
Economic impact of informal care of cancer patients at the end of life
Highlight box
Key findings
• Incorporating a Home Palliative Care Service is cost-saving from the health system and society’s perspective (including direct and indirect costs).
• The cost of informal care represents 82% of the total cost of palliative care (PC), for the Río Negro society.
What is known, and what is new?
• It has been published that home PC decreases the days of hospitalisation in the last year of life and increases the percentage of death at home.
• It is known that the provision of PC services has a heterogeneous distribution in Argentina and worldwide.
• We found that informal care represents the largest share of total PC spending in a province of Argentina.
What is the implication, and what should change now?
• Quantifying the incremental costs (savings) and health results of implementing an organised PC service could encourage different jurisdictions to expand their network of providers of these services, presenting heterogeneous coverage throughout Argentina.
Introduction
Background
Palliative care (PC) at the end of life is an essential aspect of health policies since it concerns suffering, dignity, care needs and people’s quality of life (1). PC improves the quality of life of patients and their relatives when they face problems inherent to a life-threatening disease (2-7). Although expressly recognised in the context of the human right to health (8), significant differences are observed in the way in which PC services are organised in health systems and in the access that individuals have to them (9-11). It is estimated that only 14% of people who need PC worldwide receive it (12). Only 19% of the countries have some integration of PC services as a conventional health service provided by health systems (9). This integration is central to strengthening patient-centred care and universal health coverage (13). The Atlas of Palliative Care in Latin America (14) provides an overview of the status of PC in the region regarding policies, drug availability, education and implementation of services. It finds an essential heterogeneity in the provision of PC services between the different countries.
A recent study from Chile shows that people with a cancer diagnosis had PC access with financial protection, accounting for almost 42% of patients in need (15). This research provides an empirical approach for applying the Lancet Commission’s serious health-related suffering framework to estimate the cost of achieving national universal PC access anchored in a package of health care services (16). A study (10) on the degree of development of PC services in Argentina found large differences between jurisdictions.
Economic evaluations (EE) are comparative studies of the effects on health and costs between two or more health technologies (17). These seek to offer help on how the best options can be chosen objectively and systematically, including the opportunity cost. The economic analysis of the incorporation of PC programs lets us evaluate the potential financial impact of moving the activity from the secondary care sectors to the primary, community and social care sectors, since it allows funders to estimate the variation in the costs of each subsector that funds these services, including patients and/or their families.
Various studies have analysed PC services’ costs and use of resources at the end of life (2,18-23). These costs and resources can be seen from the perspective of the funder (public health, social security or private insurance) or the perspective of society and thus include other expenses that the families and the community environment of the patient must bear. A problem in the analysis of the costs of community care is the incorporation of the costs of care provided by informal caregivers, which is the care that patients receive in their own homes from relatives or friends who are not paid for the care they provide. The economic repercussions of caregiving, which falls mainly on women, remain relatively neglected at the policy and research level.
The visibility of care tasks has gained relevance in theoretical and political problematisation in recent years. Care includes those tasks necessary to maintain daily life and its intergenerational reproduction. The concept of care involves both the set of practices that constitute the material and physical action of caring and the concern, interest, affection and attention that falls on those who, for different reasons, require care (24).
The distribution of tasks related to the care economy is crossed by gender inequality and is characterised by an unfair social organisation where women carry out greater unpaid workloads (25,26). It is estimated that 90% of women in Latin America participate in unpaid care tasks and housework, spending twice as much time as men on these tasks (27). In Argentina, women have a 55% higher participation rate in unpaid care tasks than men, while they spend almost twice as much daily as men on such tasks (28).
For this reason, progress towards a development agenda based on economic, social and environmental sustainability must incorporate the care concept with a gender perspective to ensure structural change within the inclusive growth framework (29).
Rationale and knowledge gap
In general, EE do not recognise care tasks in the generation of value, resulting in an undervaluation of informal care (30). Particularly, in EE of PC, little attention has been paid to identifying and measuring the costs incurred by patients and their caregivers (31). Most of the published works analyses home care only in terms of what is financed by the public subsector, using the perspective of the funder-financier (2,19-23,32,33). The social perspective (SP) includes the direct costs of the funder and the indirect costs borne by society. In this sense, the SP captures the family costs of informal care, while the funder’s perspective (FP) ignores this cost. Few works incorporate the SP in the economic analysis of PC (34-38).
The importance of family caregivers has been recognised within PC (39). It is unpaid work, which is generally confused with a lack of value (40).
Care is based on effective and kinship relationships belonging to the private level, which takes place in the domestic sphere and, as such, remains hidden from the public field (39).
In particular, the economic repercussions of care in a PC context remain relatively neglected at the policy and research level (41). Informal care is associated with important costs from the perspective of society since parents, children, partners, friends and other family members reduce their working hours or directly stop working and/or spend a significant proportion of their leisure time providing informal care (42). In this sense, the recommendations of the Second Panel on Cost-Effectiveness in Health and Medicine highlight the importance of including the implications of informal care in EE developed from the perspective of society (43).
The cost-effectiveness analysis of PC has not yet been studied in Argentina. However, important studies have been developed concerning the evaluation of PC modalities (44-50).
