrillation, bowel ischemia has to be considered. SMA syndrome typically occurs in patient with low body mass index (BMI), malnourished, history of significant weight loss and spine deformities such as scoliosis and exaggerated lumbar lordosis (4). These factors could all precipitate narrowing of the aorto-mesenteric angle. Our patient has a remote history of poliomyelitis during childhood leading to scoliosis. In his Abdominal X-ray (Figure 1), there is marked convexity towards the right side, which could be a contributing factor in this patient. Furthermore, he has prolonged hospitalization due to recurrent heart failure symptoms and pleural effusion, which also contributed to his recent weight loss.
Treatment in SMA syndrome mainly aims to alleviate the symptoms of obstruction and to avoid nutritional depletion (4). Parental or enteral nutrition administration was shown to have positive effect in terms of disease outcomes, leading to weight gain (6). The patient should be monitored closely for change in weight; both enteral and parental nutrition may be needed. Gradual introduction of oral feeding should be initiated as patient’s obstructive symptoms begin to subside.
Our patient died shortly after removal of nasogastric tube due to recurrence of obstruction and aspiration. It illustrated the importance to monitor signs and symptoms of intestinal obstruction as SMA syndrome is prone to recur (7). Insertion of nasogastric tube can reduce discomfort due to abdominal distension and lower the risk of aspiration.
This case also highlighted the presence of non-malignant/organ failure patients in palliative care ward. As such, palliative care physicians should be aware of SMA syndrome as a differential diagnosis for intestinal obstruction and proper care should be given for this group of patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient's next of kin for publication of this Case report.
References
- Shiu JR, Chao HC, Luo CC, et al. Clinical and nutritional outcomes in children with idiopathic superior mesenteric artery syndrome. J Pediatr Gastroenterol Nutr 2010;51:177-82. [Crossref] [PubMed]
- Gerasimidis T, George F. Superior mesenteric artery syndrome. Wilkie syndrome. Dig Surg 2009;26:213-4. [Crossref] [PubMed]
- Shetty AK, Schmidt-Sommerfeld E, Haymon ML, et al. Radiological case of the month. Denouement and discussion: superior mesenteric artery syndrome. Arch Pediatr Adolesc Med 1999;153:303-4. [Crossref] [PubMed]
- Merrett ND, Wilson RB, Cosman P, et al. Superior mesenteric artery syndrome: diagnosis and treatment strategies. J Gastrointest Surg 2009;13:287-92. [Crossref] [PubMed]
- Chan KY, Yip T, Yap DY, et al. Enhanced psychosocial support for caregiver burden for patients with chronic kidney failure choosing not to be treated by dialysis or transplantation: a pilot randomized controlled trial. Am J Kidney Dis 2016;67:585-92. [Crossref] [PubMed]
- Lippl F, Hannig C, Weiss W, et al. Superior mesenteric artery syndrome: diagnosis and treatment from the gastroenterologist's view. J Gastroenterol 2002;37:640-3. [Crossref] [PubMed]
- Raissi B, Taylor BM, Taves DH. Recurrent superior mesenteric artery (Wilkie's) syndrome: a case report. Can J Surg 1996;39:410-6. [PubMed]


