
To feel or not to feel: a scoping review and mixed-methods meta-synthesis of moral distress among surgeons
Highlight box
Key findings
• Despite the absence of a uniformly applied definition of moral distress, the emerging body of literature identifies various sources of moral distress among surgeons.
What is known and what is new?
• Surgeons may be particularly vulnerable to moral distress given their unique relationship with patients. Ultimately, the emotional consequences of moral distress may affect surgeon well-being and adversely impact the ability of surgeons to care for their patients.
• Research investigating moral distress in healthcare workers is increasingly common. However, assessment of moral distress among surgeons is limited.
What is the implication, and what should change now?
• A better understanding of the complex interplay of factors may help facilitate a detailed investigation into this critical problem and may potentially facilitate targeted interventions that protect surgeons from psychological harm and promote better patient outcomes.
Introduction
The British Medical Association (BMA) recently defined moral distress as “the psychological unease generated where professionals identify an ethically correct action to take but are constrained in their ability to take that action… (and) by witnessing the moral transgression by others” (1). Sustained or severe moral distress may transgress into psychological harm and impaired function, sequelae along a continuum known as moral injury (1). Surgeons may be particularly vulnerable to moral distress given their unique relationship with patients, which requires healing through harm, embracing a high degree of accountability for their actions, and forming a profoundly intimate and physical connection with patients. Ultimately, the emotional consequences of moral distress may affect surgeon well-being and adversely impact the ability of surgeons to care for their patients.
Research investigating moral distress in healthcare workers is increasingly common. However, assessment of moral distress among surgeons is limited. The majority of studies that include a surgeon cohort tend to generalize their findings to all healthcare providers, and even fewer focus on surgeons and the field of surgery specifically (2-9). The invasive nature of a surgeon’s craft and the responsibility surgeons have over patients place this group at unique risk for moral distress. The few studies assessing surgeons reveal variability in the prevalence of moral distress. Maftei et al. recently reported moral distress was present among 48% of neurosurgeons in their study (10). However, other studies show variability in the prevalence of distress among surgeons and it is unclear how burdensome the distress is in this cohort compared to other healthcare professionals (7,8). To date, there is no summative assessment of the predisposing attributes and external factors that lead to moral distress and its sequelae among surgeons despite increasing attention to this phenomenon in both the scientific literature and the media.
In this context, we sought to review the existing literature regarding the known and suspected factors contributing to moral distress among surgeons. Our objective was to synthesize current literature and provide a thematic summary of these factors based on the social ecological model (SEM), which facilitates the conceptualization of health broadly. Here, a summative understanding of the complex interplay of factors at the SEM levels (e.g., individual, interpersonal, environmental, community, and policy) help facilitate a detailed investigation into this critical problem and may potentially facilitate targeted interventions that protect surgeons from psychological harm and promote better patient outcomes. We present the following article in accordance with the PRISMA-ScR reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-22-916/rc).
Methods
Review design, data sources, and search strategy
We engaged a research librarian to initiate a search of the published literature within EBSCOhost PsycINFO, Elsevier EMBASE, Ovid MEDLINE, and Wiley Cochrane Central Register of Controlled Trials Library from January 1, 2009 to February 21, 2022 with guidelines established by Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRIMSA) guidelines (11). We selected 2009 given the sharp increase in the discussion surrounding moral distress that began around this time (12). Search terms included data-specific combinations of index terms and text words: surgeon, surgery, moral, distress, stress, damage, injury, and harm. Appendix 1 provides reproducible searches for all databases.
Inclusion and exclusion criteria
We developed inclusion criteria for relevant articles using the PRISMA schema (13). All surgeon subspecialties were included (e.g., breast, cardiothoracic, colorectal, general, neurologic, orthopedic, otolaryngology/head and neck, pediatric, plastic, surgical oncology, transplant, trauma, urologic, and vascular). Only peer-reviewed studies based on primary data examining moral distress and/or moral injury among surgeons were included. We excluded reviews or guidelines, book chapters, and opinion pieces or letters. We excluded studies from the grey literature (e.g., abstract or conference proceedings) due to concerns regarding quality of data and the inability to verify peer review. Finally, we excluded studies without surgeon representation and non-English studies. While moral distress was the focus of this review, moral injury was included as an inclusion term given the many definitions of what constitutes moral distress and the frequent conflation of the two terms.
Study selection and data extraction
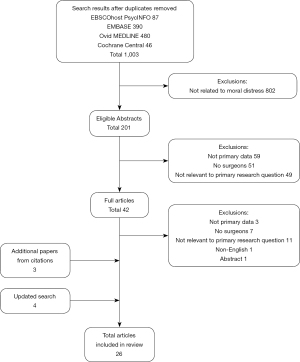
Article selection occurred in three phases. First, 1,003 titles and abstracts were screened using the inclusion and exclusion criteria. Consensus discussions regularly took place to resolve disagreements. We excluded 802 total abstracts, yielding 201 eligible abstracts. In the second phase, we excluded an additional 159 articles that did not include primary data (n=59), did not explicitly include surgeons (n=51), or otherwise did not fulfill inclusion criteria (n=49).
In the third phase (in-depth review), we excluded an additional 23 articles and then performed a hand-search of the references from the 19 remaining articles, which yielded a total of 22 articles for full review. Finally, we included the search terms “ethics” and “ethical” to our searches based on expert review and performed an updated search (September 29, 2022), which yielded an additional four articles for full review (Figure 1).
