
Effect of chewing gum on anxiety in women undergoing elective cesarean section: a randomized controlled study
Highlight box
Key findings
• Chewing gum did not alleviate preoperative anxiety for cesarean section
What is known and what is new?
• Pregnant women often experience the high level of anxiety before cesarean section, but an effective anxiolytic strategy has not been established.
• Chewing gum was associated with reduced procedural pain for regional anesthetic technique.
What is the implication, and what should change now?
• Further research is necessary to explore an alternative intervention to reduce anxiety before cesarean section.
Introduction
Cesarean section is one of the most commonly performed surgeries in obstetrics and gynecology (1). Pregnancy and childbirth bring great joy; however, a great number of pregnant women experience anxiety during pregnancy, and their anxiety levels are highest before cesarean section (2-4). Preoperative anxiety negatively affects puerperium and neonatal care as well as postoperative recovery in women undergoing cesarean section (5). In addition, high levels of anxiety weaken uterine contractions and negatively affect lactation through the neuroendocrine system after childbirth (6-8).
Pharmacologic interventions such as anxiolytics and sedatives for pregnant women are not recommended prior to delivery because they expose the newborn to the drug via the placenta and breastmilk and impede first bonding following childbirth. As a non-pharmacologic intervention, though cognitive behavioral therapies such as relaxation, yoga, and music have been used to relieve preoperative anxiety (8,9) the quality of evidence is very low. Another non-pharmacological intervention, chewing gum, has been reported to reduce stress and anxiety in acutely stressful situations (10,11). A recent study conducted at our institution in women who underwent laparoscopic gynecological surgery also found that chewing gum before surgery reduced stress and anxiety (12). Based on this, we conducted this prospective randomized trial with the hypothesis that chewing gum during the pre-anesthetic period would help alleviate preoperative anxiety and stress-related discomfort in women undergoing elective cesarean section. The study aimed to determine the anxiolytic effects of chewing gum in pregnant women undergoing elective cesarean section under regional anesthesia. We present the following article in accordance with CONSORT reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-22-811/rc).
Methods
Study participants
This study was a single-center, prospective, randomized controlled trial conducted at Samsung Medical Center, Korea, between October 2021 and February 2022. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Institutional Review Board of Samsung Medical Center (SMC No. 2021-07-053-002) and informed consent was taken from all the patients. The trial was prospectively registered on the Clinical Research Information Services (https://cris.nih.go.kr/cris/index.jsp; identifier: KCT0006602; date of registration: September 27, 2021).
Pregnant women scheduled to undergo elective cesarean section were assessed for eligibility. We included pregnant women after 37 weeks of pregnancy with the American Society of Anesthesiologists (ASA) physical status I–III. The exclusion criteria were as follows: age <19 years, unstable vital signs, increased risk of pulmonary aspiration, medication affecting gastrointestinal motility, and refusal to participate. The risk factors of pulmonary aspiration were defined as one or more of the following: body mass index (BMI) >35 kg/m2, esophageal stricture, achalasia, diabetic enteropathy, or history of gastrointestinal mass (13).
Randomization and blinding
Participants were allocated to either the control group or gum group at a 1:1 ratio. A randomization sheet with a block size of 2 was generated using a web service (www.randomizer.org). Allocation information was sealed in an opaque envelope numbered with a randomization sequence and stacked in labor and delivery units. Only one investigator (EKL) who was blinded to group assignment obtained informed consent and conducted baseline surveys and outcome assessments. An investigator (YJB) opened the envelope in sequence and then distributed chewing gum and instructions on the gum chewing protocol if the patients were allocated in gum group. Independent attending anesthetists performed combined spinal epidural anesthesia (CSE) according to institutional protocols (14). Obstetricians were also blinded to group assignment.
Intervention
Eligible participants provided written informed consent a day before surgery. Participants were requested to complete their first Amsterdam Preoperative Anxiety and Information Scale (APAIS) (15,16) to evaluate baseline anxiety. On the eve of surgery, all patients were explained about the surgery and anesthesia and rested with their families without any other medical treatment. For pre-anesthetic fasting, all participants were instructed to stop solid food ingestion 6 h before surgery and encouraged to drink clear liquid until 2 h before surgery (17,18).
