Excellent and durable response to radiotherapy in a rare case of spinal cord compression due to extra-medullary hematopoiesis in β-thalassemia intermedia: case report and clinicoradiological correlation
Introduction
Spinal cord compression (SCC) is a debilitating skeletal related event (SRE) mostly caused by malignancies, however an unusual cause for SCC is extra-medullary hematopoiesis (EMH). EMH usually occurs in myelofibrosis, polycythemia vera, thalassemia, sickle cell anemia, leukemia, lymphoma or after bone marrow irradiation (1,2).
β-thalassemia intermedia (β-TI), first described in 1955 by Sturgeon et al. is a disease of intermediate clinical severity between thalassemia major and trait (3). There are isolated case reports for the successful use of RT in EMH and long term outcomes, only few with clinicoradiological correlation and we report the same (4).
Case presentation
A 24-year-old male presented to our hospital with 2 episodes of generalized tonic-clonic seizures (GTCS) and weakness of both lower limbs for 3 months, numbness below trunk for 2 months and swaying while walking for 1 month. The diagnosis of thalassemia was made when he was 7 years old, when he presented with jaundice and examination revealed frontal bossing and hepatosplenomegaly. The patient had his first blood transfusion at age 7 for a hemoglobin of 8.2 g/dL and received one pint blood transfusion every 2 years. At age 17 years, he had his first GTCS and was diagnosed as having idiopathic epilepsy.
Examination revealed pallor, bossing of skull, flattened nasal bridge, low set ears, high arched palate and kyphoscoliosis. CNS examination revealed clasp-knife spasticity in right lower limb, increased tone in lower limbs of 3+/5 at hip and knee joints. Bilateral knee jerk was exaggerated and plantar reflex was extensor bilaterally. Sensation was decreased from T9 dermatome downwards for pin prick and touch. Vibration was decreased below T8 vertebral level. Romberg sign was positive, he could walk with support with a limping gait. Abdominal examination revealed hepatosplenomegaly—liver 7 cm and spleen 4 cm below respective costal margins. A diagnosis of cord compression at T8 level was made.
Complete blood profile showed a hemoglobin (Hb) of 8.4 g/dL, total WBC count was 10,300 cells/cc and Hb electrophoresis revealed HbA, HbA2 and HbF of 14.4%, 2.3% and 83.3% respectively. An MRI of the spine was obtained which revealed diffusely altered signal seen in whole spine appearing hypointense in T2w with vertically oriented lace like areas of T1w hypointense signals—findings consistent with thalassemia with marrow reconversion (Figure 1).
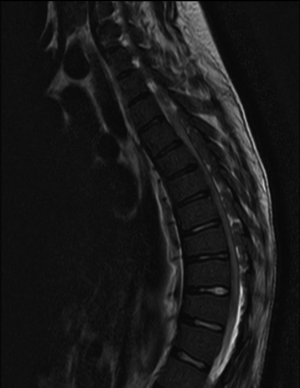
The differential diagnoses entertained were EMH, lymphoma, leukemia or epidural abscess however a diagnosis of thalassemia with extra medullary hematopoiesis was made based on MRI findings. EMH was noted from T5−T11 and L5−S2 causing maximal SCC at T6 as well as compression to cauda equina nerve roots. There was edema of the spinal cord between T5−T10 level (Figure 1).
With a diagnosis of thalassemia intermedia and seizure disorder with EMH causing SCC and paraparesis, the patient was planned for external beam radiotherapy (EBRT) along with steroids and two-pint blood transfusion. Informed consent for EBRT was obtained after explaining the beneficial effect of EBRT but with an attending minor increased risk of malignancy in future. EBRT was planned with 6-MV beams (Elekta Precise, Stockholm) and AP-PA portals to a dose of 20 Gy/10 fractions over 13 days after contouring T3−T12 and L4−S3 vertebral bodies and the haematopoietic mass, optimizing the dose using the treatment planning system (Oncentra v4.3, Elekta, Stockholm).
