Use of multimedia in patient and caregiver education for cancer pain management: a literature review
Introduction
With over 1.6 million new cancer diagnoses and 595,000 cancer-related deaths in the United States in 2016 alone, cancer-related morbidity and mortality remains highly pervasive (1,2). The burden of cancer has increasingly shifted to less developed countries, which currently account for 57% of cases and 65% of cancer-related deaths worldwide (2). Despite the increasing incidence of diagnoses, cancer patients are living for longer durations with their diagnoses (1).
While the exact etiology of cancer pain remains unknown and is likely multifactorial, 38% of all cancer patients report experiencing moderate to severe pain during the course of their illness (3,4). A published meta-analysis suggested that pain prevalence rates among cancer patients was substantial but variable: 39.3% reported pain following curative treatment, 55% during anti-cancer treatment, and 66.4% in advanced, metastatic, or terminal stages of the disease (4).
Pain management programs in cancer treatment centers often provide educational interventions for patients and caregivers using a multidisciplinary approach. Health literacy is critical to successful pain management interventions, specifically those addressing medical aspects such as medication adherence, and those that account for patient knowledge, attitudes, values and preferences (5-8). Meta-analyses have shown that patient and caregiver education (PCE) as an intervention for pain management is moderately favoured compared to management not involving education components, and is associated with lower perceived pain intensity (6-8). These encouraging results may be attributed to either the successful promotion of the use of prescribed analgesics by the team (5), and/or improved self-efficacy on the part of a better educated patient and caregiver (8,9). While the effectiveness of PCE interventions has been evidenced, it is recognized that such interventions may also be burdensome in terms of costs, time investment and resource allocation, especially for certain intervention modalities.
Multimedia-based interventions may provide a relatively low-cost, time-efficient, user-friendly and easily-accessible medium for PCE. To the best of our knowledge, recent efforts to synthesize the evidence surrounding the clinical effectiveness and costs associated with multimedia-based PCE interventions are limited. As such, the purpose of our literature review is to examine the literature surrounding clinical effectiveness involved with multimedia-based PCE interventions addressing pain management outcomes in cancer patients.
Materials and methods
Search strategy
A literature search was conducted in Ovid MEDLINE (1946–July Week 2, 2016), Ovid Embase (1947–2016 Week 29), and Ovid Cochrane Central Register of Controlled Trials (up to June 2016). The three databases were selected based on the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions. Both controlled vocabularies (MeSH & Emtree subject headings) and free text keywords were used in the search. Search terms included: ‘Neoplasms/’, ‘Pain/’, ‘Pain Management/’, ‘Pain Clinic/’, ‘Cancer Pain/’, ‘Patient Education as Topic/’, ‘Health Education/’, ‘Education/’, ‘Caregivers/’, ‘family’, ‘spouse’, ‘train*’, ‘coping’, ‘coach*’, ‘teach*’, ‘educat*’, ‘empower*’. The search was limited to human subjects and English-language studies, with no publication date limit. The complete search strategy is available in Appendix.
Eligibility criteria
Studies were considered eligible if they: (I) involved an experimental, quasi-experimental or cohort (retrospective or prospective) study design; (II) involved a cancer patient population and/or their caregivers; (III) involved the use or provision of one or more multimedia-based PCE interventions focused on pain and symptom management; and (IV) reported on cancer pain and pain management-related outcomes using a standard pain measure. We defined multimedia as any audio/visual recordings or interactive programs available in various multimedia formats such as CDs, DVDs or computer-playable files delivered via portable media or internet resources.
Study selection
Two reviewers (M Lam, M Choi) screened titles and abstracts independently based on the a priori eligibility criteria. Consensus was established with discussion to resolve conflicts. Full-text articles for potentially eligible titles and abstracts were then retrieved and screened for eligibility independently by the two reviewers (M Lam, M Choi) using the same a priori criteria, with consensus established via discussion.
Data extraction
The following data were extracted from all eligible articles: year of publication, number and characteristics of patients included, multimedia-based PCE intervention group (sample size, details regarding intervention), control group intervention (sample size, details regarding intervention), standard pain measure used, and a qualitative summary of study findings. Study quality and risk of bias were not formally evaluated.
Data extraction was conducted by two reviewers (M Lam, M Choi) independently, with consensus established via discussion.
Analysis
Findings were summarized for each study independently. Due to the substantial differences in study design and the variability in quantitative assessment tools among the five RCTs, results were synthesized qualitatively without a meta-analysis.