We used a modified data abstraction tool, which has been previously used for systematic review and meta-synthesis studies (14-17). Detailed data, including sample population, methods, results, and conclusions were extracted from each article and independently assessed by at least two reviewers (CF, IVW) for methodologic quality. Consensus discussions were utilized to resolve disagreements and final adjudication was made by the lead author.
Assessment of methodologic quality and risk of bias
We assessed methodologic quality according to predefined criteria for reliability, validity, and quality (18). To evaluate quantitative studies, we assessed selection and minimization of attrition bias, minimization of confounding and measurement bias, appropriateness of statistical tests, and whether the results supported the conclusions. To evaluate qualitative studies, we used explicit sampling strategy and description of data analysis, statement of final themes with definitions, validation of findings, and strategies to achieve consensus among coders (14,16,17). No study deviated from these established methodologic quality metrics.
Data analysis
A mixed-methods meta-synthesis was employed for this study due to: (I) the heterogeneity of methodology and outcome measures of the included studies; and (II) the ability to synthesize and provide overviews of both quantitative and qualitative studies based on themes, interventions, and results (19,20). We incorporated both deductive and inductive components in our thematic analysis. Thematic analysis was used to organize and synthesize data into coherent themes using a five-step approach: (I) in-depth reading of each article by at minimum two independent reviewers (familiarization with the data); (II) independent coding of each article; (III) search for themes related to moral distress among surgeons; (IV) group discussion to review, compare, and contrast themes for further refinement; and (V) develop a final set of themes based on consensus regarding definitions and predetermined strategies for adjudication of any discrepancies. These codes were deductively sorted into the SEM’s five domains. Themes were coded to best fit when they could be categorized under multiple domains. The SEM is a conceptual framework introduced in the 1970s to facilitate the understanding of human development. The model has previously been used to better understand patient health-related behaviors and the process of forming individual surgeon identity (21-23). The SEM posits that personal development and subsequent behavior is a function of individual, interpersonal, environmental, community and policy factors. The SEM enables us to examine how particular factors, and the interplay between factors, influence the formation of moral distress in individual surgeons while identifying shared factors that all surgeons experience. All authors reviewed the categorization of the themes and agreed on the final results of the data analysis (14,17).
Results
Review of the literature revealed variation in the definition of moral distress. Most studies refer to Jameton’s traditional definition of moral distress, where distress results from an individual’s inability to pursue what is ethically right due to institutional or hierarchical constraints (7,8,24-31). One study adopted a definition of moral distress in-line with the BMA definition, indirectly defining moral distress to include Jameton’s original definition while also capturing the distress caused by witnessing perceived moral wrongs (32). Another study expanded on Jameton’s original definition, noting that distress may occur following a moral decision as individuals struggle with the sequelae of forgoing choices justified by alternative ethical principles, implying distress caused by ethical “opportunity costs” (33). Several studies discussing moral distress did not include any explicit definition of moral distress (2-6,9,34,35).
Moral distress was found to be a complex process, influenced by factors that exist at multiple levels of the healthcare system. Factors affecting moral distress were identified through literature review and categorized into the five SEM domains to capture this complexity: individual, interpersonal, environmental, community, and policy. By organizing the drivers of moral distress into these domains, we highlight the breadth of sources from which these factors originate and draw attention to existing knowledge gaps (Table 1).
Table 1
| Source | Participants | Study design | Findings | SEM themes | ||||
|---|---|---|---|---|---|---|---|---|
| Individual | Interpersonal | Environment | Community | Policy | ||||
| Abbasi et al. | 399 physicians practicing in hospitals affiliated with a medical university | Cross-sectional survey | The frequency of moral distress was 1.24±0.63, the intensity of moral distress was 2.14±0.8, and the composite score of moral distress was 2.94±2.38 using the Moral Distress Scale-Revised. Moral distress was associated with age, experience, specialty, and participation in medical ethics training | × | × | × | ||
| Aljehani et al. | 234 surgical residents | Cross-sectional survey | Approximately half (50.4%) of respondents reported being deployed to cover staff shortages in ICUs and EDs during the COVID-19 pandemic. Anxiety was significantly associated with male gender (P=0.055), level of training (P=0.002), deployment to cover ICUs (P=0.05), testing positive for COVID-19 (P=0.054), and having an infected family member (P=0.004) | × | × | |||
| Arslan et al. | 190 members of the International Pediatric Transplant Association | Cross sectional | Among the 190 professionals working in pediatric transplantation, 38% respondents experienced ethical issues. Surgeons, relative to physicians, were more likely to encounter ethical issues. European clinicians were more likely to experience ethical issues compared to North American clinicians. Ethical issues most commonly were associated with psychosocial evaluation and donor follow up care | × | × | × | ||
| Austin et al. | 329 health care providers from a single institution | Cross-sectional survey | Significant correlations between secondary traumatic stress, burnout, and moral distress (as measured by the Moral Distress Survey-Revised) were found. High moral distress was associated with intentions to leave. Highest levels of moral distress were due to being compelled to provide care that seems ineffective and working with a critical care patient load >50% | × | × | × | ||
| Bender et al. | 205 nurses and 124 providers at two academic hospitals | Cross-sectional survey | Nurses reported greater moral distress when using comfort care order sets compared to providers (40.5% vs. 19.4%, P=0.002). The majority of respondents felt that comfort care was generally started too late in a patient’s course | × | ||||
