
Improving timely transfers from acute care to the local palliative care unit for patients at the end of life
Highlight box
Key findings
• In this quality improvement initiative, standardizing a transfer process improved patient transfer times from acute care to a palliative care unit by 29% (from 180.2 to 128.3 min; P<0.003).
What is known and what is new?
• Despite the majority of Canadian’s wishing to die at home, most continue to experience end-of-life in hospital; creating a strain on the health care system.
• Initiatives that help address hospital occupancy have recently been encouraged.
• Improving the timely transfer of patients at end-of-life from acute care to a palliative care setting can be a useful initiative to address hospital occupancy issues. This is a complex processes requiring the commitment of multiple stakeholders.
What is the implication, and what should change now?
• Improved transfer times can correspond to cost savings and reduced acute care wait times.
• Expanding the outlined initiative across the organization will amplify its benefits to patients and the health care system.
Introduction
Honouring a patient’s wish for their preferred location of death is an essential component in end-of-life care (EOLC). A recent survey revealed that despite the fact that 2/3 of Canadians have expressed a preference to die at home, the majority die in an acute care setting (1). In addition to that, patients nearing the end of life (EOL) prioritize adequate symptoms management and being surrounded by loved ones regardless of their care setting. Thus, patients who choose to be cared for in another setting such as a palliative care unit (PCU), should be able to transition to their setting of choice with ease and with their loved one present. For this reason, it is imperative that health care systems align their processes to allow for safe and timely transfers. Effective interventions have many benefits such as reducing patient’s length of stay in hospital referred to as Alternative Level of Care (ALC) days in Ontario, Canada hospitals, in addition to ensuring the most optimal end of life care experience is achieved. Prolonged acute care stays are a major contributor to poor acute care bed utilization (2). A previous study has shown that delays in transfers from acute care were associated with increased ALC bed occupancy, increase healthcare cost and contributed to the inability to repatriate patients to other settings (3). Noted by the Ontario Hospital Association (2019) was the growing number of ALC patients remaining in hospital longer when services were inaccessible or unavailable (4). Such delays are known to be costly to the healthcare system. At the local level, those patients that are impacted greatly by such delays are those in the emergency department. Patients in the hospital emergency department are often waiting between one to three days before being transferred to an acute care unit. Such delays have consistent effects on patient care. Therefore these inefficiencies and gaps in the delivery of care supports the need for a transformative approach to improving patient flow and transfer processes within the organization (5). An interprofessional team thus embarked on a quality improvement project to help improve transitions at EOL.
Local context
This hospital is a tertiary care centre that is associated with a PCU that is geographically adjacent to the main hospital building and operationally and administratively separate from acute care. The PCU is a 56-bed inpatient unit with a mandate to provide comprehensive EOLC for patients with a prognosis of <3 months. Of the 56 beds, the unit also reserves a few beds for patients adopting a palliative approach to care with a longer prognosis of one year or less. The PCU accepts referrals from all acute care units in hospitals across the province of Ontario, Canada.
The organization did not have a standardized time or process for patients transferring from acute care to PCU. However, there is a standardized application that needs to be submitted to the administrative staff of the PCU for review prior to admission. Once the application is approved, the social worker is informed of acceptance and is provided with a bed offer. Once a bed offer was accepted by the patient and family, the discharge from the General Internal Medicine (GIM) unit (C6) to the PCU could take on average between one to six hours to complete.
A limiting factor to timely transfers is the institution’s current hybrid medical record system. In this system, any patient admitted in acute care has an electronic medical record chart that allows for viewing of clinical notes and test/laboratory results, as well as a physical chart in the form of a binder on the admitted unit in which nursing daily observations and physician orders are written.
The aim of this quality improvement project was to establish a standardized, safe and efficient patient transfer from GIM (C6) unit to the PCU for a standard arrival time of 10 am, Monday to Saturday, by May 2020.
An inter-professional quality improvement (QI) team was formed to analyze the transfer process for patients. Several change cycles were tested, targeting all steps of the transfer process. A turnaround time of two hours was set as the target (time between bed offer to the actual PCU transfer). This target time was set in collaboration with the PCU physicians and due to confounding factors such as pharmacy hours.
Methods
Project design
This project was a time series in accordance with the Standards for Quality Improvement Reporting Excellence Guidelines 2.0 (5) and used a lean six sigma improvement framework (6-8). Inclusion criteria where GIM and oncology patients on C6 who had a prognosis of <3 months and a preference for the EOLC to take place in a PCU. Baseline data was collected between September 2019 and March 2020 (Table 1).