Objective
The objective of this work is to estimate and make visible the economic impact of unpaid care tasks within the framework of the EE of incorporating an organised home PC program for cancer patients at the end of life from a SP in the Rio Negro province of Argentina. We present this article in accordance with the CHEERS reporting checklist (51) (available at https://apm.amegroups.com/article/view/10.21037/apm-23-240/rc).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Commission on Ethics and Evaluation of Research Projects in Human Health of the Province of Río Negro (Resolution MS No. 4974/18) and was incorporated into the National Registry of Health Research (No. IS002450). Individual consent for this retrospective analysis was waived.
A cost-effectiveness Markov model was developed using the TreeAge Pro Healthcare software Version 2021, R1, simulating end-of-life care and resource use in a cohort of cancer patients admitted to a home-based PC program compared to the usual care (UC) received by a cohort of patients in their last year of life.
Study population and setting
The population included in the study are cancer patients at the end of life who do not have any other health coverage and are attended by the public health system of Río Negro. This province is located in the Patagonia region of Argentina and has a population of 728,403 inhabitants (52). Cancer is the second leading cause of death in this province with 1,033 deaths in 2018 (53). The public health system covers 26.9% of the population exclusively (54), while the rest have some form of private or social security coverage. We assume that the cohort of patients entering the model is made up of the 278 patients who died of cancer and has exclusively public health coverage.
Comparators
The economic model compares the provision of PC through a home-based program that operates in Cipolletti Hospital, a high-complexity public hospital that serves as head of the health zone in the province of Río Negro, with the UC that patients receive at the end of life. The latter represents a scenario in which patients receive medical, nursing and day-hospital consultations, use certain support medical equipment and receive informal care from family and/or friends. The UC aims to control symptoms and complications of cancer but does not address the holistic needs of patients and their families.
Perspective
The aim of the analysis was to estimate the social costs of end-of-life care from two perspectives: the FP, which includes the direct costs incurred by the provincial health subsystem, and the SP, which also includes the indirect costs borne by patients and their families. The model estimated the average cost per patient in both scenarios. Since the time horizon was of one year, the discount rate was not applied for costs or health outcomes. The effectiveness outcomes used were the number of days spent at home in the last year of life and the proportion of deaths that occurred at home. These outcomes were chosen based on the literature that shows the preferences of terminal patients to die at home rather than in a hospital (55,56).
The study protocol was approved by local Bioethics Committees and incorporated into the National Registry of Health Research under number IS002450.
Patients entered the model in the “Usual Care” state and remained in that state or changed to the “PC Program” or to the “Hospital Admission” states, as described in Figure 1.
Transition probabilities (the possible changes of state) were estimated from published literature (19,21) and validated by local experts (Table 1). In the Intervention branch, it was assumed that patients would spend 245 days in the “home care” status and that they entered the PC Program in their last 120 days of life, given the average value of permanence in the program according to statistics of the PC Service of Cipolletti Hospital. Transition probabilities were assumed to remain stable throughout the last year of life and not affected by each patient’s specific history of transitions.
Table 1
| Transition probabilities | Value | Range | Source |
|---|---|---|---|
| Home care to emergency call (UC) | 0.01000 | 0.00675 to 0.01326 | Pham B, Krahn M (21) |
| Hospital admission due to emergency care that comes from Home Care (UC) | 0.55917 | 0.47667 to 0.64167 | Pham B, Krahn M (21) |
| Continue hospitalization after spending the last day in the hospital (UC) | 0.91304 | 0.61538 to 0.95098 | Calculated from Hatziandreu et al. (19) |
| Home care to emergency call (PC) | 0.00610 | 0.00412 to 0.00809 | Pham B, Krahn M (21) |
| Hospital admission due to emergency care that comes from Home Care (PC) | 0.55917 | 0.47667 to 0.64167 | Pham B, Krahn M (21) |
| Continue hospitalized after spending the last day in the hospital (PC) | 0.90476 | 0.6875 to 0.94382 | Calculated from Hatziandreu et al. (19) |
UC, usual care; PC, palliative care.
Each patient could only be in one state each day. Patients progressed through the model in 1-day cycles for 365 days. All patients were at the end of life and “alive” in the model for 365 days and death occurred on day 366. Costs associated with the different types of care were obtained from Tariff lists of healthcare practices (57) and from the information of the Ministry of Health of Río Negro. The total cost of care of cancer patients in their last year of life was derived from this information combined with the time the cohort spent in each state.
Costs
The cost analysis was carried out from a SP, including the health system’s direct costs and informal caregivers’ costs. The information on the use of resources was obtained from the literature (19,21,58). It was validated and adjusted by key informants and referents in PC who work in the different health subsectors included in the study. All costs were calculated for the year 2019 in American dollars, according to the official exchange rate (Banco Nación Argentina, July 1, 2019, US$ 1 = $Arg 43.40).
The calculation structure of PC services costs was made based on a theoretical definition of the makeup of PC service of the Cipolletti Hospital, which is shown in detail in the Appendix 1. To get to the direct daily cost per patient, from de funders perspective, we divided the monthly cost by 30 days and by the 81 patients that were cared for by the service each month.