| Bleicher et al. | 21 nurses, 25 physicians and residents from a single, academic SICU | Cross-sectional survey (n=46) followed by semi-structured interviews (n=17) | Both nurses and physicians report high levels of moral distress (MMD-HP 132±63.5 and 121.7±64.7 respectively). The most frequent root cause of moral distress was delivery of aggressive care perceived to be futile | × | × | × | × | × |
| Bruce et al. | 29 ICU team members at a single institution | Semi-structured interviews focused on key sources of moral distress in the context of team-based models | All respondents reported experiencing moral distress. A key source of distress across all healthcare disciplines was intrateam discordance. Two situations when intrateam discordance created to moral distress: (I) situations involving initiation or maintenance of non-beneficial life-sustaining treatments and (II) situations involving lack of full disclosure about interventions | × | ||||
| Chiu et al. | 45 pediatric surgery trainees | Cross-sectional survey | 59% of respondents felt they had received adequate training in bioethics to handle ethical issues pertaining to the care of critically ill children. Moral conflicts were resolved through direct discussions with medical staff, family, or friends | × | × | × | ||
| Fagerdahl et al. | 12 operating room team members | Semi-structured interviews focused on experiences during the COVID-19 pandemic | Participants described working hard but felt their efforts were not enough according to their moral ideals | × | × | × | × | |
| Fainstad et al. | 101 female residents, 18 of which were from surgical subspecialities | Randomized clinical trial. Intervention arm offered 6-month coaching program to reduce burnout, moral injury and imposter syndrome | Among the intervention group, emotional exhaustion decreased, impostor syndrome was less frequent, and self-compassion was greater. There was no difference in depersonalization, professional accomplishment or moral injury scores | |||||
| Hines et al. | 96 healthcare workers | Longitudinal Study | Moral injury remained stable over the time period during the COVID-19 pandemic. Distress was not affected by any baseline occupational or resiliency factors. Poor sleep at baseline was predictive of more distress | × | ||||
| Khattab et al. | 781 spine surgeons | Cross-sectional survey | Those most affected by COVID-19 included older surgeons, orthopedic spine surgeons, and those who work in the private sector. Lower psychological stress was associated with the availability of N95 masks and disposable eye protectors or face shields | × | × | |||
| Knifed et al. | 28 surgery, otolaryngology, and obstetrics and gynecology residents at a single institution | Semi-structured interviews focused on ethical concerns and distress as a result of being a trainee | Residents encountered ethical dilemmas leading to moral angst during their training and expressed the need to feel safe to discuss these events openly | × | × | |||
| Lievrouw et al. | 17 doctors and 18 nurses working in three different oncology hospital settings | Semi-structured interviews to gain insight into the meaning-making strategies of professionals and their way of dealing with moral distress | Moral distress lingered if accompanied by emotional distress. Doctors reported a mainly rational coping style while nurses tended to focus on feelings and experiences. Coping with moral distress was influenced by personal or work-related experiences and perceived team culture | × | ||||
| Mackel et al. | 173 neurosurgeons | Cross-sectional | 47.7% reported significant moral distress in the past year with the most common cause originating from managing critical patients lacking a clear treatment plan and the most intense cause being from families pressuring surgeons to perform futile surgery. Moral distress led to 10% of surgeons leaving a position and 26.6% contemplating doing so | × | × | |||
| Maftei et al. | 114 physicians | Cross-sectional survey | Nearly 50% of respondents reported high levels of potentially morally injurious events. No significant differences were noted in exposures between COVID-19 and non-COVID-19 units, specialization, experience level, age, or gender | × | ||||
| Miljeteig et al. | 1,606 nurses and physicians | Cross-sectional survey | 67% of respondents experienced priority-setting dilemmas in the previous two weeks. Those directly involved in COVID-19 care, were redeployed or worked in psychiatry/addition medicine experienced it more often. Moral distress levels were generally low (2.9 on a 0–10 scale) but higher among those redeployed, managers, and working in psychiatry/addition medicine | × | × | |||
| Miranda et al. | 62 neurosurgery residents from the American Association of Neurological Surgeons/Congress of Neurological Surgeons Joint Section on Neurotrauma and Critical Care email listserv | Cross-sectional survey | Most respondents reported no explicit teaching on: explaining the risks and benefits of intubation and ventilation (69%), formulating prognoses in neurocritical care (60%), or leading family meetings (69%). Most (87%) reported moral distress, agreeing that they “participated in operations and worried whether surgery aligned with patient goals” | × | × | × | × | × |
| Peetz et al., 2022 | 11 trauma surgeons from Level 1 or 2 trauma centers in Tennessee | Semi-structured interviews focused on ethical dilemmas and ethical constraints focused on organ preservation among lethally injured patients | All participants felt a primacy of obligation to the patient. Most (n=9) felt the moral obligation to consider organ preservation was secondary/balancing whereas a few (n=2) felt it was irrelevant/immoral. All participants expressed some resource limitation and all conveyed clear moral agency when the goal was to save a patient’s life but this was less clear when resuscitating for organ preservation | × | × | × | × | × |
| Peetz et al., 2021 | 31 trauma surgeons | Cross-sectional | Many respondents encounter resuscitations where the goal is to preserve the potential for organ transplantation. Notable range in complexity of interventions used in order to preserve organs (from intubation to thoracotomy). Respecting the dying process and future organ quality were most frequent concerns when deciding whether to stop resuscitation | × | × | × | ||
| Pololi et al. | 1,708 residents in general surgery, internal medicine, and pediatrics at 14 academic health systems | Cross-sectional survey | Vitality, capturing the joy and meaningfulness of work, and measured using the C-Change Resident Survey, varied widely with scores ranging from 17–71%. 50% of variance was attributed to factors such as work-life integration, relationships/inclusion/trust, institutional/program support, respect, values alignment, and ethical/moral distress | × | × | × | ||
| Redman et al. | 16 pediatric otolaryngology faculty and fellows at a single tertiary institution | Cross-sectional survey | Overall Moral Distress Survey-Revised score was 40 [14–94], which is lower than prior reports of pediatric surgeons and pediatric intensivists, and similar to pediatric oncologists. Fellows had significantly higher levels of moral distress than faculty (69 vs. 26, P<0.05) | × | × | × | ||
