
Complexity of patient care needs in palliative care: a scoping review
Highlight box
Key findings
• A consensual definition of complexity is needed.
What is known and what is new?
• The definition for clinical complexity is still underexplored, as well as the instruments available to assess complexity.
• This scoping review aims to gather relevant information on the definition of clinical complexity in PC, as well as on the instruments used to objectively assess complexity.
What is the implication, and what should change now?
• The present scoping review suggest a need for systematic reviews on both topics, which may be able to provide support to a consensual definition of complexity, further contributing for instrument improvement.
Introduction
Palliative care (PC) is health care provided to a person with a serious and progressive, life-threatening illness, without the possibility of treatment, and is associated with a high degree of suffering (physical, psychological, social and spiritual) (1). PC is aimed to avoid and manage suffering, as well as to improve quality of life of PC patients. Interdisciplinary PC teams address the intervention to both patients and families, by an early identification, assessment, and suffering management, also supporting the family through the grieving process (2).
According to the biopsychosocial-spiritual model, suffering is a direct consequence not only of the disease, but also of the psychosocial and spiritual dimensions of the person. This person-centered care model is reflected in the organizational models of PC teams, highlighting the need of multidisciplinary teams, where each health professionals carry out an independent assessment of the patient, contributing to a broader and comprehensive assessment, improving the treatment plan, as an additional layer of services (3).
Early identification of needs in PC, and subsequent referral to PC teams, has a positive impact on the quality of life of patients and their families, being crucial to draw integrated care plans. However, early identification does not necessarily mean referral to specialized services for patients with moderate/high clinical complexity. Yet, these patients would benefit from a palliative approach, adjusting differentiated care in case of complexity, according to a collaborative and integrated model (2).
Complexity in the palliative patient is a concept that has been developed in recent years. It is a multifaceted term that encompasses several levels and domains, including all the conditions experienced by a person during the course of the disease (whether in the transversal or longitudinal context), persons’ values, family, and the surrounding environment (such as social and/or financial characteristics), that may interfere in the perception of symptoms, influencing the course of the disease. All the aforementioned factors must be considered in the evaluation of the clinical complexity of the PC patient (4), acknowledging that this is dynamic and modular phenomenon (5).
Rationale for the review
The assessment of the degree of complexity, would allow to adjust the responses of health professionals to the needs of the patient and family/caregiver, in line with bioethical and PC principles, in a time-effective way, avoiding unnecessary suffering for the patient and family (6). It is consensual that it warrants a multidimensional assessment and multidisciplinary intervention (4). Yet, the definition of complexity and the usability of the instruments available to objectively assess complexity are still little explored.
It seems crucial to find a universal definition of complexity in PC patients, as well as suitable and accurate instruments to assess it, in order to improve decision-making and resources allocation, facilitating and systematizing the intervention of PC teams (1). This is particularly important in high-income countries where it is estimated that 30-45% of PC patients are in a clinical status with such complexity that should receive specialized PC (7).
Objectives
The main aim of this Scoping Review is to identify, and map suggested definitions of clinical complexity of patients in need of PC, as well as the instruments available to objectively assess complexity, and its suitability to the clinical setting. The following questions guided the review of the literature: (I) What are the prevailing definitions of clinical complexity of patients with PC needs? (II) What are the instruments available to assess complexity in PC, which may be suitable to be used at the clinical setting? We present this article in accordance with the PRISMA-ScR reporting checklist (8) (available at https://apm.amegroups.com/article/view/10.21037/apm-22-894/rc).
Methods
Eligibility criteria
Scientific articles published in international peer-reviewed journals, referring to (I) the definition, approach and/or protocols, related to the clinical complexity in patients followed up or in need of PC; (II) the instruments used to assess clinical complexity in PC, were considered, independently of language or publication date.
As exclusion criteria were considered: books and book chapters, opinion articles, case studies, conference abstracts, and guidelines. Although the identified sources may be included in systematic reviews without a critical impairment of quality (9), to the best of our knowledge, there is no evidence on the impact of it inclusion in scoping reviews.
Information sources and search strategy
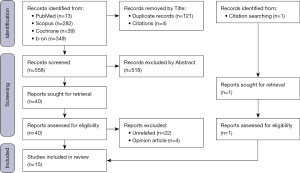
The search syntax was initially used on PubMed/MEDLINE to test and optimize the search strategy and was subsequently used on all the other databases (i.e., Scopus, Cochrane, and b-on databases), using the search terms: (“palliative care” AND “hospitalization criteria”; “palliative care” AND “complexity criteria”; palliative care AND “complexity assessment”; “palliative care” AND “clinical complexity”. Study selection and screening were conducted by two researchers, GC and AVS, who independently reviewed and analyzed titles and abstracts of the studies found in the search and entry them on to a Microsoft Excel matrix, which was used to gather the number of hits for each article from all databases, remove duplicate records and assess eligibility for inclusion. Full texts of the selected articles were further reviewed independently to establish compliance with the eligibility criteria. The search was performed during April 2022. In each selection phase (i.e., identification, selection, illegibility, and inclusion) the results obtained by the researchers were compared and discussed. According to the methodology of a Scoping Review (10), the methodological quality of the included studies was not analyzed.