By the 5th fraction of EBRT itself, patient was significantly better and could walk without support, WBC count was 4,600 cells/cc. At conclusion of EBRT, examination revealed power 4+/5 in both hips and 5/5 in rest of the muscle groups. His WBC count was 4,290 cells/cc. An MRI at EBRT conclusion revealed hyperintense marrow changes in T3-L1 spine suggestive of post-radiation changes (Figure 2). The posterior epidural soft tissue (EMH) had reduced in size, increasing the AP diameter of the spinal canal from 3.6 to 6.9 mm at T6 (where the compression was maximum). However, the dorsal spinal edema was unchanged (Table 1,Figure 3).


Full table
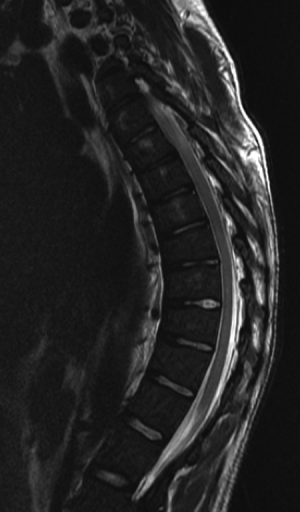
At 2 months post radiotherapy, patient had fully improved clinically and was able to ambulate with a normal gait. CNS examination was unremarkable. Hb was 9.1 g/dL for which one pint whole blood was transfused. MRI revealed persistence of spinal cord edema at T5−T9. However, the spinal canal diameter had increased further to 8.9 mm at T6 spinal level with further reduction in size of the epidural soft tissue (Figure 3). Patient was begun on hydroxyurea 500 mg once daily in addition to the previous medication. Patient is presently 18 months post-EBRT and has no residual weakness.
Discussion
Thalassemia is not an uncommon disease in India—with an overall prevalence of 3−4% however the predominant subtype is the minimally symptomatic thalassemia minor (5). While 10,000−12,000 children are born each year in India with thalassemia major, the incidence of thalassemia intermedia in India is not known (6). Pathological hemoglobinopathies in India occur around 1.2/1,000 live birth (7). Ineffective erythropoiesis in hemoglobinopathies leads to EMH mainly in the liver, spleen and lymph nodes and unusually in the adrenal glands, kidneys, breasts, dura mater, adipose tissue and skin (2). Since 1954, when the first case report of SCC in EMH due to Coley’s disease was reported, isolated case reports have published their experience with this rare disease but the optimal management still remains debatable (8).
The diagnosis of EMH is made in the background of a chronic hemoglobinopathy and an MR showing an epidural soft tissue component (1). MRI is the gold standard for diagnosing EMH as biopsy of the vascular mass could lead to catastrophic hemorrhage and should be reserved for patients with severe cord compression planned for laminectomy (2). Findings in MRI suggesting an active marrow lesion are high vascularity, minimal gadolinium enhancement and intermediate signal intensity on T1 and T2 weighted images while an older inactive marrow lesion shows high signal intensity due to fatty infiltration. The differential diagnoses for an epidural mass are metastatic malignant disease, lymphoma, multiple myeloma, vascular anomalies, EMH or epidural abscess (1,2).
In our patient, active extra-medullary hematopoietic masses were initially hypointense on T1w and T2w MR images which by conclusion of RT and at follow-up became hyperintense (Figures 2,3). This is explained by the rapid conversion of active marrow into yellow fatty marrow (9). Also, bone marrow is an exquisitely radiosensitive organ, experiments showing the D0 dose for a mouse bone marrow as 0.95 Gy (10). There was a corresponding 58% drop in total WBC count from 10,300 to 4,290 cells/cc and 61% decrease in AP diameter of the mass over the 2 weeks of radiotherapy (Table 1). Thus, even a short course of low dose RT produces rapid reversal of the SCC without significant myelosuppression.
Among the various treatment options available, rapid and durable reversal of SCC can be achieved with radiotherapy or laminectomy. Though there is no guideline for the optimal management, case reports of excellent and durable response to EBRT exist (2,4,11). Hypertransfusion can reduce the body’s requirement of EMH but has other side effects and was found inadequate in a case report of SCC, later relieved by EBRT (12). Hydroxyurea, which increases fetal hemoglobin production has been shown to relieve SCC in a case report but over several weeks again requiring EBRT at the time of relapse (13). Radiotherapy has shown residual masses on imaging which have a potential risk of recurrence in an older series where the dose of radiotherapy was suboptimal (14).