This information was validated and complemented with published literature on resource use and costs in PC services at the end of life (58-60). The results were validated by experts involved in the management and provision of PC services.
Unpaid informal care costs
The SP includes the indirect costs that fall on the patient and their family. To address this concept, the cost of informal care required by patients when they are cared for at home was incorporated. For the estimation of the economic value of informal care, various methods have been published and were previously discussed (61). The most frequently used method is the” next best” method and the “opportunity-cost” method (62). In the first case, care hours are valued at the market price of the tasks considered to be the closest substitute in the market. In this way, care tasks are considered and valued as work. The opportunity-cost method values informal care time as its opportunity cost from the perspective of the caregiver (42). According to Posnett, it is preferable to use this last method since the resources (such as the time assigned) must be valued according to the opportunity cost that they represent for society (63).
Informal care time was valued using the human capital approach (64). This method requires knowing the number of hours of informal care and a salary assigned as the monetary value of the substitute in the market (38,65). The estimate of the number of hours assigned to caring for cancer patients at the end of life was obtained from published literature (38,65-67). The gross market salary was taken as the opportunity cost for the allocation of the monetary value of the time dedicated to care tasks. In that case, we used the median of the gross remuneration of registered employees in the private sector, surveyed by the Employment and Dynamics Observatory of the Ministry of Labour, Employment and Social Security for July 2019 (68). To obtain the value per hour, the monthly remuneration was multiplied by 13 months (in order to incorporate the complementary annual salary), and then divided by 52 weeks and by 44 hours of weekly work for a formal worker. The average gross remuneration of registered employees of the private sector in Argentina was considered, which was USD 817 (68), and the number of hours per week dedicated to caring for patients at the end of life was obtained from published literature (38,66,67).
Different authors evaluated the monetary value of informal caregivers of cancer patients at the end of life and identified the weekly hours dedicated by families: Urwin (38) estimated 93.07 h. Wolff (67) estimated 43 h and Brick (66) estimated 29.28 h per week. We decided to use the number of informal care hours reported by Wolff et al. (67), because it is similar to the results of the “Time Use Survey in Argentina” that reports 6 hours a day of care provided by women (69).
Cost of UC
The UC represents a scenario in which the patient at the end of life receives medical, nursing and day-hospital consultations, and uses certain support medical equipment. A patient receives informal care from family and/or friends, which is assumed to be for 6 hours a day. We considered the results obtained by Coyle et al. (58) regarding the use of services per patient in the week before and after admission to the study and were extrapolated to one year. The annual cost was calculated, by multiplying the number of consultations and stays in day-hospital by their respective unit costs, according to the Tariff list of the Province of Neuquén (57).
It was incorporated the cost of supporting medical equipment necessary to improve the comfort of patients at home, using the results presented by Coyle et al. (58) to estimate the requirements and the market prices to estimate the unit cost for each element.
Sensitivity analysis
To address the uncertainty about the real value of the parameters used in the economic model, different types of sensitivity analysis were developed. In particular, we developed a univariate sensitivity analysis to study the impact of a change in the value of one parameter at a time on the result of the cost-effectiveness analysis without modifying the rest of the parameters. Sensitivity analysis through diagrams of tornadoes was included, which allows joint analysis of changes in different parameters.
Results
Costs of the PC service
The direct cost, funded by the health system, was estimated at USD 6.46 per patient/day. By adding the diary cost of informal care, funded by the patients and their families, the total daily cost from the SP is calculated at USD 34.97 (Table 2).
Table 2
| Concept | PCS daily cost per patient (USD) |
|---|---|
| Human resources | 5.63 |
| Fuel | 0.01 |
| Disposable | 0.07 |
| Equipment | 0.04 |
| Medicines | 0.71 |
| Informal care cost | 28.51 |
| Total | 34.97 |
PCS, palliative care service.
The analysis of Table 2, particularly the composition of the direct costs of the PC Service, shows that the main driver of costs, from the FP, corresponds to human resources, which participates in 87% of the total direct costs. Also, it’s relevant to notice that daily direct cost funded by the public health system represents only 18% of the total costs funded by society.
Cost of UC
The main driver of the UC cost structure is medical consultations, which represent 96% of the cost borne by the funder. From de social perspective, the total daily cost of UC is $32.36, of which 88% corresponds to informal care (Table 3).
Table 3
| Concept | UC daily cost (USD) |
|---|---|
| Medical consultations | 3.70 |
| Equipment | 0.14 |
| Informal care cost | 28.51 |
| Total cost usual care | 32.36 |
UC, usual care.
Table 4 shows the summary of the daily costs used in de Markov Model, both from de FP and from the SP. In this model, the hospital admission costs were used to allocate costs during the time that patients are in the “Hospital Admission” state. Notice that the cost is almost 33 times the daily cost of PC from de FP.