Results
From 683 references identified, 668 did not meet the inclusion/exclusion criteria after identification and screening processes, thus 15 articles were included in the present review. The screening process is presented in the PRISMA flow diagram (Figure 1) (11).
Seven studies (46.7%) were carried out in Spain, 2 (14.3%) in the UK, 2 (14.3%) in the USA, 1 (7.1%) in Germany, 1 (7.1%) in Switzerland, 1 (7.1%) in Australia, with 1 (7.1%) resulting from an international collaboration between Australia and the Netherlands (Tables 1,2).
Table 1
| Author, year | Objectives | Design | Context (country) | Participants/studies | Complexity domains | Results/Conclusions |
|---|---|---|---|---|---|---|
| Busquet-Duran et al., 2020 | Description of complexity in patients with PC needs | Original research (cross-sectional) | Community (Spain) | Patients (n=832) | Clinical, psychological, spiritual, socio-familial, ethical, and end-of-life (18 subdomains) | The socio-family domain, the integrated care plan, and end-of-life communication (with discussion of the place of death) are particularly relevant |
| Carduff et al., 2018 | Description of complexity in PC (healthcare professionals’ perspective) | Original research (qualitative interviews) | Healthcare* (UK) | Healthcare professionals (n=34) | Patient (psychosocial, physical, and spiritual), health system and sociocultural | Complexity perception depends on the characteristics of the healthcare professionals (training, experience); training in PC is essential for a better identification of complexity |
| Hodiamont et al., 2019 | Development of a conceptual model of complexity | Original research (qualitative interviews) | Healthcare* (Germany) | Healthcare professionals (n=42) | Patient, social and healthcare team | Complexity in PC should be adjusted to the stage of the disease (adaptive system) |
| Murali et al., 2020 | Development a conceptual model of clinical complexity | Review (narrative review) | Healthcare* (USA) | Included studies (n=58) | Patients and family’s needs, factors that may affect health services, provided care by the service that cares for the patient and family, and patients and family’s condition | The developed model should guide future investigations, although the unique personal and psychosocial characteristics must be considered |
| Pask et al., 2018 | Development of a complexity concept | Original research (qualitative interviews) | Healthcare* (UK) | Patients, family, and healthcare professionals (n=65) | Physical, psychological, social, spiritual, and pre-existing, cumulative, and invisible complexity (micro-system, meso-system, eso-system, macro-system, chrono-system) | Complexity should reflect the reality of the patient and family, and its perception by patients, family, and healthcare professionals |
*, healthcare, including community, nursing homes, and hospital settings. PC, palliative care.
Table 2
| Author, year | Objectives | Design | Context (country) | Participants/studies | Instruments | Results/conclusions |
|---|---|---|---|---|---|---|
| Busquet-Duran et al., 2020 | Development of an instrument able to assess complexity | Original research (cross-sectional) | Community (Spain) | Patients with PC needs (n=832) | HexCom | Consistent tool; possible validation in clinical practice |
| Busquet-Duran et al., 2021 | Validation of HexCom in complexity assessment | Original research (Delphi method) | Community (Spain) | Patients with PC needs (n=14) | HexCom | Valid and useful instrument (including adaptations) for complexity assessment |
| Carrasco-Zafra et al., 2020 | Description of complexity levels | Original research (retrospective observational) | Community (Spain) | Cancer patients (n=42) | IDC-Pal | Useful instrument in the identification of clinical complexity-related factors, and in the timely referral to specialized PC teams |
| Grant et al., 2021 | Identification of complexity assessment instruments | Review (systematic review) | The Netherlands and Australia | Included studies (n=9) | HexCom, Perroca Scale, AN-SNAP, Hui Major Criteria, IDC-Pal, and PALCOM | HexCom and IDC-Pal allow a broader determination of complexity from a personal perspective |
| Kamal et al., 2021 | Development of a complexity assessment instrument | Original research (retrospective observational) | Healthcare (USA) | Outpatient/ambulatory (n=3,121) | QDACT (adaption) | Patient characteristics, diagnosis, and team characteristics, at the time of the request for a PC consultation, are associated with complexity level |
| Teike Lüthi et al., 2021 | Validation of the ID-PALL | Original research (prospective) | Hospital (Switzerland) | Inpatient (n=2,232) | ID-PALL | Useful in the identification of complexity level in patients with PC needs (generalists versus specialized) |
| Martin-Rosello et al., 2018 | Clinical complexity assessment | Review (narrative review) | Community (Spain) | Included studies (n=31) | Hui’s criteria, PALCOM, INTERMED, and IDC-Pal | IDC-PAL is a valid instrument to assess complexity in patients with PC needs |