| Rushton et al. | 595 healthcare workers from a research network | Cross-sectional survey | Overall prevalence of moral injury was 32.4% with nurses reporting the highest occurrence. Moral injury was associated with ethical concerns, religious affiliation, and years of experience. Moral resilience was a moderator of moral injury | × | × | × | × | |
| Spilg et al. | 962 healthcare workers | Cross-sectional survey | Respondents working with patients with COVID-19 showed significantly more severe moral distress, anxiety, and depression symptoms (F ≥5.5, P≤0.02), and a higher proportion screened positive for mental disorders (Chi-squared >9.1, P=0.002) compared to healthcare workers who were not. Moral resilience moderated the relationship between exposure to morally distressing events and moral distress compared (P<0.001) | × | × | |||
| Zimmerman et al., 2020 | 2,161 members of the American College of Surgeons | Cross-sectional survey | High moral distress was associated with the decision to offer surgery that was influenced by the belief that pursuing surgery gives the patient or family time to cope (OR =1.44, 95% CI: 1.02–2.03) | × | × | × | × | × |
| Zimmerman et al., 2021 | Trauma clinicians from three academic institutions | Interventional study consisting of focus groups (n=48) and pre/post intervention surveys (n=122) | Moral distress was higher among nurses than physicians and overall, did not change after the communication intervention. There was less distress regarding “witnessing providers giving false hope” by physicians after the intervention | × | ||||
SEM, social ecological model; ICU, intensive care unit; ED, emergency department; COVID-19, coronavirus disease 2019; SICU, surgical intensive care unit; MMD-HP, Measures of Moral Distress for Healthcare Professionals; OR, odds ratio; CI, confidence interval.
Individual
In 19 articles, individual factors were considered in relation to their association with moral distress among surgeons (2-6,8,10,25,27-37). In some instances, this was in connection to demographic characteristics such as gender (2,8,30,31), years in practice (2,29,31-33,36), and the impact of being in a leadership or supervisory position (30). While greater experience level was generally associated with decreased moral distress, working in a leadership or supervisory role predisposed individuals to distress, placing the traditional correlation of seniority and acquiring increasing responsibility in direct conflict with each other as it relates to moral distress. In other instances, moral distress was a result of more personal factors such as the religious views of the provider (32), personal beliefs on organ donation (6), and acting or witnessing actions that betrayed their morals (10,29). Other studies focused on aspects that were connected to mental health, including the emotional weight of watching patients die alone (32), coping mechanisms in place for managing moral distress (10), baseline moral injury (28), and the need to have time to reflect and process events and experiences that are distressing (29). Other individual factors included the perception of a knowledge deficit about disease processes or how to conduct an operation (3,5,27,34) and concerns of spreading infection to self/other patients/family (e.g., COVID-19) (2,27,32). Of the studies identifying individual factors associated with moral distress, only two considered a cohort exclusively of surgeons.
Interpersonal
Interpersonal factors were also explored in relation to the moral distress among surgeons (3,5-9,25-27,31-39). In some instances, these interpersonal factors arose in connection to the care provided, such as having unclear or inconsistent goals of care (7,25,34,37), discordance among and between teams or families (3,5,8,26,38), disruptions to the doctor-patient relationship (32), providing life prolonging intervention for terminally ill patients (3,6-9,25,33,34,37,39) and pressure from others to drive care (7,8,25,26,33,34,37). In studies assessing surgeons, interpersonal factors’ impact on moral distress appear to differ based on surgeon roles. For example, Redman et al. demonstrated that fellows had higher moral distress scores among items such as “following family’s wishes to continue life support even though I believe it’s not in the best interest of the child” and “initiate extensive life-saving actions when I think they only prolong death” when compared to attending surgeons (7). In other instances, the focus was on the surgical team, such as the impacts of being overshadowed by colleagues (27), level of support from co-workers (31) and working alongside inadequately trained colleagues (7,33,36). While still others focused on the impacts of leadership, such as feeling like they were being abandoned by superiors (27), the impact of following ethically discordant directions (3,7,25,32-34), and repercussions for voicing safety concerns (32). Poor communication, both among team members (3,7,33) and between the medical team and family (25,32,34), was also repeatedly identified to be an instigating factor for moral distress.
Environment
Practice environment was found to influence moral distress among surgeons (2-4,6-8,24,25,27,30,32-36,38,39). While some studies focused on the type of setting (e.g., intensive care units, Veterans Affairs hospitals, private practice) (2,8,33) others focused on the influence of subspecialty (33), and differences based on patient population (e.g., pediatric vs. adult) (36,38). Austin et al.’s assessment of moral distress reveals high rates among surgery and medical subspecialty groups compared to primary care among physician and nursing cohorts, highlighting the increased burden practitioners in procedure-based and specialized fields may face. They also report higher rates of moral distress among surgeons whose patient census contained more patients in a critical care setting compared to surgeons who did not. In other instances, studies focused on the impact of limited medical resources (6,32,36,39), including, but not limited to personal protective equipment especially during the COVID-19 pandemic (27). Other studies focused on the impacts of logistical and administration issues, including the difficulty surrounding redeployment (27,30,32,33), the impacts of a demanding patient workload (3,25,27,36), the lack of provider continuity (33,36) and perceived persistence of stressful situations (27). Difficulties inherent to certain practice settings were a clear source of distress. For example, the intensive care unit (ICU) setting is more prone to exposing providers to patients whose care requires navigating established sources of moral distress, including the need to provide non-beneficial interventions (7,8,25,33), manage patients with unclear prognostication (34) and manage comfort care (24).
