Clinical presentations of below knee bone metastases: a case series
Introduction
Bone metastases are one of the most common sites of metastases, particularly in prostate and breast cancer patients (1). The prevalence of bony metastases seems to be rising due to a combination of factors including increased incidence of cancer due to longer survival and improved systemic treatment resulting in improved overall survival of cancer patients (2). Typical skeletal-related events caused by bone metastases include spinal cord compression, hypercalcemia, neurologic deficits, fractures and most commonly, pain. While bone metastases affect the axial skeleton in over 85% of cases, they may also occur in the appendicular skeleton, with the most frequent locations being the femur and humerus; however, below-the-knee metastases are extremely rare (3).
There are two types of bone metastases: osteoblastic and osteolytic. In osteolytic metastases, the bone resorption rate greatly exceeds that of the bone production rate which can cause severe reductions in bone strength (4). Osteoblastic lesions involve increased bone formation leading to inflexibility and rigidity, which compromises structural integrity of the bone (4). Below-the-knee metastases can have a significant impact on patient mobility and function compared to other sites in the axial and appendicular skeleton due to their weight-bearing potential. Bone metastases in the tibia and fibula can disrupt the integrity of the bone through cortical and tracebular destruction, ultimately causing pathological fractures and severely impacting QoL (4).
Herein, we present four cases in which two female and two male patients developed painful below-the-knee metastases.
Case presentation
Case 1: unknown primary cancer with metastases to right tibia
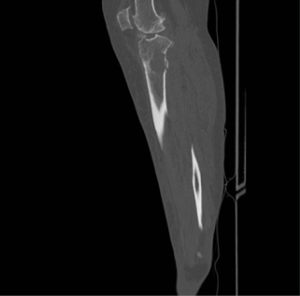
A 55-year-old woman was referred to palliative radiation clinic in 2016 for treatment of painful bone metastases in the right lower leg from an unknown primary. Computed tomography (CT) scans of the thorax and upper abdomen revealed pulmonary nodules and lytic lesions in the thoracic vertebra with a differential diagnosis of metastatic disease, sarcoid infection, or another inflammatory process. In the knee, CT scans revealed a lytic soft tissue lesion measuring 2.5 cm × 2.3 cm with focal destruction of the cortex in the proximal tibial metaphysis. The patient was referred to an orthopedic surgeon for consideration of surgical fixation of the tibial lesion and given acetaminophen, codeine, and hydromorphone to manage her pain. However, the patient presented to the Emergency Department the following day due to increased pain and investigations revealed a pathologic fracture of the tibia (Figure 1). The patient was admitted and underwent a CT-guided biopsy of the tibial lesion to determine the appropriate course of surgical action. CT scans during the admission revealed disease progression with metastatic lesions in the liver, adrenal glands, kidneys, lungs, and bone. The biopsy revealed renal cell carcinoma and 2 weeks after admission, the patient underwent open reduction internal fixation of the tibial plateau fracture and complete total knee replacement for the right knee (Figure 2). The patient was planned for 30 Gy in ten fractions of post-operative radiation to the tibia 1 month following surgery to prolong the lifetime of the prosthesis; however, complications arose including necrosis at the surgical site and infection during radiation; thus, treatment was cancelled until further re-assessment. In the interim, the patient passed away on the ward.

Case 2: primary breast cancer with bilateral metastases to fibulae
In 2016, a 58-year-old woman with metastatic breast cancer was referred to a palliative radiotherapy clinic due to painful lesions in both lower legs. Prior to her appointment, X-rays were completed that indicated a pathological oblique fracture of the right proximal fibula (Figure 3) and metastatic lesions within her left tibia and fibula as well (Figure 4). The patient was originally referred to orthopedic surgery but was deemed not suitable for surgical treatment. The patient underwent radiotherapy consisting of 30 Gy in ten fractions for the lesions in her bilateral lower limbs to promote bone healing and to palliate pain. During radiotherapy, the patient developed pain flare that subsequently resolved. When the patient was reassessed 1-month post-radiation, she reported good pain relief and improved mobility.