| Masso et al., 2016 | Test the reliability and validity of the PCPSS | Original research (cross-sectional) | Hospital (Australia) | Patients with PC needs (n=420) | PCPSS | Acceptable instrument (moderate reliability) |
| Mota-Romero et al., 2021 | Assessment of clinical complexity | Original research (cross-sectional) | Nursing homes (Spain) | Patients with PC needs living in nursing homes (n=149) | Frail-VIG index, CCIndex, IDC-Pal, Palliative prognosis index, Barthel index (dependency), Pfeiffer’s test, and ChCI | IDC-Pall is a suitable instrument, yet nursing home patient needs do not always match the elements identified as complex in the IDC-Pal; there is a need to adapt complexity detection instruments to this type of institution |
| Tuca et al., 2018 | Development a of PC complexity scale | Original research (prospective) | Healthcare (Spain) | Patients with PC needs (n=324) | PALCOM | Useful instrument for complexity stratification in patients with PC needs |
PC, palliative care; AN-SNAP, Australian National Subacute and Non-acute Patient Classification; CCIndex, case complexity index; Frail-VIG index, Frail-VIG (abreviatura de Comprehensive Geriatric Assessment em castelhano) index; HexCom, The Hexagon of Complexity model; IDC, nstrumento Diagnóstico de la Complejidad en Cuidados Paliativos; ID-PALL, IDentification of patients in need of PALLiative care; INTERMED, método de avaliação biopsicossocial para documentar informações integradas das necessidades dos doentes; PALCOM, predictive model of complexity in palliative care; PCPSS, palliative care problem severity score; QDACT, quality data collection tool; Hui’s criteria, The Health Utilities Index Major Criteria; ChCI, Charlson comorbidity index.
Regarding methodology, 12 (80%) studies showed do be original investigations (cross-sectional n=4, qualitative interviews n=3, retrospective n=2, prospective n=2, Delphi method n=1), and 3 (20%) literature reviews (narratives n=2, systematics n=1) (Tables 1,2).
Five studies (33.3%) aimed to find/clarify the definition of complexity in patients with PC needs (Table 1), in line with the first objective of the present study; and 10 (66.7%) aimed to report on instruments for the assessment of complexity in patients with PC needs (Table 2), in line with the second study objective. All the included studies were published between 2016 and 2021.
Definition of complexity
According to the studies included the definition of complexity in patients with PC needs can be organized into:
- 3 domains (n=1 study): patient domain (psychosocial, physical, and spiritual), health system and sociocultural (12).
- 4 domains (n=2 articles): factors that affect the needs of patients and families (sociodemographic and social determinants of health); factors that affect health services (health system in general—research, health policy; resources in the community), factors related to the variables of the service that takes care of the patient and family (quality of care, experience) and patient’s condition and families (symptom burden, quality of life, cost, death, place of death, satisfaction) (13); or physical, psychological, social, spiritual, associated with factors of pre-existing and cumulative complexity, interconnected in the micro-system, meso-system, eso-system, macro-system, and chrono-system (14).
- 6 domains (n=1 article): clinical, psychological, spiritual, socio-family, ethical, end of life and 18 subdomains, including physical, therapeutic, relational, emotional, practical, external, financial and place of death in the last days (15).
Instruments used in the assessment of complexity in patients with PC needs
A total of 13 instruments used to assess the complexity of patients in need of PC were identified. The instruments are listed in descending order of use/citation:
- IDC-Pal (n=5 articles): The Diagnostic Instrument for Complexity in PC (IDC-Pal) is an instrument that assesses aspects related to the patient, family support and the organization of the PC team focusing on the patient and family. Each of the 36 items is identified as non-complex, complex, or highly complex, allowing the characterization of the level of complexity as non-complex (absence of complex or highly complex items), complex (presence of one or more complex items, but no highly complex items) or highly complex (presence of at least one highly complex item). In the case of a non-complex status, usual care may be maintained, without the need of a specialized PC team. However, in a complex status, the criterion for follow-up by the specialized PC team may depend on the PC team’s assessment. In a highly complex status, the intervention of the specialized team should be mandatory. According to the present review, the IDC-Pal seems to be the most used instrument, having already been validated for several languages (15-19).