Community
Community level factors have also been found to influence moral distress among surgeons (6,8,25,34,38,39). For this analysis, “community” was used as an umbrella term to capture the values and identities among surgeons as a population and American society as a whole. At the surgeon level, encountering false hope in the clinical setting and wrestling with the surgeon mentality of being a “fixer” was cited as contributing to distress (25,34). Surgeons also encountered moral distress when confronting controversial values in American culture, such as providing life-extending interventions to facilitate family’s emotional closure (6,8) and extending life to facilitate organ donation (6,39). Organ transplantation generated unique drivers of distress at the community level, with several studies describing distress arising from allocation (maximizing utility vs. equity, duty to the donor vs. the population) and providing a dignified death to a donor (38,39).
Policy
Several papers acknowledged the impact of medicolegal concerns on moral distress among surgeons (6-8,25,27,32,34). Policy level considerations included discussion on excessive documentation resulting in impaired ability to care for patients (25), financial considerations (e.g., hospital billing, conflicts of interest, insurance coverage) (6,34), limited family access to loved ones during the pandemic (32), frequently changing COVID-19 guidelines (27), the legal ramifications regarding organ donation (6) and not offering surgery (7,8) or pursuing care for fear of legal repercussions. For example, Redmann et al. document that surgical fellows are particularly susceptible to distress when put in positions where they have to “follow the family’s wishes for the child’s care when I do not agree with them, but do so because of fears of a lawsuit” (7).
Protective factors
Several studies explicitly identified traits associated with decreased moral distress among surgeons. Some of these traits were intrinsic to the individual, these included traits such as seniority (7,36), having a religion/belief system (32), being male (31), being older (31), getting enough sleep (31), and having no existing mental disorder (31). Other sources of reducing moral distress were extrinsic and encompassed both sources acting on the individual or the individual being involved in a difficult situation. These extrinsic sources included having ethics training (29,36), early access to palliative care (25), having more frequent discussion about goals of care (25), as well as experiencing team collaboration (27,29) and colleague support (28,31).
Discussion
This is the first scoping review to examine moral distress among surgeons and the underlying factors contributing to moral distress among this cohort. This analysis identified 26 manuscripts since 2009 that assessed moral distress among healthcare workers, with only ten studies focused primarily on surgeons. The definition of moral distress has evolved since first described by Andrew Jameton in 1984 as the “experience of knowing the right thing to do while being in a situation in which it is nearly impossible to do it” (40). While moral distress has been documented widely in nursing literature, it has only recently been described among physicians, pharmacists, and social workers. Consequently, there is variability in how distress is defined among the studies we assessed. The terms “moral distress” and “moral injury” are increasingly common terms in healthcare literature, which may be attributed to a trend in academic interest or more worrisome, as Jameton recently asserted, it “may also reflect an increase in the frequency, intensity, or extent of distress among health professionals” (41). To facilitate future research with clear objectives on this topic, we favor the definitions described by the BMA, which sufficiently capture the triggers leading to moral distress and its sequelae while being broad enough to capture consternating sources beyond an individual’s sole action.
Critical to the definition of moral distress is an individual’s identification of an “ethically correct action”. The literature reveals many factors that lead to distress; however, this work also includes factors that do not necessarily stem from ethical discordance and do not fit this explicit definition of “moral distress”. While we included factors such as “spread of infection to others”, “communication issues among teams”, and “watching patients die alone”, these may not be issues of ethical discordance but rather complex stressors in a demanding job that contribute to burnout (1). We propose a model to capture the differences between burnout, moral distress, and moral injury. Starting with an occupational stressor, an individual may internalize this stressor by experiencing burnout, distress and/or injury (Figure 2). If a stressor has a moral component, the individual is at risk of experiencing moral distress and/or moral injury. If no moral component exists, they risk experiencing burnout alone. In some cases, a moral stressor may generate burnout, moral distress, and moral injury; in others, a moral stressor may not generate burnout but could cause moral distress and injury. Critical to experiencing moral distress is grappling with an issue of ethical discordance. A unique circumstance may arise when an individual is so overcome by burnout that they are unable or unwilling to contemplate the issue of ethical discordance and subsequently do not experience moral distress. Ultimately, existing risk and protective factors influence how an individual internalizes a stressor. These factors result from prior life experiences, including previous exposure to stressors and the introspective reflection individuals may experience in the coping process following burnout, moral distress and moral injury. Coping may manifest in various positive ways, including but not limited to discovering enlightenment and personal growth, avoidance of future stressors, or development of moral resilience. Alternatively, individuals may fail to cope and reflect, putting them at risk of experiencing burnout, distress and injury from future stressors, or developing ambivalence toward their experiences. This coping process has previously been described as an intellectual response to a stressor (42). Suppose an individual intrinsically possesses sufficient protective factors or has acquired these through the process of prior coping responses. In that case, they may never experience burnout, distress or injury following exposure to a stressor. Our model emphasizes that future research in moral distress will benefit from explicitly describing how the stressors under investigation have a moral component in order to differentiate these from non-moral sources of occupational stress. In other words, is what is currently being described in the literature psychological distress rather than moral distress (41)?