Case 3: primary NSCLC with metastases to distal tibia epiphysis
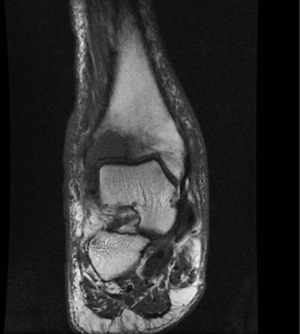
In 2016, a 78-year-old man with non-small cell lung cancer (NSCLC) presented to a radiotherapy clinic with pain in his right ankle and difficulty walking. Magnetic resonance imaging (MRI) of the right ankle revealed a heterogeneous soft tissue mass at the right distal tibial epiphysis (Figure 5). A subsequent bone scan showed increased uptake in the right anterior distal tibia and in the ribs. He was previously treated for his cancer by resection of the primary cancer and was on adjuvant chemotherapy consisting of Carboplatin and Vinorelbine, finishing his last cycle 1 month prior to his clinic visit. After consultation by radiologist and orthopedic surgeons, the lesion was deemed most likely to be metastatic, and radiotherapy was advised. The patient elected for palliative radiotherapy of 20 Gy in five fractions directed at his right lower leg and ankle. He had some relief of pain following the radiotherapy.
Case 4: primary urothelial cancer with metastases to distal tibia
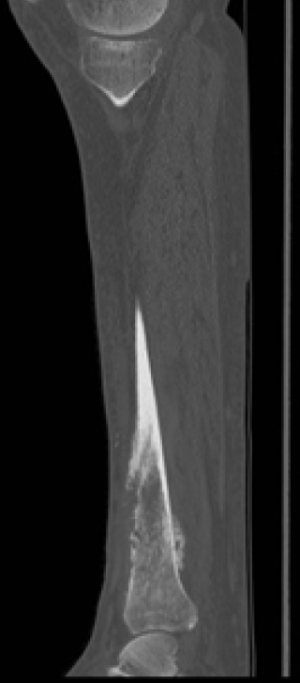
In 2016, a 77-year-old man with urothelial cancer presented to a clinic with excruciating pain and swelling in his left ankle. An X-ray revealed permeative lytic lesion in the distal tibial diametaphysis with nondisplaced spiral pathological fracture in the distal tibia and elevated periosteal reaction with destruction of anterior tibial cortex. CT scan showed a poorly defined destructive lesion in the diametaphysis with subtle extension into the distal tibial articular surface. The extent of the lesion was hard to determine but was approximated at 13 cm (Figure 6). The patient was assessed by orthopaedic surgery and subsequently underwent open reduction with internal fixation of the left distal tibia with tumour excision, and insertion of antibiotic bone cement 2 weeks later (Figure 7). Surgery was deemed successful with no complications and the patient had improved mobility and good pain relief upon discharge. One month post-surgery, the patient had developed redness and inflammation at the left tibia, possibly due to cellulitis or disease recurrence, thus post-operative radiotherapy was postponed and the patient was given antibiotics. The patient received radiotherapy of 20 Gy in five fractions directed to his lower left leg almost 2-month post-surgery.

Discussion
Bone metastases can significantly impact patient functioning and QoL, which is a particular concern for palliative cancer patients given their typically limited prognosis. In particular, bones with metastases below-the-knee may no longer be able to support the brunt of the body’s weight, interfering with patient mobility and QoL. The present case series highlights the management of four different cases of below-the-knee metastases.
Treatment options for below-the-knee metastases include radiotherapy, hormonal therapy, bisphosphonates, bone cement, and surgical intervention. Surgical fixation provides structural stabilization, pain relief, and promotes healing of the fracture. Piccioli et al. reviewed 13 patients who underwent surgery for tibial metastases. Overall QoL improved significantly, and 12 of 13 patients returned to the same activities of daily living they had prior to the tibial lesion. Patients’ ECOG index also improved significantly post-operatively (5). Therefore, surgical fixation is a recommended treatment option for impending or pathologic fractures due to below-the-knee metastases.
However, several factors must be considered prior to surgical intervention including the size and location of the metastases causing impending fracture, as well as the patient’s overall performance status and medical condition. Patients with at least a 3-month expected survival may benefit from surgery (2), whereas patients with limited survival who suffer from major complications post-operatively may not experience these benefits. This was seen Case 1, where the patient had disease progression and passed away in the interim while suffering from major surgical complications.