- HexCom (n=3 articles): The Hexagon of Complexity model (HexCom) is a Spanish model, with 18 items, which aims to define complexity as low (PC approach), moderate, and high complexity (need for specialized PC), in six domains: clinical, psychological, spiritual, socio-familiar, ethical, and end of life. HexCom seems to be particularly useful at the community level (17,20,21).
- PALCOM (n=3 articles): The Predictive Model of Complexity in Palliative Care (PALCOM) is an instrument developed in Spain, consisting of 24 items, including the Karnofsky functional scale and the Edmonton Classification System for Cancer Pain (ECS-CP). It is a validated tool for patients diagnosed with advanced stage neoplasia, that allow the classification of complexity in three levels: low complexity (with no need of specialized PC team intervention), moderate complexity (where the treatment plan showed be discussed with a specialized PC team), and high complexity (where patients’ follow-up should be made by a specialized PC team) (17,18,22).
- HUI Major Criteria (n=2 articles): The Health Utilities Index Major Criteria (HUI’s criteria) was developed in the USA and comprises 11 items that suggest the need for follow-up by the specialized PC team. It addresses the personal domain and health services. It was developed according to the Delphi method, with a total of 60 international specialists in PC, mainly for cancer patients (15,17).
- Perroca Scale (n=1 article): The Perroca Scale was developed in Brazil, consisting of 10 to 13 items, aiming to classify patients’ needs according to clinical complexity into minimal, intermediate, intensive, and highly intensive complexity. Although it has been used in PC units, it was not created for this purpose, being not validated yet for the population with PC needs (17).
- AN-SNAP (n=1 article): The Australian National Subacute and Non-acute Patient Classification (AN-SNAP) is an instrument developed in Australia, comprising 9 items, aiming to identify complexity in inpatients or at home. It mainly addresses patients’ personal and social domains. AN-SNAP do not stands alone, requiring the parallel use of other instruments, such as the Resource Utilization Groups - Activities of Daily Living Score (RUG-ADL) and the Palliative Care Problem Severity Score (PCPSS) (17).
- Frail-VIG index (n=1 article): The Comprehensive Geriatric Assessment (Frail-VIG) index was developed in Spain and contains 22 items, that aim to assess the degree of frailty of geriatric patients, being a predictor of mortality at 24 months. Although it has been used in PC units, there is no validation for its use on populations in need of PC (18).
- CCIndex (n=1 article): The Case Complexity Index (CCIndex) is an instrument developed in Spain, consisting in 14 items, that aim to identify the complexity of patients who remain at home and who need nursing care at home. It is not validated for the population in need of PC (18).
- ChCI (n=1 article): The Charlson Comorbidity Index (ChCI) is a method of characterizing patients’ comorbidities. Each comorbidity is associated with a value that is directly related to the risk of mortality. It is not validated for the population in need of PC (18).
- INTERMED (n=1 article): The biopsychosocial assessment method to document integrated information on patients’ needs (INTERMED) is an instrument used by the observer during a structured interview, which allows to classify information into four domains: biological, psychological, social and health. Each domain is evaluated from a timely point of view (history, status, and prognosis) resulting in 20 variables. The output shows the patients’ area of vulnerability, care needs, and provide a direction for the elaboration of the integrated care plan (15).
- QDACT (n=1 article): The Quality Data Collection Tool (QDACT) is a registry that includes patient demographic and clinical information. In the study included in this review, this instrument was adapted, and variables such as quality of life, physical symptoms and advanced care plan were added to the instrument (23).
- ID-PALL (n=1 article): The Identification of patients in need of Palliative care (ID-PALL) instrument was developed in Switzerland, and contains 15 items, which assess the level of complexity of patients with PC needs. This instrument is divided into two parts: the first part (7 items) indicates the level of complexity and allow to identify those patients who would benefit from a PC approach; the second part (8 items) assesses the level of complexity of patients who could benefit from specialized PC. It is a recent and promising instrument in the assessment of complexity, allowing the differentiation of patients who would benefit from general versus specialized PC (24).
- PCPSS (n=1 article): The Palliative Care Problem Severity Score (PCPSS) is an instrument that assesses four PC domains: pain, other symptoms, psychological/spiritual and family/caregiver. This instrument is additionally required for AN-SNAP use (14).
Discussion
Clinical complexity concept in patients with PC needs is not well defined, being necessary to differentiate complex situations from complexity criteria (25). This is crucial to provide the best healthcare to patients and families (26).