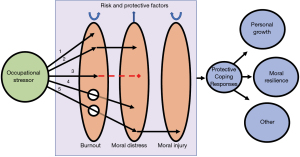
Despite the absence of a uniformly applied definition of moral distress, the emerging body of literature identifies various sources of moral distress among surgeons. Given the diversity of factors contributing to distress, we categorized the causes according to the SEM. This model captures the drivers of moral distress at the individual, interpersonal, environmental, community, and policy levels (Figure 3). Categorization using the SEM facilitates rapid and precise identification of moral distress sources; this “by-level” categorization allows stakeholders with predominant influence at these levels to identify where they can potentially act to moderate moral distress. For example, medical educators might focus on individual and interpersonal contributors to moral distress by teaching surgical residents resilience strategies to better cope with traumatizing events, mediate team conflict, and guide goals of care discussions.
The surgeon-patient relationship is marked by unique features separating this specialty from the rest of healthcare, including healing through harm, a profoundly intimate physical relationship, and an inherently high degree of accountability to patients. Most of the reviewed literature identifies drivers of moral distress among many providers, including surgeons. While we identified a handful of surgeon-specific studies, the moral distress literature studying this cohort is still sparse. This presents a significant knowledge deficit given the unique nature of the surgeon-patient relationship and the context of surgery. Additional investigation is needed to understand how the unique role of a surgeon generates specialty-specific sources of moral distress. This future research might also consider the different sources of moral distress that present through surgical training into autonomous practice. There is emerging evidence that these sources are different, which is not surprising given the change in surgeon responsibility and surgeon-patient dynamics that occur over time (7). Ultimately, addressing moral distress among surgeons requires addressing the sources that are context-specific, this requires addressing the drivers of distress when they occur at different points in what is a long, laborious training process and demanding career.
Moral distress research should aim to identify what factors most influence distress and transgression to moral injury and ultimately, what remedies are most effective at addressing these powerful drivers. Our analysis revealed several factors that provide some protective utility from moral distress. However, many of these factors are intrinsic traits unamenable to intervention (e.g., age, sex, race/ethnicity), with a few offering the potential for intervention (e.g., team collaboration, ethics training). Early work assessing the impact of interventions on moral distress at the individual level has yet to show a statistically significant impact (9,43). While such individual-level interventions are critical to mitigating moral distress, investigators might consider drawing from “burnout” literature, which has demonstrated that interventions to reduce rates of burnout are most successful when directed by the organization rather than individual-level interventions (44-46).
This scoping review has several limitations. First, there is no universal consensus on the definition of “moral distress”. While we favor the BMA association of the term, we considered studies that use other definitions of distress. We selected a definition of moral distress that was intentionally broad to be as inclusive as possible during our literature search. To reduce publication and search bias in this scoping review, we searched four large databases with the assistance of a research librarian. We performed a hand search of all the references from the included studies. We also included sources of moral distress that these studies identified but which may not fit a strict definition of moral distress as they lack a true moral stressor. Several studies identified various factors leading to moral distress but failed to assess if these were statistically significant drivers of distress. When confronted with the list of factors these studies presented, we elected to include all factors that were enumerated. For studies that identified statistically significant drivers of distress, we listed only those drivers. Understanding the prevalence of moral distress among surgeons was also clouded by the numerous definitions of moral distress and moral injury and the multiple instruments used to study their presence. Of the studies we assessed, 11 different established survey instruments and 14 self-created instruments were used to assess moral distress/injury (47-58).
Conclusions
This is the first scoping review to categorize the sources of moral distress among surgeons. Our findings demonstrate notable variation in the definition of moral distress among studies and a general lack of investigation into the sources of moral distress among surgeons. Categorizing the known and suspected factors leading to moral distress among surgeons demonstrates that distress arises at several different “levels”, which are well categorized according to the SEM model. There is a critical need to understand the drivers of distress among surgeons better. This knowledge can potentially reduce moral distress among surgeons as sources are intervened upon and mitigated. It is simply not enough to understand “intrinsic” surgeon factors that predispose this group to distress when there are likely actionable steps that can be taken at an institutional and national level to promote surgeon well-being and improve patient care.
Acknowledgments
Funding: The authors acknowledge their support from the following: MAM and SK are supported through Agency for Healthcare Research and Quality (No. T32HS000053). PAS is supported by the Agency for Healthcare Research and Quality (No. K08 HS026772-01A1).
Footnote
Reporting Checklist: The authors have completed the PRISMA-ScR reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-22-916/rc
Peer Review File: Available at https://apm.amegroups.com/article/view/10.21037/apm-22-916/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-22-916/coif). PAS serves as an unpaid editorial board member of Annals of Palliative Medicine from February 2022 to January 2024. The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- British Medical Association. Moral distress and moral injury recognising and tackling it for UK doctors. 2021.