Table 4
| Daily costs | Value (USD) | Range (USD) | Source |
|---|---|---|---|
| Palliative care (FP) | 6.46 | 5.17 to 7.75 | Calculated |
| Usual care (FP) | 3.85 | 3.08 to 4.62 | Calculated |
| Palliative care (SP) | 34.97 | 27.98 to 41.97 | Calculated |
| Usual care (SP) | 32.36 | 25.89 to 38.83 | Calculated |
| Emergency guard | 9.59 | 7.67 to 11.50 | Neuquén Tariff 2019 (57) |
| Hospital admission | 213.06 | 170.45 to 255.68 | Neuquén Tariff 2019 (57) |
FP, funder’s perspective; SP, social perspective.
Cost-effectiveness analysis from the SP
The main results of the cost-effectiveness analysis from the SP are shown in Table 5.
Table 5
| Strategy | Cost (USD) | Incremental cost | Effectiveness (% home death) | Incremental effectiveness | ICER |
|---|---|---|---|---|---|
| UC | 15.680 | 45.41 | |||
| PC service | 14.929 | −750 | 55.73 | 10.32 | −7.270 |
ICER, incremental cost-effectiveness ratio; UC, usual care; PC, palliative care.
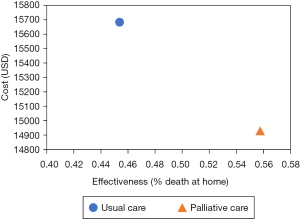
The UC strategy implied a social cost of USD 15,680 per cancer patient during the last year of life, allowing 45.41% of patients to die at home. By incorporating an organised PC service, the probability of patients dying at home increased by 10.32%. and the annual social cost per patient decreases to USD 14,929. So, the PC strategy is less costly and more effective than the UC strategy, as it is shown in Figure 2. This result is reinforced by the incremental cost-effectiveness ratio (ICER), which is the main indicator of the results of cost-effectiveness analysis and refers to the difference in cost per unit of effectiveness of the intervention compared to the reference one. In this case, the ICER is negative, indicating the intervention is dominant and should be adopted.
Model from the FP
The cost-effectiveness analysis was carried out from the perspective of the public health system of the province of Río Negro, as funder. In this sense, only the direct costs of the health system were considered, without including the social costs of informal care at home. The transition probabilities were the same in the model from the SP.
From the FP, the incorporation of PC services at the end of life also resulted in cost-saving. A higher percentage of deaths at home (10.32% increase) is achieved with lower costs, since the total cost of the last year of life per patient was USD 4,900 in the PC strategy compared to USD 5,912 in the UC.
Sensitivity analysis
Since the values of the parameters used in the model presents a degree of uncertainty, a sensitivity analysis was developed, allowing reasonable variations of the parameters in order to analyze their impact on the final results of the model.
To analyse the impact of the variation of the transition probabilities, the variation ranges proposed by Pham & Krahn were used (21) both for the transition from home care to emergency care and for the transition to hospitalisation after being admitted by emergency care. For transition probability values of returning home after admission to the hospital, the range of days of hospitalisation was taken from Gomes et al. (70). The cost variation range was calculated as 20% lower and higher of each daily cost in order to capture possible over or underestimation of those parameters. The range of maximum and minimum values of variation of the transition probabilities and costs used for the sensitive analysis are shown in Tables 1,4, respectively.
The sensitivity analysis showed that the results of the Markov model were robust to changes in the values of the parameters, since it only ceased to be cost-saving when there were important changes in the probability of transition from home care to emergency care, in the probability of continuing hospitalized and in the daily costs of care.
The tornado graph (Figure 3) showed the impact of changing the values of the parameters on the result of the incremental cost-effectiveness ratio (ICER). The larger bars show the parameters whose variation has the greatest impact on the result of the ICER. In this way, the ICER could stop being negative due to an increase in the Daily Cost of the PC branch or in the probability of continuing hospitalized, given that the patient is already hospitalized, in the PC branch or due to the decrease in the probability of continuing hospitalized given that the patient is already hospitalized, in the UC branch, or to a decrease of the Daily Cost of the UC branch.

Discussion
Key findings
This study, which is the first cost-effectiveness analysis of PC in Argentina, found that incorporating a home PC Service is cost-saving both for the health system and for society and allows a greater percentage of end-of-life cancer patients to die at home while the average number of days of hospitalisation they require decrease.
This study let us estimate that informal care represents the largest proportion of total spending (82%).
Strengths and limitations
Identifying and quantifying the weight of unpaid work in the PC at the end of life is the first step to advance in the analysis and study of the distribution of the visible and invisible costs of health care. This information should contribute to the discussion on a social (re)distribution of care, where the state designs policies aimed to reorganize resources to improve society’s well-being.
In the context of the fragmentation, segmentation and heterogeneity of health services in Argentina and the region (71), the results are not necessarily directly transferable to other provinces and countries, making it necessary to know their cost structures and their way of delivering PC services.
One of the main limitations of this study was the difficult access to information. The lack of unified records of PC indicators in public health has made it impossible for us to rely on local information on the percentage of deaths at home.
Cost-effectiveness models carry as one of their main limitations that they are an abstraction and simplification of real life. The variability between patients and different health contexts makes it difficult for the results of a model to be generalized. Another limitation of our work is given by the impossibility of having basic information regarding the hours dedicated to informal care in homes. To survey the unpaid care hours and a descriptive analysis of caregivers of end-of-life cancer patients in our region are proposed as future work.