Table 1
| Timeline | Intervention | Details |
|---|---|---|
| September 2019 | Start of QI project | • Identification of the problem through chart reviews and analyzing arrival time of the patient • Assemblage of a QI team |
| Project charter | ||
| October 2019 | Root cause analysis | • C6 team and PCU team met to complete current state and future state process mapping • SW shadowed Residents from 7 am – 6 pm • Worked with patients and families to find a mutually agreed upon transfer time |
| Ischikawa and driver diagrams | ||
| Process Mapping | ||
| Direct Observation | ||
| Collection of qualitative data | ||
| November 2019 | Stakeholder engagement | • Working with our PCU colleagues, Residents/Staff MD’s, Porters and C6 RN’s, patients and families • Dotmotcracy |
| Co-designing pre-discharge orders with physician’s (MD’s) and RN’s and transfer time with patients and families | ||
| December 2019 | PCB | • Designed and completed PCB • Outcome measure: # of patients that arrived to the PCU by 10 am/2-hour turnaround time • Process measures: (I) % of patients with pre-discharge orders, (II) % of patients with pre-discharge summaries, (III) % of Porters who arrived at the designated time, (IV) % of Families who accompanied their loved one to the PCU |
| Family of measures established | ||
| January to February 2020 | PDSA cycles | • PCB used for on every PCU transfer |
| March 2020 | C6 team deployed to the COVID-19 unit | • Project on hold, although some COVID-19 patients were transferred to the PCU |
QI, quality improvement; PCU, palliative care unit; SW, social worker; RN, registered nurse; PCB, Process Control Board; PDSA, Plan-Do-Study-Act.
Ethical statement
Ethical considerations for this QI project were assessed through Sunnybrook Research Ethics Board -Self-Assessment Tool and were deemed to not require a full Research Ethics Board review.
Improvement framework
A Lean Six Sigma framework was adopted for this QI project. Lean Six Sigma in healthcare is an improvement framework focused on eliminating waste and variation of a process, with a general goal to improve efficiency and achieve standardization. This lens was used in this QI project to design the standardized transfer process between the GIM (C6) acute care unit and PCU (6-8).
Consistent with continuous QI project methodology, small cycle changes were designed and implemented in an incremental way via Plan-Do-Study-Act (PDSA) cycles (9). In this framework, each suggested intervention/change was initially tested on a small scale and evaluated prior to being fully implemented on the unit. Moreover, once the interventions were implemented, the fidelity and effectiveness of the implemented measures were continuously evaluated via the established process measures. Lastly findings were used to inform the immediate next steps in the project in order to improve fidelity of the implemented changes.
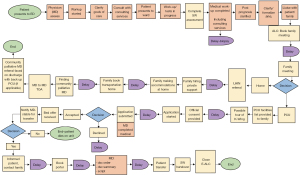
Root cause analysis
To address the domains of efficiency and timelines, the PCU transfer process for a patient was mapped from initial entry point (emergency department) to the PCU (Figure 1). The most common reasons for the delays were: (I) waiting for the discharge order and summary, (II) delay in booking the porter, (III) waiting for family to arrive on the unit to accompany their loved one to the PCU.
Healthcare providers both on the PCU and GIM (C6) units were interviewed to elicit their perspectives on how transfers and admissions impacted their daily workload.
Interventions to reduce transfer times
To address the root causes, the following four interventions were introduced.
The first change involved the implementation of pre-discharge orders written by a GIM physician the night prior to the day the patient transfer was to take place (Appendix 1). This change concept was co-designed with the relevant stakeholders including residents, staff physicians and nurses. Lean methodology was used to conduct direct observation of a resident’s work flow to ensure feasibility of this change.
The second change involved the implementation of a standard booking time with the Portering Service for 9:30 am pick-up. Portering Service Manager was engaged early on in the stakeholder process and was part of the direct observation flow process map.
The third and fourth change in the process was the social worker informing the patient’s family/next of kin ahead that the transfer time to the PCU would take place at 9:30 am. This information allowed families/next of kin to plan accordingly and be available for the transfer. The 9:30 am transfer time was established based on survey results [ten families; PCU colleagues (five nurses, three physicians, and manager)].
Family of measures
A family of measures including outcome, process and balancing was collected and used to inform successive PDSA cycles. The project’s outcome measure is the percentage of patients who arrive at the PCU at new standard time for 10:00 am (two-hour turnaround time).
Process measures included:
- Percentage of pre-discharge orders written;
- Percentage of pre-discharge summaries place on the patients chart the day before a potential bed offer;
- Percentage of Porters arriving to the unit by the new standard time for 9:30 am pick-up time;
- Percentage of families accompanying their loved one to the PCU by 9:30 am.