- Aljehani YM, Othman SA, Telmesani NK, et al. Stress and psychological resilience among general surgery residents during COVID-19 pandemic. Saudi Med J 2020;41:1344-9. [Crossref] [PubMed]
- Chiu PP, Hilliard RI, Azzie G, et al. Experience of moral distress among pediatric surgery trainees. J Pediatr Surg 2008;43:986-93. [Crossref] [PubMed]
- Khattab MF, Kannan TMA, Morsi A, et al. The short-term impact of COVID-19 pandemic on spine surgeons: a cross-sectional global study. Eur Spine J 2020;29:1806-12. [Crossref] [PubMed]
- Knifed E, Goyal A, Bernstein M. Moral angst for surgical residents: a qualitative study. Am J Surg 2010;199:571-6. [Crossref] [PubMed]
- Peetz A, Kuzemchak M, Hammack C, et al. Trauma Surgeons' Perceptions of Resuscitating Lethally Injured Patients for Organ Preservation. Am Surg 2022;88:663-7. [Crossref] [PubMed]
- Redmann AJ, Smith M, Benscoter D, et al. Moral distress in pediatric otolaryngology: A pilot study. Int J Pediatr Otorhinolaryngol 2020;136:110138. [Crossref] [PubMed]
- Zimmermann CJ, Taylor LJ, Tucholka JL, et al. The Association Between Factors Promoting Nonbeneficial Surgery and Moral Distress: A National Survey of Surgeons. Ann Surg 2022;276:94-100. [Crossref] [PubMed]
- Zimmermann CJ, Zelenski AB, Buffington A, et al. Best case/worst case for the trauma ICU: Development and pilot testing of a communication tool for older adults with traumatic injury. J Trauma Acute Care Surg 2021;91:542-51. [Crossref] [PubMed]
- Maftei A, Holman AC. The prevalence of exposure to potentially morally injurious events among physicians during the COVID-19 pandemic. Eur J Psychotraumatol 2021;12:1898791. [Crossref] [PubMed]
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372: [PubMed]
- Lamiani G, Borghi L, Argentero P. When healthcare professionals cannot do the right thing: A systematic review of moral distress and its correlates. J Health Psychol 2017;22:51-67. [Crossref] [PubMed]
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 2009;62:e1-34. [Crossref] [PubMed]
- Dossett LA, Hudson JN, Morris AM, et al. The primary care provider (PCP)-cancer specialist relationship: A systematic review and mixed-methods meta-synthesis. CA Cancer J Clin 2017;67:156-69. [Crossref] [PubMed]
- Guetterman T, Creswell JW, Kuckartz U. Using joint displays and MAXQDA software to represent the results of mixed methods research. Use of visual displays in research and testing: Coding, interpreting, and reporting data. 2015:145-75.
- Mouch CA, Regenbogen SE, Revels SL, et al. The quality of surgical care in safety net hospitals: a systematic review. Surgery 2014;155:826-38. [Crossref] [PubMed]
- Suwanabol PA, Kanters AE, Reichstein AC, et al. Characterizing the Role of U.S. Surgeons in the Provision of Palliative Care: A Systematic Review and Mixed-Methods Meta-Synthesis. J Pain Symptom Manage 2018;55:1196-215.e5. [Crossref] [PubMed]
- Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000;283:2008-12. [Crossref] [PubMed]
- NHS Health Development Agency. Integrative approaches to qualitative and quantitative evidence. London: Health Development Agency, 2004.
- Sandelowski M, Voils CI, Barroso J. Defining and Designing Mixed Research Synthesis Studies. Res Sch 2006;13:29. [PubMed]
- Golden SD, Earp JA. Social ecological approaches to individuals and their contexts: twenty years of health education & behavior health promotion interventions. Health Educ Behav 2012;39:364-72. [Crossref] [PubMed]
- Nyambe A, Van Hal G, Kampen JK. Screening and vaccination as determined by the Social Ecological Model and the Theory of Triadic Influence: a systematic review. BMC Public Health 2016;16:1166. [Crossref] [PubMed]
- Rivard SJ, Vitous CA, De Roo AC, et al. "The captain of the ship." A qualitative investigation of surgeon identity formation. Am J Surg 2022;224:284-91. [Crossref] [PubMed]
- Bender MA, Andrilla CHA, Sharma RK, et al. Moral Distress and Attitudes About Timing Related to Comfort Care for Hospitalized Patients: A Survey of Inpatient Providers and Nurses. Am J Hosp Palliat Care 2019;36:967-73. [Crossref] [PubMed]
- Bleicher J, Place A, Schoenhals S, et al. Drivers of Moral Distress in Surgical Intensive Care Providers: A Mixed Methods Study. J Surg Res 2021;266:292-9. [Crossref] [PubMed]
- Bruce CR, Miller SM, Zimmerman JL. A qualitative study exploring moral distress in the ICU team: the importance of unit functionality and intrateam dynamics. Crit Care Med 2015;43:823-31. [Crossref] [PubMed]
- Fagerdahl AM, Torbjörnsson E, Gustavsson M, et al. Moral Distress Among Operating Room Personnel During the COVID-19 Pandemic: A Qualitative Study. J Surg Res 2022;273:110-8. [Crossref] [PubMed]
- Hines SE, Chin KH, Glick DR, et al. Trends in Moral Injury, Distress, and Resilience Factors among Healthcare Workers at the Beginning of the COVID-19 Pandemic. Int J Environ Res Public Health 2021;18:488. [Crossref] [PubMed]
- Lievrouw A, Vanheule S, Deveugele M, et al. Coping With Moral Distress in Oncology Practice: Nurse and Physician Strategies. Oncol Nurs Forum 2016;43:505-12. [Crossref] [PubMed]