Progress in the definition of complexity
Although PC has its roots in the UK in the 60s (27), the timeline (2016-2021) and the low number of studies included in this review highlight the novelty, and the need for further investigation on this topic.
The need for an objective definition of clinical complexity, encouraged original research studies such as the one of Carduff et al. (in 2018) (12), that based on semi-structured interviews with PC health professionals, purposed a definition of complexity, similar to the one defined by Schaink’s complexity model (not specific to PC but to the healthcare system) (28), where the social, demographic, psychological, physical and economic status, coexist and interact with the sociopolitical reality, influencing the perception and the definition of complexity, that is, a multidimensional model where the patient and family are the center of the intervention of PC teams, with their complexity being directly related to other surrounding dimensions, from the most (such as the physical, psychological, social and spiritual dimensions) to the less direct dimensions (such as the healthcare system and/or the sociocultural and political scenery) (15).
A coeval study by Pask et al. (in 2018), including families and health administrators, in addition to health professionals, suggested that complexity in PC, should consider all the elements included in the dimensions and systems that surround the patient and the family: (I) the “micro-system”, related to the person needs and characteristics, comprising factors such as patients’ age, personal history, addictions, symptoms types and characteristics, PC emergencies, and adaptation disorders, or emotional adjustment problems in disease acceptance or in its evolution; (II) the “chrono-system”, regarding the change of complexity over time; (III) the “meso-system”, comprising patient-family-healthcare team interactions, focusing on elements such as the patient’s dependence for performing daily activities, the absence of a caregiver capable of ensuring basic support, social fragility, and the presence of risk factors for a complicated grief process (29). When considering the interaction between the patient and family, and the healthcare teams, or the interactions between distinct healthcare teams that follow the patient at the same time, the integrative model should be continuously monitored to ensure its functionality; (IV) the “eco-system” is characterized by the accessibility to specialized care levels based; and (V) the “macro-system” corresponding to the society and people in general, comprising health policies at national and global levels. This multidimensional model showed that the complexity of the PC patient is not related to the type of diagnosis and/or prognosis, but rather and mainly to the assessment of the intrinsic needs of the patient and family, as well as the perceived “complexity” by the healthcare professionals who follow the patient, that is, in a multidimensional and adaptive model (29,30).
In 2019, Hodiamont et al., published an original study based on the Complex Adaptive Systems theory, using semi-structured qualitative interviews, including specialized PC professionals and health administration professionals (31). The Complex Adaptive System is a large-scale, dynamic system that evolves and adapts to changes and events in the system and the environment (32). Based on this model, three systems were identified in the context of PC: the patient (personal symptomatic control), the social, and the PC team systems. Each of these interconnected systems, has its own subsystems, also interconnected.
In 2020, a literature review suggested a new conceptual model to be applied to severe diseases, multiple chronic conditions, and PC (13). This model was based on the characterization of severe diseases associated with patients’ multi-comorbidity, identifying domains directly dependent on the patients’ needs, on the characteristics of the healthcare teams involved, and of the holistic approach to PC. This model points to the interconnection between domains (and subdomains) and external factors such as sociodemographic characteristics, health system, health policies and access to healthcare (13).
Also in 2020, Busquet-Duran et al., applied and validated a conceptual model to assess complexity in healthcare (20), based on the Multiple Chronic Conditions Research model from the University of Washington, that defines complexity as the “gap between patient needs and health care services” (33). The new conceptual model, Hexagon of Complexity (HexCom), comprises a total of 6 domains and 18 subdomains in the definition of complexity. The main domains identified (clinical, social/family, end-of-life, ethical decisions, spiritual, and psychological) are related to the available resources at the operative, intrapersonal, interpersonal, and transpersonal levels, being classified by the PC team as highly complex, moderately complex, and non-complex, as previously described (20).
Interestingly, around 47% of the included studies were performed/conceptualized in Spain. This fact may be attributed to the use of “complexity” as a criterion for access to specialized PC, after a fall from 5th to 11th place in the European ranking of PC in 2013 (34).
Integration of the different models
Although in 2018 Tuca et al. (22) have proposed a consensus definition of complexity in PC needs, based on a multidimensional model (“the clinical situation that depends on the interaction of the characteristics of the emerging symptoms, according to a multidimensional evaluation, that shows a special tendency to clinical instability, uncertainty in the result of the care intervention and to the subsequent need to intensify specialized measures of palliative support”), according to the present scoping review, the proposed definition is not universally recognized.
For more qualified, suitable, and comprehensive care of patients in need of PC, it is imperative to reach a universal consensus regarding the definition of complexity and its assessment.