Balancing measure included:
- Family/next of kin that wanted to accompany their loved one, yet couldn’t make it for the 9:30 am transfer and transfer proceed without accompaniment.
Data collection
Data was collected prospectively between January to June 2020. A process control board (PCB) was used for data collection and continuous evaluation of the transfer process. In accordance with the above described lean six sigma methodology, a process control board is a tool that can be used to monitor existing operational processes with an aim to improve the process by eliminating waste (5,7). The “Comments” column captures any divergence of the transfer process (5).
Statistical analysis
Statistical process control charts were used to analyze data to determine the degree and sustainability of any identified change (Appendix 2). Two sample t-test were used to determine statistical significant in change, in transfer times before and after the intervention bundle.
Results
Outcome measure
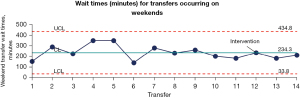
During the duration of the project, a total of 12 weekday transfers occurred and a total of two weekend transfers occurred over a six months period. Average turnaround time during the week was reduced from a baseline average of 180.2 to 128.3 minutes (P<0.003). This change was found to be statistically significant and sustained (Figure 2). The average transfer time on weekends remained stable at 234 minutes (Figure 3).

We achieved the outcome target of a 10:00 am arrival time to the PCU 42% of the time. Improvement to transfer times become apparent when patients’ families were preemptively prepared for the 9:30 am transfer; noting it was successful 86% of the time. Early engagement of family members allowed the nurse to focus on the necessary discharge steps, i.e., dismantling the paper chart, gathering medications, providing telephone handover to the admitting unit (PCU nurse), supporting the porter with the physical transfer, and attending to the patients’ physical and emotional needs prior to discharge.
Process measures
Several metrics were monitored as process measures in the project. This included the percentage of pre-discharge orders written, the percentage of pre-discharge summaries placed in the patients’ chart the day before a potential bed offer. The percentage of Porters arriving to the unit by the new standard pick-up time of 9:30 am, and the percentage of families accompanying their loved one to the PCU.
Of the 20 EOLC patients who had an anticipated discharge date to the PCU during the study period, 45% had a pre-discharge order and pre-discharge summary. Upon review of the cases, six of them were potentially eligible for transfer, however tested positive for the coronavirus disease 2019 (COVID-19) and therefore became ineligible at that time. Hence, these patients had to remain on GIM (C6) due to hospital’s infection control policies; leaving a total of 14 eligible patients for transfer to the PCU. Sixty-four percent of the 14 patients had a pre-discharge order and summary in the chart and of this group, 57% had a porter arrive at 9:30 am. All substitute decision makers of 14 patients were notified ahead of the planned transfer time to the PCU.
Discussion
This improvement project showed that standardizing patient transfer processes can reduce transfer times for patients from an acute care unit to the PCU. Particularly noting an improvement with the average turnaround time on weekdays. Transfer times were decreased by 29% (from 180.2 to 128.3 min; P<0.003) with the implementation of the following processes: an established discharged time, a pre-booked porter, pre-arranged family notification and option to accompany transfer, and physician discharge orders. There was less favorable improvement during weekend transfers with transfer times remaining stable at 234 min. It is noteworthy that only two weekend transfers occurred after the implementation of the transfer process changes and thus, there are not enough data points to truly reveal any change in this setting. Associated factors that could have potentially impacted transfer times on weekends include the reduced hospital staff (social worker and portering). More specifically, weekends do not have a dedicated social worker on the unit to help facilitate transfers and discharges. These two compounding factors may have contributed to the lack of improvement in timely weekend transfers. Further exploration of these factors are required.
Significant strain currently exist on hospitals as the majority of Canadians (60%) die in hospital (10). Therefore, there is an urgent need to ensure patients are dying in their preferred place of death. When contemplating their preferred place of death, individuals often prefer to be at home or transition to a home-like environment, i.e., hospice or PCU. Very rarely do individuals state their preferred place of death to be in hospital, given the often loud and unwanted noises within this setting, which ultimately impacts quality of life and EOLC (11). Improving the EOLC experience of patients in acute care has been highlighted as an area for quality improvement in the literature (12). This has been an area of interest for this organization for many years and in fact lead to the development of the Quality Living and Dying Initiative (QLDI) a decade ago (13). Part of delivering high quality end of life care is also addressing transitions across settings (14) and ensuring they are completed in a timely manner and with the least amount of distress to patients and their families (15).