- Miljeteig I, Forthun I, Hufthammer KO, et al. Priority-setting dilemmas, moral distress and support experienced by nurses and physicians in the early phase of the COVID-19 pandemic in Norway. Nurs Ethics 2021;28:66-81. [Crossref] [PubMed]
- Spilg EG, Rushton CH, Phillips JL, et al. The new frontline: exploring the links between moral distress, moral resilience and mental health in healthcare workers during the COVID-19 pandemic. BMC Psychiatry 2022;22:19. [Crossref] [PubMed]
- Rushton CH, Thomas TA, Antonsdottir IM, et al. Moral Injury and Moral Resilience in Health Care Workers during COVID-19 Pandemic. J Palliat Med 2022;25:712-9. [Crossref] [PubMed]
- Austin CL, Saylor R, Finley PJ. Moral distress in physicians and nurses: Impact on professional quality of life and turnover. Psychol Trauma 2017;9:399-406. [Crossref] [PubMed]
- Miranda SP, Schaefer KG, Vates GE, et al. Palliative Care and Communication Training in Neurosurgery Residency: Results of a Trainee Survey. J Surg Educ 2019;76:1691-702. [Crossref] [PubMed]
- Pololi LH, Evans AT, Civian JT, et al. Resident Vitality in 34 Programs at 14 Academic Health Systems: Insights for Educating Physicians and Surgeons for the Future. J Surg Educ 2018;75:1441-51. [Crossref] [PubMed]
- Abbasi M, Nejadsarvari N, Kiani M, et al. Moral distress in physicians practicing in hospitals affiliated to medical sciences universities. Iran Red Crescent Med J 2014;16:e18797. [Crossref] [PubMed]
- Mackel CE, Alterman RL, Buss MK, et al. Moral Distress and Moral Injury Among Attending Neurosurgeons: A National Survey. Neurosurgery 2022;91:59-65. [Crossref] [PubMed]
- Arslan Z, Hennessy J, McCulloch MI, et al. Experience of ethical dilemmas among professionals working in pediatric transplantation: An international survey. Pediatr Transplant 2022;26:e14331. [Crossref] [PubMed]
- Peetz AB, Kuzemchak MD, Streams JR, et al. Regional ethics of surgeon resuscitation for organ transplantation after lethal injury. Surgery 2021;169:1532-5. [Crossref] [PubMed]
- Jameton A. Nursing practice: the ethical issues. Prentice-Hall series in the philosophy of medicine. Englewood Cliffs, NJ, USA: Prentice-Hall, 1984.
- Jameton A. What Moral Distress in Nursing History Could Suggest about the Future of Health Care. AMA J Ethics 2017;19:617-28. [Crossref] [PubMed]
- Bamdad MC, Vitous CA, Rivard SJ, et al. "You Remember Those Days"-A Qualitative Study of Resident Surgeon Responses to Complications and Deaths. J Surg Educ 2022;79:452-62. [Crossref] [PubMed]
- Fainstad T, Mann A, Suresh K, et al. Effect of a Novel Online Group-Coaching Program to Reduce Burnout in Female Resident Physicians: A Randomized Clinical Trial. JAMA Netw Open 2022;5:e2210752. [Crossref] [PubMed]
- Panagioti M, Panagopoulou E, Bower P, et al. Controlled Interventions to Reduce Burnout in Physicians: A Systematic Review and Meta-analysis. JAMA Intern Med 2017;177:195-205. [Crossref] [PubMed]
- Vitous CA, Dinh DQ, Jafri SM, et al. Optimizing Surgeon Well-Being: A Review and Synthesis of Best Practices. Ann Surg Open 2021;2:e029. [Crossref] [PubMed]
- Shanafelt TD. Physician Well-being 2.0: Where Are We and Where Are We Going? Mayo Clin Proc 2021;96:2682-93. [Crossref] [PubMed]
- Andrews G, Slade T. Interpreting scores on the Kessler Psychological Distress Scale (K10). Aust N Z J Public Health 2001;25:494-7. [Crossref] [PubMed]
- Hamric AB, Borchers CT, Epstein EG. Development and testing of an instrument to measure moral distress in healthcare professionals. AJOB Primary Research 2012;3:1-9. [Crossref]
- Flanagan JC. The critical incident technique. Psychol Bull 1954;51:327-58. [Crossref] [PubMed]
- Corley MC, Elswick RK, Gorman M, et al. Development and evaluation of a moral distress scale. J Adv Nurs 2001;33:250-6. [Crossref] [PubMed]
- Epstein EG, Whitehead PB, Prompahakul C, et al. Enhancing Understanding of Moral Distress: The Measure of Moral Distress for Health Care Professionals. AJOB Empir Bioeth 2019;10:113-24. [Crossref] [PubMed]
- Stamm BH. The professional quality of life scale: Compassion satisfaction, burnout & compassion fatigue/secondary trauma scales. Lutherville, MD, USA: Sidran Press, 2005.
- Heinze KE, Hanson G, Holtz H, et al. Measuring Health Care Interprofessionals' Moral Resilience: Validation of the Rushton Moral Resilience Scale. J Palliat Med 2021;24:865-72. [Crossref] [PubMed]
- Mantri S, Lawson JM, Wang Z, et al. Identifying Moral Injury in Healthcare Professionals: The Moral Injury Symptom Scale-HP. J Relig Health 2020;59:2323-40. [Crossref] [PubMed]
- Nash WP, Marino Carper TL, Mills MA, et al. Psychometric evaluation of the Moral Injury Events Scale. Mil Med 2013;178:646-52. [Crossref] [PubMed]
- Wocial LD, Weaver MT. Development and psychometric testing of a new tool for detecting moral distress: the Moral Distress Thermometer. J Adv Nurs 2013;69:167-74. [Crossref] [PubMed]
- Pololi LH, Evans AT, Civian JT, et al. Assessing the Culture of Residency Using the C - Change Resident Survey: Validity Evidence in 34 U.S. Residency Programs. J Gen Intern Med 2017;32:783-9. [Crossref] [PubMed]
- Weiss DS. The impact of event scale: revised. In: Wilson JP, Tang CSk. editors. Cross-cultural assessment of psychological trauma and PTSD. Boston, MA, USA: Springer, 2007:219-38.