Results
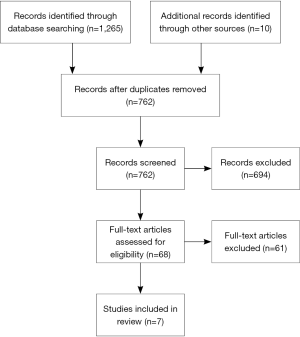
Of 1,265 hits yielded by the literature search, 752 unique hits were identified and screened at the title and abstract level. Sixty-eight titles and abstracts were deemed potentially eligible, and were retrieved as full-text articles for subsequent full-text screening. Seven references were finally deemed eligible and included in the qualitative synthesis (10-16) (Figure 1).
Characteristics of included studies
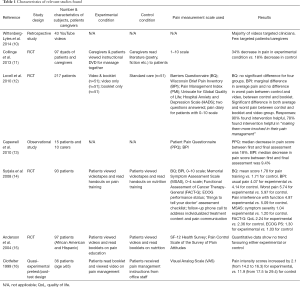
Of the seven eligible studies, five were randomized controlled trials (11,12,14-16), two were observational studies (10,13). Wittenberg et al. did not evaluate the effectiveness or cost associated with a multimedia-based PCE intervention; instead, the authors analyzed the availability of YouTube videos designed for patients/caregivers on educational interventions (10). All other studies evaluated the effectiveness of multimedia-based PCE among cancer patients and/or their caregivers directly (11-16) (Table 1).
Full table
Summary of study findings
All included RCTs except one by Anderson et al. study (15) found that multimedia-based PCE interventions were more effective for cancer pain management than control interventions. The Brief Pain Inventory (BPI) and Barriers Questionnaire (BQ) were two commonly-used assessment tools.
Syrjala et al. tested a pain training module against a nutritional control, both involving patient-targeted videos and print materials (14). The study reported lower patient-reported symptom severity [Memorial Symptom Assessment Scale (MSAS); 1.04 vs. 1.20], as well as lower ‘usual pain’ and ‘worst pain’ scores (14). Lovell et al. also reported statistically significant findings when comparing a multimedia-based educational intervention to a standard care control (12). The study found 90% of participants responded that they “felt the intervention was helpful”, and 78% stated that they “felt the intervention helped to make them more involved in their pain management” (12). However, overall quality of life (QoL) was highest in the control group (12).
Collinge et al. evaluated the effectiveness of multilingual educational DVDs detailing various aspects of massage therapy with a sample of 97 participants, where the experimental arm received instructional videos on communication, frame of mind, and management of pain, nausea, and anxiety, and those in the control arm received educational literature (11). A 34% decrease in pain was found in the experimental arm relative to only 18% in the control arm, and relatively larger decreases in stress/anxiety, fatigue, depression and nausea symptoms were also reported (11).
Clotfelter et al. evaluated a multi-component PCE intervention in elderly cancer patients with pain management (16). The intervention involved a booklet titled “Managing Cancer Pain”, a video presentation highlighting various pain management strategies including drug and non-drug interventions, support groups, and communication with a health care provider, while classic pain management education was provided to the control group (16). Results demonstrated a greater reduction in Visual Analog Scale (VAS) pain intensity scores in the experimental group (17.5 to 29.4 vs. 14.2 to 16.3) for the experimental group (16). Based on these results the author arrived at two major conclusions; that there was limited literature on pain management for elderly cancer patients, and that the use of multimedia, namely videotaped teaching sessions, could be of value in improving “patients’ self-management of pain” (16).
Two observational studies evaluating multimedia-based PCE interventions for pain management were identified. A study by Capewell et al. found a median reduction in pain scores of 18% based on the Patient Pain Questionnaire (PPQ) and 9.4% based on the BPI with a DVD-based educational intervention for palliative care patients and their caregivers (13), demonstrating sizeable benefits with such a PCE intervention within a short period of time. A second observational study by Wittenberg-Lyles et al. investigated the availability and features of YouTube videos on pain management in cancer. Of 43 videos analyzed, 33 were targeted at clinicians. While a number of videos were categorized as “Education” on the website, assumedly due to their lecture-style format, only three were actually designed for patients and caregivers, and discussed strategies and challenges in pain management (10). Study findings suggested that additional research examining whether YouTube could be used as an effective PCE resource for pain management was needed (10).