All QI work requires the commitment of an interprofessional team. Most specifically this QI project came to flourish through the leadership role of the social worker within the GIM (C6) unit. The psychosocial assessment conducted by social work with each patient and family helped elicit the needs of the patients and families on this unit (16,17). This included the concurrent theme from patients and families that they wanted their loved ones for their transfer to the PCU. This request did not come as a surprise as it is not uncommon for patients to experience a number of challenges during transitions; specifically feelings of uncertainty (14). Social workers through their advocacy role working with patients and families are well positioned to help facilitate the necessary improvements needed to strengthen transitions across the health care system (12,18).
Patients in today’s health care system would prefer a home death (19). However, many factors impact this desired outcome (20,21), such as the patient’s condition, their caregiver’s situation, lack of home palliative supports, and at times require an emergency visit followed by an admission to hospital to await a transfer to a PCU or hospice (22). As such, the emergency department (ED) for many, may be a first point of contact when critically unwell. Therefore, ensuring the availability and sustainability of medical support is crucial to the wellbeing of all patients and their families (23). Initiatives that help address hospital occupancy and streamlining transitions across settings has been encouraged by the health care system. According to the internal 2020 Powerbase Balance Index Data dashboard, the ED had an average of 175 patients/day. For patients who required a hospital admission, their average ED length of stay was between one to three days. During that time period it was not uncommon to have patients who were also at end of life (24). These EOLC patients are categorized as alternate level of care (ALC) patients—that is, patients awaiting a transfer to an alternate location. It has been noted that having patients who are close to end of life and are waiting in hospital for their final destination in not a good use of hospital bed utilization. Specifically in Canada, Ontario ALC patients and have become a growing population of concern. In the fiscal year 2017/2018, provincial data revealed there were 190,000 ALC patient days and 40% of all ALC patients were patients in their last three months of life. More specifically, of the 40% of all ALC patients, approximately 24% represented patients awaiting transfer to a PCU or hospice (25). Delays in transferring patients from one location or setting to another is a significant contributor to the number of ALC days accumulated. This QI initiative of transferring patients to PCU from GIM (C6) within a two hour time frame can help mitigate time spent in ED. Salifu & Bayuo’s, 2022 article encourages palliative care stakeholders to invest the time needed to improve transition processes (14). This project is timely in responding to this call for action in reducing ALS days and health care cost (26). In fact, this QI project was successful as it achieved a 57% decrease in hospital cost of ALC patients. At the unit level, this streamlined transfer process corresponded to savings of $6,000.00/year. The QI team plans to expand this project on a larger scale with the hopes of reaping greater hospital savings.
Limitations
This QI project presents with several limitations, starting with a small sample size. Secondly, six months into the project, the World Health Organization announced the COVID-19 pandemic impacting the full scope of this project as hospital transfer policies change due to infection control purposes.
Thirdly, this initiative is unique to this large tertiary care hospital as it is affiliated with a PCU. Several Canadian hospitals do not have a designated PCU within its institution (15); therefore, the generalizability of this QI project may be limited to other organizations without a PCU.
Conclusions
With the lack of hospice/palliative care beds in the province of Ontario, Canada wait times for EOLC patients in hospital continue to be an issue. Therefore, this project highlights the utility of standardizing transfer times to improve access and ensure a seamless transition. Institutions can consider adapting such process measures to improve their own palliative care transitions across settings. Such processes are complex and require the commitment of multiple stakeholders and time to reduce acute care wait times, improve bed flow, and in turn reduce health care costs.
Acknowledgments
Lois Fillion-RN, BScN, MHSc; Jocelyn Charles MD; Kaveh Shojania MD; Dominick Shelton MD, MSc, CCFP (EM); Fanchea Lau- BSc.
Funding: None.
Footnote
Data Sharing Statement: Available at https://apm.amegroups.com/article/view/10.21037/apm-22-1257/dss
Peer Review File: Available at https://apm.amegroups.com/article/view/10.21037/apm-22-1257/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-22-1257/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy of integrity of any part of the work are appropriately investigated and resolved. Ethical considerations for this QI project were assessed through Sunnybrook Research Ethics Board -Self-Assessment Tool and were deemed to not require a full Research Ethics Board review.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tepper J. Palliative Care at the End of Life. 2016: Health Quality Ontario.
- Alali H, Kazzaz Y, Alshehri A, et al. Reducing unnecessary delays during the transfer of patients from the paediatric intensive care unit to the general ward: a quality improvement project. BMJ Open Qual 2019;8:e000695. [Crossref] [PubMed]
- Rojas-García A, Turner S, Pizzo E, et al. Impact and experiences of delayed discharge: A mixed-studies systematic review. Health Expect 2018;21:41-56. [Crossref] [PubMed]
- Ontario Hospital Association. A balanced approach: the path to ending hallway medicine for Ontario patients and families. Pre-budget submission 2019 Ontario budget.