The two main drawbacks of radiotherapy in SCC are the risk of persistent spinal cord edema and myelosuppression. As demonstrated in our patient, the cord edema is clinically not relevant and can be controlled with a short course of steroids and the myelosuppression is not severe as the duration of radiotherapy is short.
Hence, we strongly advocate radiotherapy as the treatment of choice for SCC secondary to EMH as it results in rapid reversal, durable response with minimal acute hematological and GI side effects.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Informed consent for EBRT was obtained after explaining the beneficial effect of EBRT but with an attending minor increased risk of malignancy in future.
References
- Haidar R, Mhaidli H, Taher AT. Paraspinal extramedullary hematopoiesis in patients with thalassemia intermedia. Eur Spine J 2010;19:871-8. [Crossref] [PubMed]
- Talapatra K, Nemade B, Siddha M, et al. Extramedullary haematopoiesis causing spinal cord compression: A rare presentation with excellent outcome. Ann Indian Acad Neurol 2007;10:115-7. [Crossref]
- Sturgeon P, Itano HA, Bergren WR. Genetic and biochemical studies of intermediate types of Cooley's anaemia. Br J Haematol 1955;1:264-77. [Crossref] [PubMed]
- Munn RK, Kramer CA, Arnold SM. Spinal cord compression due to extramedullary hematopoiesis in beta-thalassemia intermedia. Int J Radiat Oncol Biol Phys 1998;42:607-9. [Crossref] [PubMed]
- Aggarwal R, Prakash A, Aggarwal M. Thalassemia: An overview. J Sci Soc 2014;41:3-6. [Crossref]
- Mohanty D, Colah RB, Gorakshakar AC, et al. Prevalence of β-thalassemia and other haemoglobinopathies in six cities in India: a multicentre study. J Community Genet 2013;4:33-42. [Crossref] [PubMed]
- Christianson A, Howson CP, Modell B. March Dimes global of report on birth defects: The Hidden Toll of Dying and Disabled Children. March of Dimes Birth Defects Foundation 2006. Available online: http://www.marchofdimes.org/materials/global-report-on-birth-defects-the-hidden-toll-of-dying-and-disabled-children-full-report.pdf
- Gatto I, Terrana V, Biondi L. Compression of the spinal cord due to proliferation of bone marrow in epidural space in a splenectomized person with Cooley's disease. Haematologica 1954;38:61-76. [PubMed]
- Yankelevitz DF, Henschke CI, Knapp PH, et al. Effect of radiation therapy on thoracic and lumbar bone marrow: evaluation with MR imaging. AJR Am J Roentgenol 1991;157:87-92. [Crossref] [PubMed]
- Till JE, McCulloch EA. A direct measurement of the radiation sensitivity of normal mouse bone marrow cells. Radiat Res 1961;14:213-22. [Crossref] [PubMed]
- Ruo Redda MG, Allis S, Reali A, et al. Complete recovery from paraparesis in spinal cord compression due to extramedullary haemopoiesis in beta-thalassaemia by emergency radiation therapy. Intern Med J 2014;44:409-12. [Crossref] [PubMed]
- Goerner M, Gerull S, Schaefer E, et al. Painful spinal cord compression as a complication of extramedullary hematopoiesis associated with beta-thalassemia intermedia. Strahlenther Onkol 2008;184:224-6. [Crossref] [PubMed]
- Gamberini MR, Fortini M, De Sanctis V. Paraplegia due to spinal cord compression by extramedullary erythropoietic tissue in a thalassaemia intermedia patient with gynecomastia secondary to cirrhosis: successful treatment with hydroxyurea. Pediatr Endocrinol Rev 2004;2 Suppl 2:316-8. [PubMed]
- Papavasiliou C, Sandilos P. Effect of radiotherapy on symptoms due to heterotopic marrow in beta-thalassaemia. Lancet 1987;1:13-4. [Crossref] [PubMed]