In the gum group, the participants were provided a pack of xylitol gum (Sweetory xylitol, Daeyoung Foods Co., Korea) and instructed to chew a piece of gum for at least 10 min/h regardless of fasting. Gum chewing was started from 5 o’clock in the evening of the day before surgery until entering the operation theater. This was because our patients were hospitalized between 4 and 5 pm. Participants were requested to log their chewing time during each hour on a self-reported form. In the control group, participants were requested to follow fasting guidelines without further instructions.
Immediately before entering the operating room, all participants completed the APAIS questionnaire and rated their subjective sense of discomfort using a numeric rating scale (NRS; 0 to 10, 0 = no suffering, 10 = worst imaginable suffering) in the preoperative holding area. We also asked the participants to rate their pain during CSE induction using the NRS. The recovery satisfaction score was recorded 24 h after surgery.
Anesthesia and postoperative management
In the operating room, ASA standard monitoring, including noninvasive blood pressure, pulse oximetry, and 3-lead electrocardiography, was applied. CSE was performed according to the institutional protocol (14). Briefly, with the patient in the right lateral position, a 19-gauge epidural catheter was inserted via a 17-gauge Tuohy needle (FlexTip Plus®; Arrow International, Inc., Reading, PA, USA) at the L2–3 intervertebral space using a midline approach with the loss-of-resistance to air technique and fixed at 10–11 cm into the skin. Spinal tapping was performed at the L3–4 interspace with a 25-gauge Whitacre needle, and 8 mg 0.5% hyperbaric bupivacaine and 20 µg fentanyl were administered. Thereafter, an epidural injection of 10 mL of 0.2% ropivacaine was administered. After achieving adequate sensory blockage, cesarean section was initiated. After the first bonding with newborn, the parturients were sedated with propofol till the end of surgery. After surgery, the patient was transferred to the post-anesthetic care unit (PACU). All the women received a standardized postoperative supplemental analgesic regimen. Patient-controlled epidural analgesia (PCEA) with 1,000 µg fentanyl and 40 mL 0.75% ropivacaine mixed with 210 mL 0.9% saline was initiated in the PACU at the first complaint of pain (NRS >1/10) and programmed to deliver a background infusion of 4 mL/h with a 2 mL bolus and a 15-min lockout interval until postoperative day 2. If patients presented with breakthrough pain (NRS ≥4), intramuscular ketoprofen 100 mg or intravenous ketorolac 30 mg was administered as rescue analgesics. If this was ineffective, after 30 min intravenous pethidine 50 mg was administered. Feeding was started step-by-step 8 h after surgery or gas passage, and early ambulation was encouraged.
Measurements and outcomes
Demographic data, including age, gestational age, cause of cesarean section, past medical history, level of education, and job, were collected to compare baseline characteristics. Intraoperative variables including fluids, anesthetics, urine output, estimated blood loss, and any complications during the hospital stay were also collected from medical records.
The primary outcome was preoperative anxiety using the APAIS score (15) immediately before surgery. The APAIS is a useful tool for assessing preoperative anxiety, which consists of an anxiety scale and an informative desire scale (Appendix 1). This questionnaire consisted of six items representing preoperative anxiety (four items) and informative desire (two items) on a Likert scale (1 to 5, 1= not at all, 5= extremely). The scores of the anxiety and informative desire domain in the APAIS ranged from 4 to 20 and 0 to 10, respectively; a score of 11 in the anxiety scale of the APAIS being the cut-off value for diagnosing anxious patients (15). We compared the severity of symptoms related to preoperative anxiety between the groups as secondary outcomes. The subjective discomforts consisted of eight questions: unfitness, concentration difficulty, hunger, thirst, dry mouth, fatigue, headache, and nausea using NRS (Appendix 1). Pain scores using NRS for the anesthetic procedure, and postoperative nausea and vomiting (PONV) during the 3 postoperative days were collected. The time to flatus and resume feeding, recovery satisfaction score, and length of hospital stay were collected to compare the postoperative recovery between the groups.