Discussion
The findings of our literature review demonstrate that there is limited but optimistic experimental and observational evidence demonstrating that multimedia-based interventions may be effective as pain management educational tools for patients with cancer pain and their caregivers compared to standard education (10-16).
Multimedia-based PCE interventions may provide a user-friendly, inexpensive and easily-accessible source of information for patients suffering from cancer pain and their caregivers. These programs are often targeted towards the needs of particular patient or caregiver groups, and therefore, may provide tailored educational material fitting the needs of specific cancer patient and caregiver populations better than broadly-focused educational material (16). Multimedia-based programs may also be more engaging and interactive than traditional interventions, and may allow personalization of the information received, which may be critical to a patient- and caregiver-centered approach to education and symptom management. The flexibility of these interventions to also readily incorporate videos, animations, and spaces for user input alongside providing text-based information and images provide an added advantage over traditional hardcopy educational materials, which primarily rely on text content and images (16).
While these advantages may exist, multimedia-based interventions might not be well-received by all patients and caregivers, may require additional technology and require a baseline level of user capability to operate, which may not be barriers faced by traditional tools. Interventions such as computer and smartphone programs may also be challenging to navigate and may be more unstable or likely to be incompatible with certain operating systems. Health care organizations may also find the development of multimedia-based educational tools more challenging, and tools may be more likely to be poorly-developed relative to traditional educational materials due to limited technological resources and the complexity of the development process involved; the usability of the educational information may suffer in such cases.
An important finding of our literature review was that multimedia-based resources on the internet such as YouTube were largely focused on clinicians and rarely targeted patients and caregivers (10). Additional efforts to expand the scope of patient/caregiver-centered educational materials on these forums might be beneficial, given how widespread their use is among these groups.
It is important to recognize certain limitations when interpreting the findings of our literature review. The literature review is limited by the small number of studies available addressing the research question. Given that only peer-reviewed literature was searched, multimedia-based PCE interventions for cancer pain that did not have an associated peer-reviewed publication evaluating their effectiveness would be missed by this literature review; as such, the literature review is a reflection of the state of the evidence supporting a limited proportion of these interventions, rather than a holistic overview of all existing interventions. It is also important to consider that the usability and user-friendliness of these multimedia-based PCE interventions was not formally addressed in this literature review; these are critical aspects to the uptake and success of such interventions. In addition, the lack of a meta-analysis due to differences in study designs and variability in the quantitative assessment tools used across the included RCTs limited our findings to a qualitative synthesis of identified studies. Finally, given limitations in sample sizes, lengths of follow-up and other aspects of study design for most of the included studies, it is important to consider that our findings are based on lower-quality evidence. Risk of bias was not formally evaluated.
Conclusions
Our review summarized the literature surrounding the effectiveness of multimedia-based PCE interventions for cancer-related pain management. Limited evidence suggested positive effects of multimedia-based interventions among cancer patients and caregivers for pain management relative to conventional educational materials such as verbal instruction and medical management of cancer pain. Additional research regarding the usability and user-friendliness of these multimedia-based PCE interventions and their effectiveness among cancer patients and their caregivers is needed to better understand how useful these tools might be for patients and caregivers, and may help guide their role moving forward as an integral part of education throughout the cancer journey.