Comparison with similar researches
From the SP, the greatest costs driver corresponded to informal care provided mainly by families, representing 82% and 88% of the total daily cost in the PC and UC strategies, respectively. This result can be compared with the estimate in Mexico, where the monetary value of health care provided at home was equivalent to 85.5% of the value of hospital services (72). As well, this is consistent with other works in which the SP has been incorporated. For example, the work by Chai et al. found that 76.7% of the costs of PC in the last year of life corresponded to the costs of unpaid care, while in work by Guerriere et al., this percentage was 71%.
It is shown the urgent need to make health care visible to family members and the cost that falls on them, as different works have already warned (26,41,69,73). Likewise, it has been estimated the impact of informal care in Latin America is between 15% and 44% of total healthcare costs (74).
Published studies show that patients who access PC services in the last year of life are more likely to die at home than those who only receive regular care. In a Cochrane systematic review on the effectiveness and cost-effectiveness of home PC services (70) they developed a meta-analysis that included only the 5 high-quality studies, which determine an odds ratio for the outcome “death at home” of 1.73 (95% CI: 1.28–2.33) for patients in home-based PC programs compared to those receiving UC. In the study of Pham & Krahn (21), 55.73% of patients with home PC services died at home, compared to 45.41% of those who received UC. This is the measure of effectiveness that we considered in this study.
Explanations of findings
In the PC strategy the percentage of the informal cost of caregivers is lower than in the UC strategy, so we can infer that the incorporation of the PC strategy could slightly reduce the enormous cost that families must face in this stage of care, without considering the decrease in the emotional cost due to the intrinsic characteristics of the PC strategy.
When comparing the results of the ICER from the SP with the results from the FP, we can observe that in the latter the ICER shows greater savings. This may be indicative of the existence of cost transfers from the health care system to the families, quantified through the monetary value of hours of unpaid care at home.
Implications and actions needed
The importance of producing evidence that quantifies the enormous challenge faced by health policy makers in Latin America is highlighted and contributes to making visible the burden that informal care represents for caregivers and society. Also, the participation of the state, health care providers, market, families, and society is necessary and fundamental, not only to recognize the importance of paid and unpaid domestic care and work carried out mainly by women, but also to carry out actions that reduce this burden and redistribute it equitably. In other words, actions that promote social co-responsibility in care are needed (75).
The importance of care at the end of life is widely demonstrated in the published literature, by improving the well-being of both the patient and their family. Quantifying the incremental costs (savings) and incremental health results of the strategy of implementing an organised PC service could encourage different jurisdictions to expand their network of providers of these services, which have very heterogeneous coverage throughout our country (14).
The economic implications of care in a PC context remain relatively neglected at the policy and research level. Experts have stressed the need to link different perspectives of analysis (of the health care system, of society, of families) to the relevant decision levels (State, ministries, individual services, patients) (76). We hope this paper will make a first contribution in this regard.
Finally, since this is the first EE of PC in our region, it is expected that it can pave the way for more in-depth studies that allow identifying opportunities for improvement that contribute to the development of public policies aimed at improving the access of population that require this type of care.
Conclusions
When developing the cost-effectiveness analysis for the public health system of the province of Río Negro, both from the social and FP, the strategy of implementing an organized PC service turned out to be cost-saving in comparison with UC. This would imply that the intervention strategy is more effective, measured as a percentage of deaths at home, at a lower cost.
The incorporation of PC can improve the allocation of resources between the different levels of care. Given that informal care represents the largest proportion of total PC spending, the visualisation of care tasks becomes especially relevant when considering public policies and results. Incorporating home PC strategies could alleviate the enormous costs faced by relatives of patients, especially women, in this stage of care.
Acknowledgments
We acknowledge the Palliative Care Service of the Cipolletti Hospital for providing us with the information for this study.
Funding: This work was supported by The National Institute of Cancer, National Ministry of Health of Argentina (Financial Assistance to Cancer Research Projects of National Origin IV, ReNIS Registration Number: IS002450).
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Claudia Fischer, Gudrun Waaler Bjørnelv, Rui Dang, Peter May, and Preeti Pushpalata Zanwar) for the series “Value of Palliative Care” published in Annals of Palliative Medicine. The article has undergone external peer review.
Reporting Checklist: The authors have completed the CHEERS reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-23-240/rc
Data Sharing Statement: Available at https://apm.amegroups.com/article/view/10.21037/apm-23-240/dss
Peer Review File: Available at https://apm.amegroups.com/article/view/10.21037/apm-23-240/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-23-240/coif). The series “Value of Palliative Care” was commissioned by the editorial office without any funding or sponsorship. S.H. and L.S.L. declare the Grant for the execution of the study from National Cancer Institute of Argentina. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Commission on Ethics and Evaluation of Research Projects in Human Health of the Province of Río Negro (Resolution MS No. 4974/18) and was incorporated into the National Registry of Health Research (No. IS002450). Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Davies E, Higginson IJ, editors. The solid facts: palliative care. Copenhagen: WHO Regional Office for Europe; 2004.
