Attendance of older patients with bone metastases at a multidisciplinary bone metastases clinic: an 8-year experience
Introduction
Bone is a common site of metastasis from advanced cancer and can lead to complications such as bone pain, pathological fractures, and spinal cord compression (1-3). Bone metastases are a common cause of cancer-related pain and can manifest in functional impairment and reduced quality of life in affected patients (3,4). There is a variety of efficacious treatments for palliation of symptomatic bone metastases such as radiation therapy, surgical intervention, bisphosphonates, and analgesics (5-8).
The bone metastases clinic (BMC) at Sunnybrook Odette Cancer Centre provides highly specialized, evidence-based treatment and symptom control for patients with bony metastases. Patients with complicated or symptomatic bone metastases are referred to BMC where they are seen concurrently by orthopedic surgery, radiation oncology, interventional radiology, and palliative care teams (9).
Older adult (OA) cancer patients are a unique cohort in cancer care, as they are less likely to have localized disease and often experience more symptoms than younger patients (10,11). Previous studies have demonstrated that low rates of OA patients receive curative and/or palliative treatments for cancer, due to opposing views that exist regarding the ability for older adults to endure these treatments (10,12,13). There is some speculation that age bias is a deterrent for treatment in OA patients (14). Additionally, it has been widely observed that OA patients are not well represented in clinical trials; this fact makes the results found in these trials inaccurate to apply to older patients (15,16).
The objectives of the present study were to determine the rate of OA attendance at BMC and to analyze case dispositions following BMC consultation.
Methods
The BMC is an outpatient clinic at the Odette Cancer Centre at Sunnybrook Health Sciences Centre that provides consultation to advanced cancer patients with complicated bony metastases. All patients who were referred to the BMC from 2007 to 2015 were included in the study. Demographic information including age, gender, Karnofsky Performance Status (KPS), primary cancer site, reason for referral, and case disposition were recorded in a prospectively collected database. The proportion of OA attendance was calculated for each year from the total number of patient visits. OA attendance was defined as individuals ≥65 years of age who attended the BMC, and non-OA attendance as those <65 years of age. Descriptive statistics were conducted on demographic and case disposition information. The study was approved by the institutional research ethics board of Sunnybrook Health Sciences Centre (No. 149-2017).
Results
Patient characteristics
Between 2007 and 2015, a total of 551 patients were seen in the BMC (Table 1). The median age of all patients was 64 years, and the median KPS for OA and non-OA patients was 70 and 80, respectively. The majority of patients originated from home (93.5%) with a small proportion from the hospital (4.4%) or from another location such as a nursing home (2.1%). Overall, 49.7% of all patients were OA, with OA attendance per year ranging from 45.2% to 58.7%. Trends of OA attendance by year remained relatively stable (Table 2).
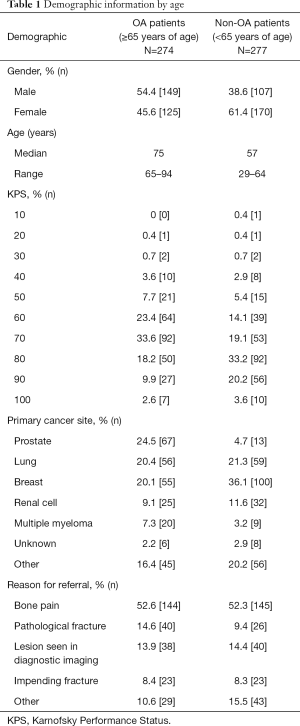
Full table
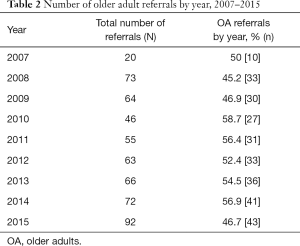
Full table
Case dispositions
The main case dispositions for all patients were orthopedic surgery or palliative radiotherapy to treat their bone metastases after BMC consultation (Table 3). Surgery was offered to 10.9% of OA patients (n=30) and 14.1% of non-OA patients (n=39). External-beam palliative radiotherapy (maximum dose: 30 Gray in 10 fractions) was offered equally to both age cohorts; 22.6% of OA patients and 22.4% of non-OA patients. A minority of patients were offered minimally invasive procedures such as vertebroplasty or cementoplasty; these procedures were offered to 4.0% of OA (n=11) and 3.2% of non-OA patients (n=9). Further investigation such as additional imaging was required in 18.2% of OA patients and 22.7% of non-OA patients. 23.0% of OA and 18.1% of non-OA patients received other case dispositions, such as the need for adjustment of pain medication or a referral to another medical specialty. No action was warranted if patients were either asymptomatic or had a stable condition, occurring in 58 OA patients and 54 non-OA patients (21.2% and 19.5% respectively).