The conceptual models of clinical complexity suggested in the literature were based on general clinical complexity models and adapted to be applied to PC. These models identify different domains for assessing the needs of patients and family members/caregivers, ranging from the patients’ “current” domains (physical, psychosocial, spiritual), to a “longitudinal” journey of pre-existing, cumulative and invisible complexity, which are directly or indirectly interconnected with the environment in all its dimensions: health services structure and level of development, specialized PC team characteristics, health policy, among others (12,13,20,29,31). Among the models found, the adaptive and multidimensional model described by Pask et al. (in 2018), which argues that the complexity of the PC patient may not rely on the type of diagnosis and/or prognosis, but it should comprise the assessment of the intrinsic needs of the patient and family, as well as the “complexity” perceived by the healthcare professionals who follow the patient (29). This model is thus assumed as a multidimensional and adaptive model that results in a constant evolutionary process, as defended by Hodiamont et al. (in 2019) (31). Further research, focused on the definition of complexity, and applicability to clinical practice and subsequent planning of health policies may benefit from this theoretical model (31,32).
The multidimensional model described by Busquet-Duran et al. (in 2020), where end-of-life care and social assessment and support are elements that should be considered in patients with high complexity, highlight the relevance of the socio-family domain, of the integrated care plan with the discussion of the place of death, and of the relationship and communication at the end of life (20).
The acknowledgement of an adaptive system is crucial to the development of future investigations on the assessment of complexity in PC, including instruments that can be adjusted to the stage of the disease (31). Evolution is thus the result of an adaptive system.
Figure 2 illustrates a fusion of the aforementioned models (22,30,31), developed by the authors of this review, in line with the evidence collected.
The assessment of the complexity of the intrinsic needs of the patient and family is easier to identify, compared to the assessment of the complexity that depends on the healthcare professionals, since the last depends on other factors, such as the level of experience of the professionals, and the availability of time to explore the multiple dimensions of the patient’s suffering (physical, psychological, social and spiritual) (32).
The conceptual model created can effectively be the basis for future research, mainly because it is the first model that links PC to the spectrum of severe diseases associated with multi-comorbidity. In addition, it identifies and suggests research gaps to strengthen the model and to be able to create a practical and viable model in clinical practice (13).
Busquet-Duran et al.’s (in 2020) study results show higher complexity in oncological patients with organ failure, compared to frail patients or with dementia (low complexity), suggesting that specialized PC teams should focus on patients with high complexity (20). High complexity in the socio-familial domain raises the need of patient assessment by the Social Worker, and of socioeconomic support, especially in patients with cancer with organ failure, where the availability of hospitalization in specialized units and the discussion of the preferred place of death, should be addressed in the first stages of contact with the specialized PC team. End-of-life care and social assessment and support should be present in patients with high complexity (20).
Instruments used to assess clinical complexity in PC
The second objective of this scoping review was to identify and map the instruments available and eventually applicable in clinical practice, in order to classify the complexity of patients with PC needs.
Although thirteen instruments were identified, only 4 (30.8%) were mentioned in more than one study (IDC-PAL n=4, HexCom n=3, PALCOM n=3, HUI Major Criteria n=2) (15-18,20-22).
According to Grant et al. (in 2021), most instruments show applicability limitations to the clinical reality (17), yet conclude that the HexCom and IDC-Pal showed to be the instruments that offer a broader determination of complexity from an personal perspective (17). This is in line with other authors, who characterize HexCom (and different instruments derived from it) as a useful tool in defining complexity in patients in need of PC (20,21); or the IDC-Pal as a valid instrument for the determination of complexity in PC (15), allowing the identification of factors related to clinical complexity, thus helping physicians to identify situations that require timely referral to specialized PC teams (16). PALCOM is also considered by some authors as a useful tool for the stratification of complexity in patients with PC needs (22).
Other instruments have been used and/or developed, although their use is less frequent. This is the case of the adaptation of the QDACT developed by Kamal et al. (in 2021) (23), which consider that patient characteristics, diagnosis and healthcare team characteristics, at the time of PC consultation request, are associated with the level of complexity; The PCPSS, an acceptable instrument with moderate reliability for determining the level of clinical complexity in patients with PC needs (14); or the ID-PALL, which allows the identification of the level of complexity of patients in need of generalist versus specialized PC (24). Among these, ID-PALL stands out, because although recent, it allows a broad determination of complexity, leveling it with HexCom and IDC-Pal.
In the presence of high levels of frailty, clinical complexity, and complexity in PC, distinct or interconnected instruments can be used. However, it may lead to an overlap of factors/dimensions that can compromise the prognosis and evaluation of symptoms accuracy (18).