- Lowery WJ, Lowery AW, Barnett JC, et al. Cost-effectiveness of early palliative care intervention in recurrent platinum-resistant ovarian cancer. Gynecol Oncol 2013;130:426-30. [Crossref] [PubMed]
- Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 2010;363:733-42. [Crossref] [PubMed]
- Zimmermann C, Swami N, Krzyzanowska M, et al. Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. Lancet 2014;383:1721-30. [Crossref] [PubMed]
- Scibetta C, Kerr K, Mcguire J, et al. The Costs of Waiting: Implications of the Timing of Palliative Care Consultation among a Cohort of Decedents at a Comprehensive Cancer Center. J Palliat Med 2016;19:69-75. [Crossref] [PubMed]
- Colligan EM, Ewald E, Ruiz S, et al. Innovative Oncology Care Models Improve End-Of-Life Quality, Reduce Utilization And Spending. Health Aff (Millwood) 2017;36:433-40. [Crossref] [PubMed]
- Bakitas M, Lyons KD, Hegel MT, et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA 2009;302:741-9. [Crossref] [PubMed]
- UN. Committee on Economic S and CR (22nd sess. : 2000 : G. General comment no. 14, The right to the highest attainable standard of health (article 12 of the International Covenant on Economic, Social and Cultural Rights). Geneva; 2000.
- Connor S, Sepulveda C. Global atlas of palliative care at the end of life. London: Worldwide Palliative Care Alliance. 2014.
- Mertnoff R, Vindrola-Padros C, Jacobs M, et al. The Development of Palliative Care in Argentina: A Mapping Study Using Latin American Association for Palliative Care Indicators. J Palliat Med 2017;20:829-37. [Crossref] [PubMed]
- Pastrana T, De Lima L, Wenk R, et al. Atlas de Cuidados Paliativos de Latinoamérica ALCP. 1a edición. Houston: IAHPC Press; 2012.
- World Health Organization. Available online: https://www.who.int/es/news-room/fact-sheets/detail/palliative-care. 2020. Palliative Care. Key Facts.
- Knaul FM. Integrating palliative care into health systems is essential to achieve Universal Health Coverage. Lancet Oncol 2018;19:e566-7. [Crossref] [PubMed]
- Pastrana T, De Lima L, Sánchez-Cárdenas MA, et al. Atlas de Cuidados Paliativos en Latinoamérica 2020 (2 ed.). Houston: IAHPC Press; 2021.
- Pérez-Cruz PE, Undurraga E, Arreola-Ornelas H, et al. Bridging gaps to universal palliative care access in Chile: serious health-related suffering and the cost of expanding the package of care services. Lancet Reg Health Am 2023;19:100425. [Crossref] [PubMed]
- Knaul FM, Farmer PE, Krakauer EL, et al. Alleviating the access abyss in palliative care and pain relief-an imperative of universal health coverage: the Lancet Commission report. Lancet 2018;391:1391-1454. Correction appears in Lancet 2018;391:2212.
- Drummond MF, Sculpher MJ, Claxton K, et al. Methods for the economic evaluation of health care programmes. Oxford university press; 2015.
- Pace A, di Lorenzo C, Capon A, et al. Quality of Care and Rehospitalization Rate in the Last Stage of Disease in Brain Tumor Patients Assisted at Home: A Cost Effectiveness Study. J Palliat Med 2012;15:225-7. [Crossref] [PubMed]
- Hatziandreu E, Archontakis F, Daly A. The potential cost savings of greater use of home- and hospice- based end of life care in England. The potential cost savings of greater use of home- and hospice- based end of life care in England. Santa Monica; 2008.
- Ljungman D, Hyltander A, Lundholm K. Cost–Utility Estimations of Palliative Care in Patients With Pancreatic Adenocarcinoma: A Retrospective Analysis. World J Surg 2013;37:1883-91. [Crossref] [PubMed]
- Pham B, Krahn M. End-of-Life Care Interventions: An Economic Analysis. Ont Health Technol Assess Ser 2014;14:1-70. [PubMed]
- McBride T, Morton A, Nichols A, et al. Comparing the costs of alternative models of end-of-life care. J Palliat Care 2011;27:126-33. [Crossref] [PubMed]
- McCaffrey N, Agar M, Harlum J, et al. Is home-based palliative care cost-effective? An economic evaluation of the Palliative Care Extended Packages at Home (PEACH) pilot. BMJ Support Palliat Care 2013;3:431-5. [Crossref] [PubMed]
- Molinier P, Lagarreta M. Subjetiviad del cuidado: etica, trabajo y proyecto político [Internet]. Vol. 2016/1, Papeles del CEIC. 2016. Available online: https://www.redalyc.org/pdf/765/76544802001.pdf
- Calvente MG, del Río Lozano M, Marcos JM. Desigualdades de género en el deterioro de la salud como consecuencia del cuidado informal en España. Gac Sanit 2011;25:100-7. [Crossref]
- CEPAL NU. Cuidados y mujeres en tiempos de COVID-19: la experiencia en la Argentina [Internet]. CEPAL; 2020 [cited 2021 Feb 18]. Available online: https://hdl.handle.net/11362/46453
- Organización Panamericana de la Salud. La economía invisible y las desigualdades de género: La importancia de medir y valorar el trabajo no remunerado. Washington; 2008. 1-312 p.