Statistical analysis
Sample size was calculated based on the result of a previous study (12) using web based calculator (www.clincalc.com). The APAIS immediately before surgery from the previous literature was 20.9±5.7 [mean ± standard deviation (SD)]. We assumed that the APAIS score of the gum group compared to control group to decrease by 20% for clinically meaningful differences. With an alpha error of 5% and power of 80%, 29 participants were required for each group. We finally enrolled 33 patients per group permitting a dropout rate of 10%.
All data were tested for normality using the Shapiro-Wilk test and are presented as means (SD) or as medians [interquartile ranges (IQR)]. Differences between groups were analyzed using the chi-square test or Fisher’s exact test for categorical variables and Student’s t-test or Wilcoxon’s rank sum test for continuous variables, as appropriate. The Bonferroni correction was applied for multiple comparisons. Statistical significance was defined as a P value less than 0.05. All statistical analyses were performed using SPSS software (version 27.0; SPSS Inc., Chicago, IL, USA).
Results
Between October 2021 and February 2022, 152 women scheduled to undergo elective cesarean section were assessed for eligibility. All 66 of the enrolled participants were randomly assigned to one of the two groups and completed the intervention (Figure 1). The baseline patient characteristics of the two groups were comparable (Table 1). The median (IQR) chewing time was 120 min (IQR, 102–157 min) in gum group. We had instructed patients to chew gum for at least 10 min/h, but the chewing time of participants varied from a minimum of 40 min to a maximum of 309 min, depending on individual preferences and circumstances.
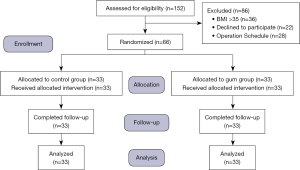
Table 1
| Characteristics | Control group (N=33) | Gum group (N=33) | P value |
|---|---|---|---|
| Age, years | 35.1±3.4 | 35.2±3.6 | 0.972 |
| Height, cm | 160.8±5.2 | 161.7±5.5 | 0.511 |
| Weight, kg | 69.5±6.5 | 73.3±11.5 | 0.099 |
| BMI, kg/m2 | 26.9±2.5 | 28.0±4.0 | 0.170 |
| Occupation, n (%) | 0.406 | ||
| Housewife | 12 (36.4) | 9 (27.3) | |
| Clerical worker | 12 (36.4) | 12 (36.4) | |
| Service worker | 1 (3.0) | 4 (12.1) | |
| Professionals | 6 (18.2) | 8 (24.2) | |
| Other | 2 (6.1) | 0 (0) | |
| Education level, n (%) | 0.558 | ||
| Deny | 2 (6.1) | 3 (9.1) | |
| High School graduate | 2 (6.1) | 3 (9.1) | |
| College graduate or higher | 29 (87.9) | 25 (81.9) | |
| Surgical history, n (%) | 0.703 | ||
| 0 | 7 (21.2) | 10 (30.3) | |
| 1 | 19 (57.6) | 14 (42.4) | |
| ≥2 | 7 (21.2) | 9 (27.3) | |
| History of the mode of anesthesia, n (%) | 0.786 | ||
| No history | 7 (21.2) | 10 (30.3) | |
| Sedation | 5 (15.2) | 3 (9.1) | |
| Regional anesthesia | 11 (33.3) | 11 (33.3) | |
| General anesthesia | 10 (30.3) | 9 (27.3) | |
| Primipara, n (%) | 19 (57.6) | 21 (63.6) | 0.801 |
| Reasons to have a cesarean section, n (%) | 0.225 | ||
| Repeated cesarean section | 14 (42.4) | 10 (30.3) | |
| Twin | 6 (18.2) | 9 (27.3) | |
| Placenta previa totalis | 2 (6.1) | 1 (3.0) | |
| Fetal presentation | 6 (18.2) | 3 (9.1) | |
| Uterus abnormality | 3 (9.1) | 2 (6.1) | |
| Maternal choice | 2 (6.1) | 9 (27.3) | |
Values are mean ± SD or numbers (%). BMI, body mass index; SD, standard deviation.