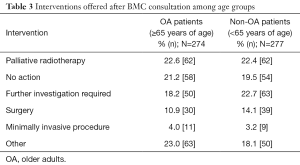
Full table
Discussion
Older adult patients comprise approximately half of all cancer cases, with estimates projecting an increase in the prevalence of OA with cancer due to the impending demographic shift expected from the baby boomer generation (16-19). Age may pose a significant deterring factor in accessing medical treatment. Several authors have highlighted the under-treatment of older cancer patients (17,19,20), with age bias as a potential reason for fewer OA patients receiving the same treatment as non-OA patients (14,19,20).
To gain a better understanding of the potential effect of age bias in physician decision-making, Foster et al. (17) conducted a study by sending case scenarios to a total of 200 physicians listed in the American Medical Association as being involved in the care of OA cancer patients. Each of the four case scenarios had two nearly identical versions, with age being the only variation. Similar to the results of the present study, Foster et al. found that the cases offering radiation were not significantly different between OA and non-OA patients. However, for 2 of the 4 hypothetical scenarios that dealt with aggressive treatments such as surgery and chemotherapy, selected treatments differed significantly based solely on the age of the patient, with the younger patient more often receiving these therapies; invasive surgical procedures were the only treatment option that slightly differed in the present study as well. Additionally, a systematic review on treatments in older females with breast and gynecological cancers found that many studies concluded that age alone was a significant factor for under-treatment with surgery, adjuvant chemotherapy and radiation, independent of all other factors (19).
A potential explanation for the age bias observed in physicians could be that OA patients have been historically excluded from clinical trials, which limits evidence of safety and efficacy of treatment in this population (15,16); this could contribute to the hesitation experienced by some physicians in exposing OA patients to these treatments. OA patients may also present with more comorbidities and lower performance status, often making their cases more complex (10,17,20); this could potentially affect the level of difficulty in treating these patients. As well, OA patients may be more likely to decline treatment offered to them due to a multitude of factors; many OA patients may face additional barriers, such as a lack of social support and limited transportation (17). Barriers such as these, in addition to advanced age, could be factors that would discourage OA patients from accepting treatment.
In the present study, relatively similar rates of OA and non-OA patients were offered subsequent treatments following consultation at the BMC, indicating that case disposition was not limited by age of the patient. This is an important observation, as several studies have concluded that OA patients can greatly benefit from the same standard treatments as non-OA patients. One retrospective analysis by Campos et al. (10) comparing radiotherapy response among OA and non-OA patients with bone metastases found that regardless of age, pain relief was equal. Liang et al. (21) measured outcomes among patients over 60 years of age after surgery for spinal metastases concluding that surgery in this cohort can provide many benefits such as improvement of pain and neurologic symptoms and restoration of functional status. However, the study cautioned that the risk of postoperative complications may be higher in an OA population, highlighting the need for awareness that more invasive treatments may still be efficacious in OA patients but with varying short- and long-term outcomes.
Contrary to the literature on the topic, OA referrals comprised a significant number of referrals in the given time period. Our study observed that OA patients were also given relatively equal opportunity for various treatment options when compared to non-OA patients. A possible reason for our positive result could be the relatively recent demographic shift resulting in more OA patients with metastatic disease and therefore more representation in the BMC. Another explanation could be the unique multidisciplinary nature of the BMC; multidisciplinary clinics allow patients to be assessed in conjunction by various specialties, allowing for treatment to be tailored to individual cases and allowing patients to see all specialists in one setting. For OA patients, this may be particularly beneficial as they tend to present with more complex clinical cases that may require more individualized treatment. As well, a multidisciplinary clinic provides streamlined access to care, with all consultations amalgamated into one visit, offering greater convenience especially given that ambulation and transportation in this demographic may be difficult.
This study has several limitations. Since this is a retrospective study, we lack details regarding presence of comorbidity and clinical reasoning for each patient’s treatment plan. Additionally, some patients were referred elsewhere to receive subsequent treatment and therefore we lack complete data on all patients to further differentiate the interventions recommended and/or offered. Not all patients were followed after consultation at the BMC and therefore information on outcomes is not available.
OA cancer patients tend to present with a more complex profile due to increased symptom burden, lower performance status, and higher rates of comorbidity. Despite this, studies have shown that cancer treatments can still have great benefit in this population. Our results suggest that OA patients are well-represented at the BMC and are given relatively equal consideration for treatment as non-OA patients. Further research is needed regarding the benefits of multidisciplinary clinics in the care of OA cancer patients.