Another treatment option is palliative radiation therapy, which has been shown to relieve pain in 60% patients, with complete remission of pain in around 25% of patients (6). Beyond pain relief, radiotherapy has been shown the capacity to re-mineralize lytic metastases. For instance, Chow et al.’s study showed that radiation therapy increased bone density in both responders and partial responders (7). An analysis of the Dutch Bone Metastasis Study found that patients with femoral metastases with an axial cortical involvement >30 mm were at significantly increased risk of fracture. Thus, for patients with ≤30 mm of cortical involvement, palliative radiotherapy is an appropriate treatment option if the metastases are symptomatic (8). In the present case report, the patient in Case 2 elected for radiotherapy as they were not a surgical candidate while for the patient in Case 3, radiotherapy was deemed more appropriate than surgery.
In Cases 1 and 4, post-operative radiotherapy, a common and recommended practice (2), was administered. A literature search by Willeumier et al. revealed only two retrospective studies reporting improved outcomes after post-operative radiotherapy with low quality evidence due to non-standardized outcome measures, small sample sizes, and limited statistical analyses among other factors (9). However, this lack of evidence does not equate to a lack of efficacy and thus, post-operative radiotherapy should continue to be administered and better quality research is needed on the efficacy of this practice.
It is important to document the management of unusual clinical cases in order to provide optimal treatment for future patients. In our experience, surgery augmented by palliative radiotherapy was an efficacious treatment option for relieving pain in below-the-knee metastases in weight-bearing bones. In our patients not suitable for surgery, radiotherapy was effective at relieving pain and improving mobility. Multidisciplinary approaches to treating metastatic bone disease should always be considered to optimize therapeutic efficacy in order to achieve the goal of improving the QoL of the patient.
Acknowledgements
We thank the generous support of Bratty Family Fund, Michael and Karyn Goldstein Cancer Research Fund, Joey and Mary Furfari Cancer Research Fund, Pulenzas Cancer Research Fund, Joseph and Silvana Melara Cancer Research Fund, and Ofelia Cancer Research Fund.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: All patients provided verbal consent for the publication of this case series.
References
- Agarwal MG, Nayak P. Management of skeletal metastases: An orthopaedic surgeon's guide. Indian J Orthop 2015;49:83-100. [Crossref] [PubMed]
- Kelly CM, Wilkins RM, Eckardt JJ, et al. Treatment of metastatic disease of the tibia. Clin Orthop Relat Res 2003.Suppl:S219-29. [Crossref] [PubMed]
- De Geeter K, Reynders P, Samson I, et al. Metastatic fractures of the tibia. Acta Orthop Belg 2001;67:54-9. [PubMed]
- Coleman RE. Metastatic bone disease: clinical features, pathophysiology and treatment strategies. Cancer Treat Rev 2001;27:165-76. [Crossref] [PubMed]
- Piccioli A, Maccauro G, Scaramuzzo L, et al. Surgical treatment of impending and pathological fractures of tibia. Injury 2013;44:1092-6. [Crossref] [PubMed]
- Chow E, Zeng L, Salvo N, et al. Update on the systematic review of palliative radiotherapy trials for bone metastases. Clin Oncol (R Coll Radiol) 2012;24:112-24. [Crossref] [PubMed]
- Chow E, Holden L, Rubenstein J, et al. Computed tomography (CT) evaluation of breast cancer patients with osteolytic bone metastases undergoing palliative radiotherapy--a feasibility study. Radiother Oncol 2004;70:291-4. [Crossref] [PubMed]
- van der Linden YM, Kroon HM, Dijkstra SP, et al. Simple radiographic parameter predicts fracturing in metastatic femoral bone lesions: results from a randomised trial. Radiother Oncol 2003;69:21-31. [Crossref] [PubMed]
- Willeumier JJ, van der Linden YM, Dijkstra PD. Lack of clinical evidence for postoperative radiotherapy after surgical fixation of impending or actual pathologic fractures in the long bones in patients with cancer; a systematic review. Radiother Oncol 2016;121:138-42. [Crossref] [PubMed]