The study design (i.e., scoping versus systematic review) may be considered one of the main limitations of the present study. Nevertheless, like a Systematic Review, the Scoping Review allows to summarize and disseminate the results of a bibliographic research, as well as to identify gaps in the literature on the analyzed topic (35). A Scoping Review, although it is a relatively recent approach to gather relevant information about broad topics, its use is becoming common, especially in topics of a heterogeneous nature, about which there is no idea of the extent of the literature that has been developed (36).
The small number and heterogeneity of the included studies may also be considered as limitations of the present review. Yet, these limitations were expected given the nature and scarcity of literature on the topic.
Despite these limitations, this study suggests a possible integration of the different dimensions in a single model (Figure 2), also gathering relevant information about the instruments used in the assessment of complexity, that could be used in clinical practice.
Conclusions
Complexity is a dynamic process, reflecting the reality of patients and family members, and its perception by patients, family members and healthcare professionals, and must be systematically adjusted to the stage of the disease, as illustrated in Figure 2. Services must therefore be flexible and adapt the response to the dynamic complexity of each person. However, the adaptability of the response depends on the characteristics of the healthcare professionals (i.e., training and experience). For this reason, training in PC is essential to provide healthcare professionals with essential tools for the recognition of patients with PC needs, as well as for the professional development and knowledge in complexity identification.
The conceptual models aim to guide the provision of PC, although more research is needed to investigate clinical complexity in patients with PC needs.
Among the instruments identified to assess complexity in PC, eventually applicable in clinical practice, the HexCom, IDC-Pal and the ID-PALL, seems to offer the broadest determinations of complexity, yet further investigation is needed regarding the adaptation and validation of these instruments to the clinical practice.
Additionally, the present scoping review suggest a need for systematic reviews on both topics, which may be able to provide support to a consensual definition of complexity, further contributing for instrument improvement.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA-ScR reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-22-894/rc
Peer Review File: Available at https://apm.amegroups.com/article/view/10.21037/apm-22-894/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-22-894/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Federal Office of Public Health. Framework for Palliative Care in Switzerland: A basis for defining palliative care for the implementation of the National Strategy for Palliative Care 2013-2015 Online. Available online: www.bag.admin.ch/palliativecare
- Comissão Nacional de Cuidados Paliativos (CNCP). Plano estratégico para o desenvolvimento dos cuidados paliativos biénio 2017-2018. Online. Available online: https://www.sns.gov.pt/wp-content/uploads/2016/09/Plano-Estrat%C3%A9gico-CP_2017-2018-1-1.pdf
- Peres R, Anjos A, Anjos Y, et al. O trabalho em equipe no contexto hospitalar: reflexões a partir da experiência de um programa de residência multiprofissional em saúde. Em Extensão. 2011;10:113-20.
- Bonavita V, De Simone R. Towards a definition of comorbidity in the light of clinical complexity. Neurol Sci 2008;29:S99-102. [Crossref] [PubMed]
- Ryan K. National Clinical Programme for Palliative Care Working Group. Role Delineation Framework for Adult Palliative Care Services. Available online: https://www.lenus.ie/bitstream/handle/10147/622898/role-delineation-framework-for-adult-palliative-care-services.pdf?sequence=1&isAllowed=y
- Magnani C, Peruselli C, Tanzi S, et al. Complessità e cure palliative. Rivista italiana di cure palliative. 2019;21:196-203. Available online: https://www.ricp.it/archivio/3225/articoli/32031/
- World Health Organization. Global Atlas of Palliative Care at the end of life. Available online: www.who.int/nmh/Global_Atlas_of_Palliative_Care.pdf
- Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med 2018;169:467-73. [Crossref] [PubMed]
- Booth A. Searching for qualitative research for inclusion in systematic reviews: a structured methodological review. Syst Rev 2016;5:74. [Crossref] [PubMed]
- Peters MD, Godfrey CM, Khalil H, et al. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc 2015;13:141-6. [Crossref] [PubMed]