The primary outcome of APAIS score immediately before surgery was similar between the control and gum groups (19.2±5.8 vs. 19.1±4.1 min, P>0.99; Table 2). There were also no significant differences in the anxiety and information subsets of APAIS scores between the two groups. Considering that the anxiety scale of the APAIS score of 11 is the cut-off value for diagnosing anxious patients (15), there was no significant change in the proportion of anxious patients before and after the intervention. There were no statistically significant differences in the eight items related to anxiety: unfitness, concentration difficulty, hunger, thirst, dry mouth, fatigue, headache, and nausea (Table 2).
Table 2
| Outcomes | Control group (N=33) | Gum group (N=33) | Differences in means or medians (95% CI) | P value |
|---|---|---|---|---|
| Baseline APAIS, 0–30 | ||||
| Total score | 18.4±4.4 | 18.0±3.2 | 0.2 (−2.3 to 2.6) | > 0.99† |
| Anxiety domain | 12.1±3.1 | 12.1±2.5 | 0.0 (−1.9 to 1.8) | > 0.99† |
| Informative desire domain | 6.3±1.7 | 5.9±1.7 | 0.2 (−0.8 to 1.1) | > 0.99† |
| Anxiety prevalence, n (%) | 21 (63.6) | 23 (69.7) | – | 0.397 |
| Preoperative APAIS, 0–30 | ||||
| Total score | 19.2±5.8 | 19.1±4.1 | 0.2 (−2.3 to 2.6) | > 0.99† |
| Anxiety domain | 13.1±4.3 | 13.1±3.0 | 0 (−1.9 to 1.8) | > 0.99† |
| Informative desire domain | 6.2±2.0 | 5.7±1.8 | 0.2 (−0.8 to 1.1) | > 0.99† |
| Anxiety prevalence, n (%) | 23 (69.7) | 27 (81.8) | – | 0.389 |
| Satisfaction about preoperative care, NRS 0–10 | 6 [2–9] | 7 [3–9] | 0 (−2 to 1) | 0.566 |
| Discomforts, NRS 0–10 | ||||
| Unfitness | 1 [0–3] | 1 [0–3] | 0 (−1 to 1) | 0.934 |
| Concentration difficulty | 4.2±3.0 | 4.6±2.3 | 0.3 (−1.2 to 1.8) | 0.580 |
| Hunger | 4 [1–6] | 5 [0–6] | 0 (−1 to 2) | 0.853 |
| Thirst | 6 [4–8] | 5 [2–7] | 1 (−1 to 2) | 0.403 |
| Dry mouth | 5.58±2.94 | 5.27±3.10] | 0.7 (−1.2 to 1.8) | 0.685 |
| Fatigue | 5 [3–8] | 5 [3–7] | 0 (−2 to 1) | 0.850 |
| Headache | 0 [0–5] | 1 [0–2] | 0 (0 to 0) | 0.948 |
| Nausea | 0 [0–3] | 0 [0–3] | 0 (0 to 0) | 0.785 |
Values are mean ± SD, median [IQR], or number (%). †, P values are adjusted using Bonferroni correction for multiple comparisons. APAIS, Amsterdam Preoperative Anxiety and Information Scale; NRS, numeric rating scale; SD, standard deviation; IQR, interquartile range.
The median (IQR) pain score during the CSE procedure was significantly lower in the chewing gum group than in the control [4 (IQR, 3–5.5) vs. 5 (IQR, 3–7), P=0.045; Table 3]. There were no significant differences in the recovery outcomes, including time to flatus, time to resume feeding, PONV, additional analgesic requirements, and length of hospital stay.