Acknowledgements
We thank the generous support of Bratty Family Fund, Michael and Karyn Goldstein Cancer Research Fund, Joey and Mary Furfari Cancer Research Fund, Pulenzas Cancer Research Fund, Joseph and Silvana Melara Cancer Research Fund, and Ofelia Cancer Research Fund.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the institutional research ethics board of Sunnybrook Health Sciences Centre (No. 149-2017).
References
- Coleman RE. Clinical features of metastatic bone disease and risk of skeletal morbidity. Clin Cancer Res 2006;12:6243s-9s. [Crossref] [PubMed]
- Tubiana-Hulin M. Incidence, prevalence and distribution of bone metastases. Bone 1991;12 Suppl 1:S9-10. [Crossref] [PubMed]
- Oster G, Lamerato L, Glass AG, et al. Natural history of skeletal-related events in patients with breast, lung, or prostate cancer and metastases to bone: a 15-year study in two large US health systems. Support Care Cancer 2013;21:3279-86. [Crossref] [PubMed]
- Ulas A, Bilici A, Durnali A, et al. Risk factors for skeletal-related events (SREs) and factors affecting SRE-free survival for nonsmall cell lung cancer patients with bone metastases. Tumour Biol 2016;37:1131-40. [Crossref] [PubMed]
- Bedard G, Hoskin P, Chow E. Overall response rates to radiation therapy for patients with painful uncomplicated bone metastases undergoing initial treatment and retreatment. Radiother Oncol 2014;112:125-7. [Crossref] [PubMed]
- Townsend PW, Smalley SR, Cozad SC, et al. Role of postoperative radiation therapy after stabilization of fractures caused by metastatic disease. Int J Radiat Oncol Biol Phys 1995;31:43-9. [Crossref] [PubMed]
- Coleman RE, McCloskey EV. Bisphosphonates in oncology. Bone 2011;49:71-6. [Crossref] [PubMed]
- von Moos R, Body JJ, Egerdie B, et al. Pain and analgesic use associated with skeletal-related events in patients with advanced cancer and bone metastases. Support Care Cancer 2016;24:1327-37. [Crossref] [PubMed]
- Chow S, McDonald R, Yee A, et al. A multidisciplinary bone metastases clinic at Sunnybrook Odette Cancer Centre: A review of the experience from 2009-2014. J Pain Manage 2015;8:117-121.
- Campos S, Presutti R, Zhang L, et al. Elderly patients with painful bone metastases should be offered palliative radiotherapy. Int J Radiat Oncol Biol Phys 2010;76:1500-6. [Crossref] [PubMed]
- Fírvida JL, Vinolas N, Munoz M, et al. Age: a critical factor in cancer management: A prospective comparative study of 400 patients. Age Ageing 1999;28:103-5. [Crossref] [PubMed]
- Mor V, Masterson-Allen S, Goldberg RJ, et al. Relationship between age at diagnosis and treatments received by cancer patients. J Am Geriatr Soc 1985;33:585-9. [Crossref] [PubMed]
- Huang J, Zhou S, Groome P, et al. Factors affecting the use of palliative radiotherapy in Ontario. J Clin Oncol 2001;19:137-44. [Crossref] [PubMed]
- Dale DC. Poor prognosis in elderly patients with cancer: the role of bias and undertreatment. J Support Oncol 2003.11-7. [PubMed]
- Yee KW, Pater JL, Pho L, et al. Enrollment of older patients in cancer treatment trial in Canada: Why is age a barrier? J Clin Oncol 2003;21:1618-23. [Crossref] [PubMed]
- Lewis JH, Kilgore ML, Goldman DP, et al. Participation of patients 65 years of age or older in cancer clinical trials. J Clin Oncol 2003;21:1383-9. [Crossref] [PubMed]
- Foster JA, Salinas GD, Mansell D, et al. How does older age influence oncologists’ cancer management? Oncologist 2010;15:584-92. [Crossref] [PubMed]
- Balducci L, Extermann M. Management of cancer in the older person: a practical approach. Oncologist 2000;5:224-37. [Crossref] [PubMed]
- Bouchardy C, Rapiti E, Blagojevic S, et al. Older female cancer patients: importance, causes, and consequences of under-treatment. J Clin Oncol 2007;25:1858-69. [Crossref] [PubMed]
- Wildiers H, Kunkler I, Biganzoli L, et al. Management of breast cancer in elderly individuals: recommendations of the International Society of Geriatric Oncology. Lancet Oncol 2007;8:1101-15. [Crossref] [PubMed]
- Liang T, Wan Y, Zou X, et al. Is surgery for spine metastasis reasonable in patients older than 60 years? Clin Orthop Relat Res 2013;471:628-39. [Crossref] [PubMed]