- INDEC. Encuesta Nacional de Uso del Tiempo 2021. Ciudad Autónoma de Buenos Aires; 2022.
- Observatorio de Igualdad de Género de América Latina. Notas para la igualdad N° 30: La economía del cuidado como acelerador del cambio estructural con igualdad. 2020.
- Balardini L, Gherardi N, Martelotte N, et al. El trabajo no remunerado de cuidado de la salud: una mirada desde la igualdad de género. Organización Panamericana de la Salud. 2020.
- Fassbender K, Fainsinger R, Brenneis C, et al. Utilization and costs of the introduction of system-wide palliative care in Alberta, 19932000. Palliat Med 2005;19:513-20. [Crossref] [PubMed]
- Brumley R, Enguidanos S, Jamison P, et al. Increased satisfaction with care and lower costs: results of a randomized trial of in-home palliative care. J Am Geriatr Soc 2007;55:993-1000. [Crossref] [PubMed]
- Isenberg SR, Tanuseputro P, Spruin S, et al. Cost-effectiveness of Investment in End-of-Life Home Care to Enable Death in Community Settings. Med Care 2020;58:665-73. [Crossref] [PubMed]
- Chai H, Guerriere DN, Zagorski B, et al. The size, share, and predictors of publicly financed healthcare costs in the home setting over the palliative care trajectory: a prospective study. J Palliat Care 2013;29:154-62. [Crossref] [PubMed]
- Chai H, Guerriere DN, Zagorski B, et al. The magnitude, share and determinants of unpaid care costs for home-based palliative care service provision in Toronto, Canada. Health Soc Care Community 2014;22:30-9. [Crossref] [PubMed]
- Gardiner C, Ingleton C, Ryan T, et al. What cost components are relevant for economic evaluations of palliative care, and what approaches are used to measure these costs? A systematic review. Palliat Med 2017;31:323-37. [Crossref] [PubMed]
- Guerriere DN, Coyte PC. The Ambulatory and Home Care Record: A Methodological Framework for Economic Analyses in End-of-Life Care. Winter L, editor. J Aging Res 2011;2011:374237.
- Urwin S, van den Berg B, Lau YS, et al. The monetary valuation of informal care to cancer decedents at end-of-life: Evidence from a national census survey. Palliat Med 2021;35:750-8. [Crossref] [PubMed]
- Tripodoro V, Veloso V, Llanos V. Sobrecarga del cuidador principal de pacientes en cuidados paliativos. Argumentos 2015;307-30.
- Espinoza Miranda K, Jofre Aravena V. Sobrecarga, apoyo social y autocuidado en cuidadores informales. Ciencia y enfermería 2012;18:23-30. [Crossref]
- Gardiner C, Brereton L, Frey R, et al. Exploring the financial impact of caring for family members receiving palliative and end-of-life care: a systematic review of the literature. Palliat Med 2014;28:375-90. [Crossref] [PubMed]
- Hoefman RJ, van Exel J, Brouwer W. How to include informal care in economic evaluations. Pharmacoeconomics 2013;31:1105-19. [Crossref] [PubMed]
- Sanders GD, Neumann PJ, Basu A, et al. Recommendations for Conduct, Methodological Practices, and Reporting of Cost-effectiveness Analyses: Second Panel on Cost-Effectiveness in Health and Medicine. JAMA 2016;316:1093-103. [Crossref] [PubMed]
- Jacob G, Sanchez L. Manual de cuidados paliativos para la atención primaria de la salud. Ciudad Autónoma de Buenos Aires: Instituto Nacional del Cáncer. 2014.
- Tripodoro VA, Llano V, De Lellis S, et al. Modelo demostrativo de identificación precoz y atención continua de pacientes con cáncer y necesidades paliativas. Rev Argent Salud Publica 202012;e9.
- Tripodoro VA, Rynkiewicz MC, Llanos V, et al. Atención paliativa en personas con enfermedades crónicas avanzadas. Medicina (B Aires) 2016;76:139-47. [PubMed]
- Tripodoro V, Luxardo N, Veloso V, et al. Implementación del Liverpool Care Pathway en español en Argentina y en España: exploración de las percepciones de los profesionales ante el final de la vida. Medicina Paliativa [Internet]. 2013 [cited 2021 Mar 13]; Available online:
10.1016/j.medipa.2013.07.001 10.1016/j.medipa.2013.07.001 - Dussel V. Práctica y recursos utilizados para la provisión de control de síntomas y soporte familiar en niños con cáncer atendidos en hospitales públicos de la República Argentina. Estudio Cualitativo.Informe académico final presentado ante la Comisión Nacional Salud Investiga. Buenos Aires: Ministerio de Salud de la Nación.