Table 3
| Outcomes | Control group (N=33) | Gum group (N=33) | Differences in means or medians (95% CI) | P value |
|---|---|---|---|---|
| Pain severity at CSE induction, NRS 0–10 | 5 [3–7] | 4 [3–5.5] | 1 (0 to 2) | 0.045* |
| Total propofol usage, mg | 250.0±100.7 | 217.9±84.2 | 32.1 (−13.5 to 77.8) | 0.165 |
| Crystalloid, mL | 900 [700–1,100] | 800 [600–1,000] | 100 (−100 to 300) | 0.309 |
| Colloid, mL | 500 [500–500] | 500 [500–500] | 0 (0 to 0) | 0.774 |
| Estimated blood loss, mL | 800 [800–1,000] | 800 [700–1,000] | 0 (−100 to 100) | 0.901 |
| Urine, mL | 200 [100–350] | 300 [170–400] | −50 (−130 to 50) | 0.476 |
| Time to flatus, h | 17.4±9.6 | 18.2±10.4 | −0.8 (−5.7 to 4.1) | 0.753 |
| Time to resume feeding, h | 20.6 [19.4–23] | 20.3 [18.3–23] | 0.7 (−0.9 to 2.4) | 0.373 |
| Total PCEA usage time, h | 49.5 [48–51.3] | 49.1 [46.8–50.7] | 0.7 (−1.1 to 2.3) | 0.353 |
| Number of patients who received analgesic requirements, n (%) | 0.476 | |||
| 3 times | 21 (63.6) | 24 (72.7) | ||
| 4–6 times | 3 (9.1) | 4 (12.1) | ||
| ≥7 times | 9 (27.3) | 5 (15.2) | ||
| PONV requiring antiemetics, n (%) | 0 (0) | 2 (6.1) | N/A | 0.672 |
| Length of stay, days | 4 [4–4] | 4 [4–4] | 0 (0 to 0) | 0.613 |
| Satisfaction for recovery, NRS 0–10 | 7 [5–8] | 7 [6–8] | 0 (−1 to 1) | 0.608 |
Values are mean ± SD, median [IQR], or number (%). *, P<0.05. CSE, combined spinal epidural anesthesia; N/A, not applicable; NRS, numeric rating scale; PCEA, patient-controlled epidural analgesia; PONV, postoperative nausea or vomiting; SD, standard deviation; IQR, interquartile range.
Discussion
In this randomized controlled trial assessing the anxiolytic effects of chewing gum, we could not demonstrate a difference between the groups in our primary outcome of anxiety level scores measured immediately before surgery in women undergoing elective cesarean section.
Preoperative gum chewing is a cost-effective, easy-to-implement, and patient-controlled anxiety relief strategy (19). A recent study conducted at our institution in women undergoing gynecological surgery demonstrated that preoperative gum chewing was associated with reduced preoperative anxiety (12). However, in the present study, we failed to validate the hypothesis that preoperative gum chewing would reduce anxiety in pregnant women undergoing cesarean section, which is consistent with recent meta-analyses that found no evidence to support anxiolytic effect of gum chewing (8,10). The discrepancy of our findings from the previous studies may be explained by differences in anesthesia (general vs. regional) and causes of cesarean section. A previous study comparing anxiety levels between general and regional anesthesia for elective cesarean section reported that patients undergoing cesarean section under regional anesthesia had higher anxiety than those under general anesthesia (20). In this study, all women received regional anesthesia (i.e., CSE). Another reason may be differences in the causes of cesarean section. Women who self-selected cesarean section were significantly more anxious than women who did not (21). In our study, the proportion of women who self-selected cesarean section was three times higher in the gum group (27.3%) than in the control group (6.1%).
One of the notable findings of our study was that the pain score during CSE induction was significantly lower in the gum group than in control group. Although the anxiolytic effect of gum chewing was not confirmed, the fact that gum chewing was associated with a lower level of pain during CSE induction in cesarean section is noteworthy. This is consistent with previous studies that chewing gum may relieve labor pain (22) or procedural pain in medical experiences (23-25). For surgical patients, higher anxiety is associated with severe pain and increased analgesic requirements (26,27). Although the exact mechanism is not known, it is speculated that chewing gum may have affected pain sensation by relieving stress (24). However, it cannot be determined whether the reduced pain score during CSE induction in the gum group was a result of chewing gum. Further studies are required to clarify this point.
The major concern related to chewing gum during preoperative fasting is possibly increased risk of pulmonary aspiration by increased gastric fluid volume and acidity (28). Previous study demonstrated that factors that could affect pulmonary aspiration risk such as saliva secretion, gastric fluid volume, and gastric fluid acidity remained unchanged after gum chewing (12). In our study, there were no women who showed adverse events associated with gum chewing.