- Ogrinc G, Davies L, Goodman D, et al. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): revised publication guidelines from a detailed consensus process. Am J Med Qual 2015;30:543-9. [Crossref] [PubMed]
- NHS Institute for Innovation and Improvement. Lean Six Sigma: some basic concepts.
- Bercaw RG. Lead Leadership for Healthcare: Approaches to Lean Transformation. New York: Productivity Press; 2013.
- Bercaw R. Taking Improvement from the Assembly Line to Healthcare. Boca Raton, Florida: CRC Press; 2012.
- Leis JA, Shojania KG. A primer on PDSA: executing plan–do–study–act cycles in practice, not just in name. BMJ Quality & Safety 2017;26:572-7. [Crossref] [PubMed]
- Stilos KK, Moore JD. How COVID-19 has changed the dying experience for acute care patients and their families. Can Oncol Nurs J 2020;30:218-9. [PubMed]
- Hsu AT, Garner RE. Associations between the receipt of inpatient palliative care and acute care outcomes: A retrospective study. Health Rep 2020;31:3-13. [PubMed]
- Stilos K, Takahashi D, Nolen AE. The role of the social worker at the end of life: paving the way in an academic hospital quality inprovement initiative. Br J Soc Work 2020;51:246-58. [Crossref]
- Stilos K, Wynnychuk L, DasGupta T, et al. Improving end-of-life care through quality improvement. Int J Palliat Nurs 2016;22:430-4. [Crossref] [PubMed]
- Salifu Y, Bayuo J. Transfer and transitioning between palliative care settings. Ann Palliat Med 2022;11:3035-9. [Crossref] [PubMed]
- Bottoms J, Nolen A, Moore J, et al. Factors that Delay Transfers from Acute Care to a Local Palliative Care Unit. Healthc Q 2022;25:36-41. [Crossref] [PubMed]
- Bosma H, Johnston M, Cadell S, et al. Canadian social work competencies for hospice palliative care: a framework to guide education and practice at the generalist and specialist levels 2008. Available online: http://cms.virtualhospice.ca/Web/CVH/Assets/Social_Work_Competencies_July_2009_20150708134353.pdf
- Bomba PA, Morrissey MB, Leven DC. Key role of social work in effective communication and conflict resolution process: Medical Orders for Life-Sustaining Treatment (MOLST) Program in New York and shared medical decision making at the end of life. J Soc Work End Life Palliat Care 2011;7:56-82. [Crossref] [PubMed]
- Gwyther LP, Altilio T, Blacker S, et al. Social work competencies in palliative and end-of-life care. J Soc Work End Life Palliat Care 2005;1:87-120. [Crossref] [PubMed]
- Cai J, Zhang L, Guerriere D, et al. Where Do Cancer Patients in Receipt of Home-Based Palliative Care Prefer to Die and What Are the Determinants of a Preference for a Home Death? Int J Environ Res Public Health 2020;18:235. [Crossref] [PubMed]
- Salifu Y, Almack K, Caswell G. 'My wife is my doctor at home': A qualitative study exploring the challenges of home-based palliative care in a resource-poor setting. Palliat Med 2021;35:97-108. [Crossref] [PubMed]
- Mertens F, Sercu M, Derycke A, et al. Patients' experiences of transfers between care settings in palliative care: an interview study. Ann Palliat Med 2022;11:2830-43. [Crossref] [PubMed]
- van Doorne I, van Rijn M, Dofferhoff SM, et al. Patients' preferred place of death: patients are willing to consider their preferences, but someone has to ask them. Age Ageing 2021;50:2004-11. [Crossref] [PubMed]
- Bayuo J, Anago EK, Agyei FB, et al. "Resuscitate and Push": End-of-Life Care Experiences of Healthcare Staff in the Emergency Department - A Hermeneutic Phenomenological Study. J Palliat Care 2022;37:494-502. [Crossref] [PubMed]
- Amado-Tineo JP, Oscanoa-Espinoza T, Vásquez-Alva R, et al. Emergency Department Use by Terminally Ill Patients: A Systematic Review. J Pain Symptom Manage 2021;61:531-43. [Crossref] [PubMed]
- C.D. Howe Institute. Expensive endings: reining in the high cost of end-of-life care in Canada. October 21, 2021.
- Office of the Auditor General of Canada. 2014 Fall Report of the Auditor General of Canada. Available online: https://www.auditor.on.ca/en/content/annualreports/arreports/en14/308en14.pdf