- de Simone G, Manzini J, Tinant E, et al. End of Life Decisions (EOLD): Defining the most important from a Group of Experts in Argentina. In: EAPC Research Network Junior Forum, editor. 12th Congress of the European Association for Palliative Care [Internet]. Lisbon; 2011 [cited 2021 Jan 30]. Available online: https://www.eapcnet.eu/wp-content/uploads/2021/03/Lisbon-Abstracts-.pdf
- Fornells HA. Cuidados Paliativos En El Domicilio. Acta Bioeth 2000;6: [Internet]. [Crossref]
- Husereau D, Drummond M, Augustovski F, et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) statement: updated reporting guidance for health economic evaluations. BJOG 2022;129:336-44. [Crossref] [PubMed]
- INDEC. Proyecciones elaboradas en base al Censo Nacional de Población, Hogares y Viviendas 2010. 2016.
- Ministerio de Salud de Río Negro. Estadísticas Vitales. 2018.
- INDEC. 4° Encuesta Nacional de Factores de Riesgo 2018. Resultados definitivos. Ciudad Autónoma de Buenos Aires; 2019.
- Hales S, Chiu A, Husain A, et al. The quality of dying and death in cancer and its relationship to palliative care and place of death. J Pain Symptom Manage 2014;48:839-51. [Crossref] [PubMed]
- Zimmer JG, Groth-Juncker A, McCusker J. A randomized controlled study of a home health care team. Am J Public Health 1985;75:134-41. [Crossref] [PubMed]
- Ministerio de Salud de Neuquén. Nomenclador Globalizado de la Provincial del Neuquén. Actualización 2019;2019.
- Coyle D, Small N, Ashworth A, et al. Costs of palliative care in the community, in hospitals and in hospices in the UK. Crit Rev Oncol Hematol 1999;32:71-85. [Crossref] [PubMed]
- Mosoiu D, Dumitrescu M, Connor SR. Developing a costing framework for palliative care services. J Pain Symptom Manage 2014;48:719-29. [Crossref] [PubMed]
- Round J, Jones L, Morris S. Estimating the cost of caring for people with cancer at the end of life: A modelling study. Palliat Med 2015;29:899-907. [Crossref] [PubMed]
- van den Berg B, Brouwer WB, Koopmanschap MA. Economic valuation of informal care. An overview of methods and applications. Eur J Health Econ 2004;5:36-45. [Crossref] [PubMed]
- Oliva-Moreno J, Peña-Longobardo LM, Vilaplana-Prieto C. An Estimation of the Value of Informal Care Provided to Dependent People in Spain. Appl Health Econ Health Policy 2015;13:223-31. [Crossref] [PubMed]
- Posnett J, Jan S. Indirect cost in economic evaluation: the opportunity cost of unpaid inputs. Health Econ 1996;5:13-23. [Crossref] [PubMed]
- Torgerson DJ, Donaldson C, Reid DM. Private versus social opportunity cost of time: valuing time in the demand for health care. Health Econ 1994;3:149-55. [Crossref] [PubMed]
- Guerriere DN, Zagorski B, Fassbender K, et al. Cost variations in ambulatory and home-based palliative care. Palliat Med 2010;24:523-32. [Crossref] [PubMed]
- Brick A, Normand C, O’Hara S, Smith S. Economic evaluation of palliative care in Ireland. Atlantic Philanthropies; 2015.
- Wolff JL, Dy SM, Frick KD, et al. End-of-Life Care Findings From a National Survey of Informal Caregivers. Arch Intern Med 2007;167:40-6. [Crossref] [PubMed]
- Observatorio de Empleo y Dinámica Empresarial (OEDE). Evolución de las remuneraciones de los trabajadores registrados [Internet]. Ciudad Autónoma de Buenos Aires; 2021. Available online: http://www.trabajo.gob.ar/estadisticas/oede/
- Dirección Nacional de Economía Igualdad y Género. Los cuidados, un sector económico estratégico Medición del aporte del Trabajo Doméstico y de Cuidados no Remunerado al Producto Interno Bruto. 2020.
- Gomes B, Calanzani N, Curiale V, et al. Effectiveness and cost-effectiveness of home palliative care services for adults with advanced illness and their caregivers. Cochrane Database Syst Rev 2013;2013:CD007760. [PubMed]
- Lamfre L, Hutter F, Álvarez J, et al. Evaluaciones económicas en un sistema de salud fragmentado: oportunidades y desafíos metodológicos para Argentina. Rev Argent Salud Pública 2018;9:37-42.
- CEPAL. Panorama Social de América Latina, 2016. 2017. Available online: https://www.cepal.org/es/publicaciones/41598-panorama-social-america-latina-2016
- Durán MÁ. Las cuentas del cuidado. Revista Española de control externo. 2018;20:57-89.
- Espinola N, Pichon-Riviere A, Casarini A, et al. Making visible the cost of informal caregivers' time in Latin America: a case study for major cardiovascular, cancer and respiratory diseases in eight countries. BMC Public Health 2023;23:28. [Crossref] [PubMed]
- Pautassi L. El cuidado: de cuestión problematizada a derecho. Un recorrido estratégico, una agenda en construcción. In: El trabajo de cuidados: una cuestión de derechos humanos y políticas públicas. ONU Mujeres; 2018. p. 178-91.
- Gomes B, Harding R, Foley KM, et al. Optimal approaches to the health economics of palliative care: report of an international think tank. J Pain Symptom Manage 2009;38:4-10. [Crossref] [PubMed]