This study had several limitations. First, participants were not blinded to the intervention. Although the outcome assessor was blinded, it would have been more appropriate to establish an active control group to exclude the placebo effect. Second, APAIS focuses on examining anxiety about surgery and anesthesia, but maternal concerns before delivery are not limited to surgery and anesthesia. Further studies using other anxiety measurement tools are required. Third, the intervention duration was too short to cause a change in the anxiety level. The intervention that started on the eve of the operation may not have been sufficient to relieve the woman’s anxiety and prepare her psychologically. Finally, this trial was conducted at a single tertiary center in Korea. Our participants were Koreans who received CSE according to our institutional protocol. If this study had been conducted in women undergoing cesarean section under general anesthesia or in women of other cultures, the results might have been different. This is because is influenced by the anesthesia method, culture, as well as personal experiences.
Conclusions
Preoperative gum chewing did not reduce anxiety measured immediately before entering the operating room in participants undergoing elective cesarean section. Nevertheless, it was noted that gum chewing was associated with a lower level of pain during CSE induction in cesarean section.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-22-811/rc
Trial Protocol: Available at https://apm.amegroups.com/article/view/10.21037/apm-22-811/tp
Data Sharing Statement: Available at https://apm.amegroups.com/article/view/10.21037/apm-22-811/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-22-811/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This research was approved by the
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- OECD. Caesarean sections (indicator). doi:
10.1787/adc3c39f-en [Accessed on 07 March 2022], Available online: https://data.oecd.org/healthcare/caesarean-sections.htm10.1787/adc3c39f-en - Hepp P, Hagenbeck C, Burghardt B, et al. Measuring the course of anxiety in women giving birth by caesarean section: a prospective study. BMC Pregnancy Childbirth 2016;16:113. [Crossref] [PubMed]
- Hobson JA, Slade P, Wrench IJ, et al. Preoperative anxiety and postoperative satisfaction in women undergoing elective caesarean section. Int J Obstet Anesth 2006;15:18-23. [Crossref] [PubMed]
- Fentie Y, Yetneberk T, Gelaw M. Preoperative anxiety and its associated factors among women undergoing elective caesarean delivery: a cross-sectional study. BMC Pregnancy Childbirth 2022;22:648. [Crossref] [PubMed]
- Consonni EB, Calderon IM, Consonni M, et al. A multidisciplinary program of preparation for childbirth and motherhood: maternal anxiety and perinatal outcomes. Reprod Health 2010;7:28. [Crossref] [PubMed]
- Grajeda R, Pérez-Escamilla R. Stress during labor and delivery is associated with delayed onset of lactation among urban Guatemalan women. J Nutr 2002;132:3055-60. [Crossref] [PubMed]
- Johnson RC, Slade P. Obstetric complications and anxiety during pregnancy: is there a relationship? J Psychosom Obstet Gynaecol 2003;24:1-14. [Crossref] [PubMed]
- Weingarten SJ, Levy AT, Berghella V. The effect of music on anxiety in women undergoing cesarean delivery: a systematic review and meta-analysis. Am J Obstet Gynecol MFM 2021;3:100435. [Crossref] [PubMed]
- Smith CA, Levett KM, Collins CT, et al. Relaxation techniques for pain management in labour. Cochrane Database Syst Rev 2018;3:CD009514. [Crossref] [PubMed]
- Luo J, Xia M, Zhang C. The Effects of Chewing Gum on Reducing Anxiety and Stress: A Meta-Analysis of Randomized Controlled Trials. J Healthc Eng 2022;2022:8606693. [Crossref] [PubMed]
- Yaman-Sözbir Ş, Ayaz-Alkaya S, Bayrak-Kahraman B. Effect of chewing gum on stress, anxiety, depression, self-focused attention, and academic success: A randomized controlled study. Stress Health 2019;35:441-6. [Crossref] [PubMed]