Acknowledgements
The authors thank the generous support of the Bratty Family Fund, Michael and Karyn Goldstein Cancer Research Fund, Joey and Mary Furfari Cancer Research Fund, Pulenzas Cancer Research Fund, Joseph and Silvana Melara Cancer Research Fund, and Ofelia Cancer Research Fund.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Appendix
Database search strategies
Ovid MEDLINE(R) <1946 to July Week 2 2016>:
1. exp Neoplasms/ [2870793]
2. exp Pain/ [335410]
3. exp Pain Management/ [24165]
4. Patient Education as Topic/ [75797]
5. Health Education/ [55876]
6. Caregivers/ [25761]
7. education/ or education, nonprofessional/ [19528]
8. [(patient* or family or families or spouse or spousal or caregiver*) adj3 (train* or coping or coach* or teach* or educat* or empower*)].mp. [120765]
9. 1 and (2 or 3) and [4 or 5 or (6 and 7) or 8] [555]
10. limit 9 to (English language and humans) [501]
Embase Classic + Embase <1947 to 2016 Week 29>:
1. exp neoplasm/ [3935496]
2. exp cancer pain/ [16739]
3. exp *pain/ [355023]
4. exp pain clinic/ [2651]
5. exp analgesia/ [131006]
6. exp patient education/ [95524]
7. patient counseling/ [36215]
8. [(patient* or family or families or spouse or spousal or caregiver*) adj3 (train* or coping or coach* or teach* or educat* or empower*)].mp. [164442]
9. 1 and (2 or 3 or 4 or 5) and (6 or 7 or 8) [632]
10. limit 9 to (human and English language) [563]
EBM Reviews—Cochrane Central Register of Controlled Trials :
1. exp Neoplasms/ or (neoplasm or cancer or tumor or tumour).mp. [92848]
2. exp Pain/ or pain.mp. [88503]
3. exp Pain Management/ or analgesia.mp. [22309]
4. Patient Education as Topic/ [6630]
5. Health Education/ [2960]
6. Caregivers/ or caregiver*.mp. [4137]
7. education/ or education, nonprofessional/ [553]
8. [(patient* or family or families or spouse or spousal or caregiver*) adj3 (train* or coping or coach* or teach* or educat* or empower*)].mp. [16644]
9. 1 and (2 or 3) and [4 or 5 or (6 and 7) or 8] [218]
10. limit 9 to English language [201]
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin 2016;66:7-30. [Crossref] [PubMed]
- Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin 2015;65:87-108. [Crossref] [PubMed]
- Schmidt BL. The neurobiology of cancer pain. Neuroscientist 2014;20:546-62. [Crossref] [PubMed]
- van den Beuken-van Everdingen MH, Hochstenbach LM, Joosten EA, et al. Update on Prevalence of Pain in Patients With Cancer: Systematic Review and Meta-Analysis. J Pain Symptom Manage 2016;51:1070-1090.e9. [Crossref] [PubMed]
- Devine EC. Meta-analysis of the effect of psychoeducational interventions on pain in adults with cancer. Oncol Nurs Forum 2003;30:75-89. [Crossref] [PubMed]
- Marie N, Luckett T, Davidson PM, et al. Optimal patient education for cancer pain: a systematic review and theory-based meta-analysis. Support Care Cancer 2013;21:3529-37. [Crossref] [PubMed]
- Jho HJ, Myung SK, Chang YJ, et al. Efficacy of pain education in cancer patients: a meta-analysis of randomized controlled trials. Support Care Cancer 2013;21:1963-71. [Crossref] [PubMed]
- Bennett MI, Bagnall AM, José Closs S. How effective are patient-based educational interventions in the management of cancer pain? Systematic review and meta-analysis. Pain 2009;143:192-9. [Crossref] [PubMed]
- van der Peet EH, van den Beuken-van Everdingen MH, Patijn J, et al. Randomized clinical trial of an intensive nursing-based pain education program for cancer outpatients suffering from pain. Support Care Cancer 2009;17:1089-99. [Crossref] [PubMed]
- Wittenberg-Lyles E, Parker Oliver D, Demiris G, et al. YouTube as a tool for pain management with informal caregivers of cancer patients: a systematic review. J Pain Symptom Manage 2014;48:1200-10. [Crossref] [PubMed]
- Collinge W, Kahn J, Walton T, et al. Touch, Caring, and Cancer: randomized controlled trial of a multimedia caregiver education program. Support Care Cancer 2013;21:1405-14. [Crossref] [PubMed]
- Lovell MR, Forder PM, Stockler MR, et al. A randomized controlled trial of a standardized educational intervention for patients with cancer pain. J Pain Symptom Manage 2010;40:49-59. [Crossref] [PubMed]
- Capewell C, Gregory W, Closs S, et al. Brief DVD-based educational intervention for patients with cancer pain: feasibility study. Palliat Med 2010;24:616-22. [Crossref] [PubMed]
- Syrjala KL, Abrams JR, Polissar NL, et al. Patient training in cancer pain management using integrated print and video materials: a multisite randomized controlled trial. Pain 2008;135:175-86. [Crossref] [PubMed]
- Anderson KO, Mendoza TR, Payne R, et al. Pain education for underserved minority cancer patients: a randomized controlled trial. J Clin Oncol 2004;22:4918-25. [Crossref] [PubMed]
- Clotfelter CE. The effect of an educational intervention on decreasing pain intensity in elderly people with cancer. Oncol Nurs Forum 1999;26:27-33. [PubMed]