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372: [PubMed]
- Carduff E, Johnston S, Winstanley C, et al. What does 'complex' mean in palliative care? Triangulating qualitative findings from 3 settings. BMC Palliat Care 2018;17:12. [Crossref] [PubMed]
- Murali KP, Merriman JD, Yu G, et al. An Adapted Conceptual Model Integrating Palliative Care in Serious Illness and Multiple Chronic Conditions. Am J Hosp Palliat Care 2020;37:1086-95. [Crossref] [PubMed]
- Masso M, Allingham SF, Johnson CE, et al. Palliative Care Problem Severity Score: Reliability and acceptability in a national study. Palliat Med 2016;30:479-85. [Crossref] [PubMed]
- Martin-Rosello ML, Sanz-Amores MR, Salvador-Comino MR. Instruments to evaluate complexity in end-of-life care. Curr Opin Support Palliat Care 2018;12:480-8. [Crossref] [PubMed]
- Carrasco-Zafra MI, Gómez-García R, Ocaña-Riola R, et al. Level of Palliative Care Complexity in Advanced Cancer Patients: A Multinomial Logistic Analysis. J Clin Med 2020;9:1960. [Crossref] [PubMed]
- Grant M, de Graaf E, Teunissen S. A systematic review of classifications systems to determine complexity of patient care needs in palliative care. Palliat Med 2021;35:636-50. [Crossref] [PubMed]
- Mota-Romero E, Tallón-Martín B, García-Ruiz MP, et al. Frailty, Complexity, and Priorities in the Use of Advanced Palliative Care Resources in Nursing Homes. Medicina (Kaunas) 2021;57:70. [Crossref] [PubMed]
- Comino MRS, Garcia VR, López MAF, et al. Assessment of IDC-Pal as a Diagnostic Tool for Family Physicians to Identify Patients with Complex Palliative Care Needs in Germany: a Pilot Study. Gesundheitswesen 2018;80:871-7. [PubMed]
- Busquet-Duran X, Jiménez-Zafra EM, Manresa-Domínguez JM, et al. Describing Complexity in Palliative Home Care Through HexCom: A Cross-Sectional, Multicenter Study. J Multidiscip Healthc 2020;13:297-308. [Crossref] [PubMed]
- Busquet-Duran X, Jiménez-Zafra EM, Tura-Poma M, et al. Assessing Face Validity of the HexCom Model for Capturing Complexity in Clinical Practice: A Delphi Study. Healthcare (Basel) 2021;9:165. [Crossref] [PubMed]
- Tuca A, Gómez-Martínez M, Prat A. Predictive model of complexity in early palliative care: a cohort of advanced cancer patients (PALCOM study). Support Care Cancer 2018;26:241-9. [Crossref] [PubMed]
- Kamal AH, Check DK, Bull J, et al. Associations of Patient Characteristics and Care Setting with Complexity of Specialty Palliative Care Visits. J Palliat Med 2021;24:83-90. [Crossref] [PubMed]
- Teike Lüthi F, Bernard M, Vanderlinden K, et al. Measurement Properties of ID-PALL, A New Instrument for the Identification of Patients With General and Specialized Palliative Care Needs. J Pain Symptom Manage 2021;62:e75-84. [Crossref] [PubMed]
- Esteban-Pérez M, Grau IC, Castells Trilla G, et al. Complejidad asistencial en la atención al final de la vida: criterios y nivelesde intervención en atención comunitaria de salud. Medicina Paliativa 2015;22:69-80. [Crossref]
- Radbruch L, De Lima L, Knaul F, et al. Redefining Palliative Care-A New Consensus-Based Definition. J Pain Symptom Manage 2020;60:754-64. [Crossref] [PubMed]
- Saunders C. The evolution of palliative care. J R Soc Med 2001;94:430-2. [Crossref] [PubMed]
- Schaink AK, Kuluski K, Lyons RF, et al. A scoping review and thematic classification of patient complexity: offering a unifying framework. J Comorb 2012;2:1-9. [Crossref] [PubMed]
- Pask S, Pinto C, Bristowe K, et al. A framework for complexity in palliative care: A qualitative study with patients, family carers and professionals. Palliat Med 2018;32:1078-90. [Crossref] [PubMed]
- Gómez-Batiste X, Porta J, Tuca A, et al. Organización de Servicios y Programas de Cuidados Paliativos. 1 ed: Arán Ediciones, 2005.
- Hodiamont F, Jünger S, Leidl R, et al. Understanding complexity - the palliative care situation as a complex adaptive system. BMC Health Serv Res 2019;19:157. [Crossref] [PubMed]
- Mainzer K. Thinking in Complexity. 5 ed. Berlin Heidelberg,: Springer-Verlag, 2007. XVIII, 482 p.
- Grembowski D, Schaefer J, Johnson KE, et al. A conceptual model of the role of complexity in the care of patients with multiple chronic conditions. Med Care 2014;52:S7-S14. [Crossref] [PubMed]
- Woitha K, Garralda E, Martin-Moreno JM, et al. Ranking of Palliative Care Development in the Countries of the European Union. J Pain Symptom Manage 2016;52:370-7. [Crossref] [PubMed]
- Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5:69. [Crossref] [PubMed]
- Pham MT, Rajić A, Greig JD, et al. A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods 2014;5:371-85. [Crossref] [PubMed]