- Bang YJ, Lee JH, Kim CS, et al. Anxiolytic effects of chewing gum during preoperative fasting and patient-centered outcome in female patients undergoing elective gynecologic surgery: randomized controlled study. Sci Rep 2022;12:4165. [Crossref] [PubMed]
- Birenbaum A, Hajage D, Roche S, et al. Effect of Cricoid Pressure Compared With a Sham Procedure in the Rapid Sequence Induction of Anesthesia: The IRIS Randomized Clinical Trial. JAMA Surg 2019;154:9-17. [Crossref] [PubMed]
- Kang R, Lee S, Lee E, et al. Validation and Clinical Utility of the Korean Version of the Obstetric Quality-of-Recovery Score (ObsQoR-11) Following Elective Cesarean Section: A Prospective Observational Cohort Study. Diagnostics (Basel) 2022;12:291. [Crossref] [PubMed]
- Moerman N, van Dam FS, Muller MJ, et al. The Amsterdam Preoperative Anxiety and Information Scale (APAIS). Anesth Analg 1996;82:445-51. [PubMed]
- Shin WJ, Kim YC, Yeom JH, et al. The Validity of Amsterdam Preoperative Anxiety Information Scale in the Assessment of the Preoperative Anxiety - Compared with hospital anxiety depression scale and visual analogue scale. Korean J Anesthesiol 1999;37:179-87. [Crossref]
- Smith I, Kranke P, Murat I, et al. Perioperative fasting in adults and children: guidelines from the European Society of Anaesthesiology. Eur J Anaesthesiol 2011;28:556-69. [Crossref] [PubMed]
- Practice Guidelines for Preoperative Fasting and the Use of Pharmacologic Agents to Reduce the Risk of Pulmonary Aspiration: Application to Healthy Patients Undergoing Elective Procedures: An Updated Report by the American Society of Anesthesiologists Task Force on Preoperative Fasting and the Use of Pharmacologic Agents to Reduce the Risk of Pulmonary Aspiration. Anesthesiology 2017;126:376-93. [Crossref] [PubMed]
- Ang AAC, Almora CCD, Al-Qaseer EC, et al. Randomized controlled trial on the effect of pre-operative gum chewing on the level of postoperative anxiety among boys undergoing circumcision. Health Sci J 2014;3:25-30.
- Maheshwari D, Ismail S. Preoperative anxiety in patients selecting either general or regional anesthesia for elective cesarean section. J Anaesthesiol Clin Pharmacol 2015;31:196-200. [Crossref] [PubMed]
- Sun Y, Huang K, Hu Y, et al. Pregnancy-specific anxiety and elective cesarean section in primiparas: A cohort study in China. PLoS One 2019;14:e0216870. [Crossref] [PubMed]
- Ebrahimian A, Bilandi RR, Bilandī MRR, et al. Comparison of the effectiveness of virtual reality and chewing mint gum on labor pain and anxiety: a randomized controlled trial. BMC Pregnancy Childbirth 2022;22:49. [Crossref] [PubMed]
- Yildizeli Topcu S, Akgun Kostak M, Semerci R, et al. Effect of Gum Chewing on Pain and Anxiety in Turkish Children During Intravenous Cannulation: A Randomized Controlled Study. J Pediatr Nurs 2020;52:e26-32. [Crossref] [PubMed]
- Kamiya K, Fumoto M, Kikuchi H, et al. Prolonged gum chewing evokes activation of the ventral part of prefrontal cortex and suppression of nociceptive responses: involvement of the serotonergic system. J Med Dent Sci 2010;57:35-43. [PubMed]
- Lewkowski MD, Barr RG, Sherrard A, et al. Effects of chewing gum on responses to routine painful procedures in children. Physiol Behav 2003;79:257-65. [Crossref] [PubMed]
- Armstrong AD, Hassenbein SE, Black S, et al. Risk Factors for Increased Postoperative Pain and Recommended Orderset for Postoperative Analgesic Usage. Clin J Pain 2020;36:845-51. [Crossref] [PubMed]
- Wilson JM, Colebaugh CA, Flowers KM, et al. Early postoperative psychological distress as a mediator of subsequent persistent postsurgical pain outcomes among younger breast cancer patients. Breast Cancer Res Treat 2022;196:363-70. [Crossref] [PubMed]
- Bouvet L, Loubradou E, Desgranges FP, et al. Effect of gum chewing on gastric volume and emptying: a prospective randomized crossover study. Br J Anaesth 2017;119:928-33. [Crossref] [PubMed]


