“Triggers” for referral to neurology palliative care service
Introduction
Patients with neurological diseases are one of the non-cancer groups that are most in need of the palliative care (PC) (1,2). The World Health Organization (WHO) defines PC as a clinical approach aiming at improving the quality of life of patients and their families facing the problems associated with life threatening illness (3). Palliative medicine addresses symptom control, psychosocial and spiritual needs. It is applicable early in the course of illness, in conjunction with other therapies including those aiming at cure of disease or prolonging life. In neurology, PC is mainly offered to those with incurable diseases with fatal course, either acute or chronic. Despite advancement in medical therapies, severe stroke, end-stage parkinsonism, dementia disorders and many neuromuscular diseases including motor neuron disease (MND), share grave prognosis. These lethal conditions have different trajectories in progression and produce various symptoms, resulting in stress to both patients and careers. Palliative medicine certainly has a role in helping neurological patients (4). However, neurologists may not be certain when to refer their patients to palliative service due to heterogenous trajectories in different neurological conditions. Palliative service may hence be underused. This paper aims to review the triggers for neurology PC. The term ‘triggers’ here refers to a set of pre-determined screening criteria. With unified indicators, it is hoped that clinicians can be oriented and referral can be initiated at appropriate time. We approach the triggers of neurology PC by dichotomizing into in-patient and out-patient settings.
In-patient settings
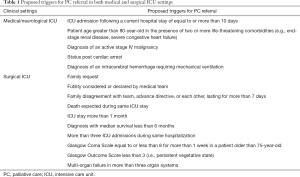
Many neurological patients who are seriously ill need prolonged in-hospital care, or even management in intensive care unit (ICU). The disease spectrum varies from acute incurable neurological disorders such as major stroke to chronic progressive diseases with acute complications such as aspiration pneumonia in MND or end-stage parkinsonism. Triggers for PC referral in the medical ICU been proposed (5). They include: (I) ICU admission following a current hospital stay of equal to or more than 10 days; (II) patient age greater than 80-year-old in the presence of two or more life-threatening comorbidities (e.g., end-stage renal disease, severe congestive heart failure); (III) diagnosis of an active stage IV malignancy; (IV) status post cardiac arrest or (V) diagnosis of an intracerebral hemorrhage (ICH) requiring mechanical ventilation (Table 1). This set of criteria has been validated and shown to shorten length of stay in the ICU without increasing mortality rate (6). These triggers have also been exploited to the neurological ICU. It has been found that the trigger of ICH with mechanical ventilation is the most common trigger in neurological critical care settings. Also, critically ill patients in the neurological ICU are more likely to have withdrawal of life-sustaining therapies (6).
Full table
For surgical ICU, proactive case-finding PC triggers have also been proposed (7). These include: (I) family request; (II) futility considered or declared by medical team; (III) family disagreement with team, advance directive, or each other, lasting for more than seven days; (IV) death expected during same ICU stay; (V) ICU stay more than 1 month; (VI) diagnosis with median survival less than 6 months; (VII) more than three ICU admissions during same hospitalization; (VIII) Glasgow Coma Scale equal to or less than 8 for more than 1 week in a patient older than 75 years old; (IX) Glasgow Outcome Score less than 3 (i.e., persistent vegetative state); (X) multi-organ failure in more than three organ systems (Table 1). It has been proposed to involve palliative team to intervene in patient management when there is prolonged dispute between parent ICU team and the family. The objective is to let a third party to discuss sensitive end-of-life issues such as withholding or withdrawing life support treatment when there is major discordant between the working team and the family. Communication and mediation skills of PC team may help to resolve challenging scenarios (7). Although these triggers are not specified for patients with neurological disorders, they may be applicable selectively if feasible.
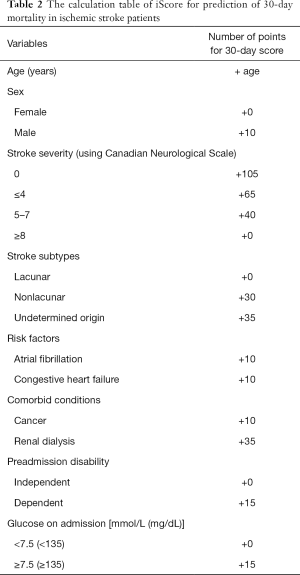
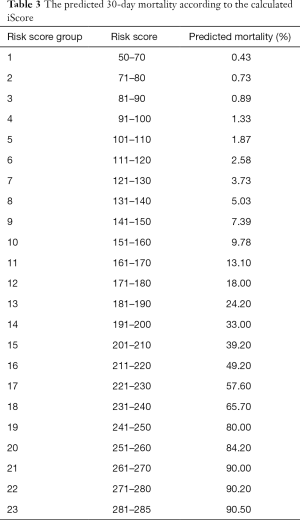
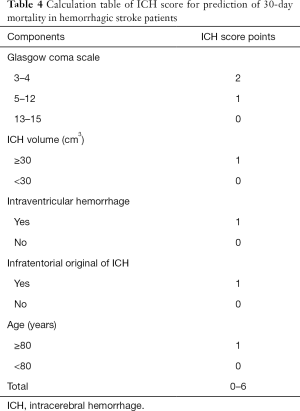
Stroke is an acute neurological condition that deserves more discussion. It is different from other chronic neurological diseases with a prolonged intractable phase so that both the patient and family can have psychological preparation and proactive planning for terminal stage of life. Cerebrovascular disease usually strikes unexpectedly. Predictive indicators may greatly help clinicians to determine whether to adopt a predominantly rehabilitative or palliative approach of further management. The prognosis prediction also directs how the medical team deliver prognostic messages to the family. Age of the patient, stroke severity upon presentation and comorbidity are proposed to be the most important prognostic indicators (8-10). Scoring systems have been developed to predict the stroke outcome. One of the example is the iScore developed by a research group in Canada (9). It depends on patient’s demographics, such as age and gender, stroke subtype, risk factors and co-morbidities, pre-admission morbidity state and glucose on admission (Table 2). It can predict the mortality risk within 30 days after ischemic stroke onset (Table 3). For hemorrhagic stroke, the ICH Score is proposed to predict the outcome (11,12). It involves the site of hemorrhage, Glasgow Coma Scale upon presentation, patient’s age, volume of the hematoma and whether there is intraventricular extension (Table 4). It can predict the 30-day mortality in hemorrhagic stroke patients (Table 5). By using these prognosis-predicting models, stroke physicians may reliably prime the family about the prognosis of the patient, discuss the end-of-life plan if appropriate and triage patient to palliative or rehabilitation facilities accordingly (13).
Full table
Full table
Full table
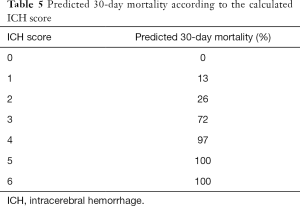
Full table
Out-patient settings
PC usually covers conditions which is progressive and eventually lead to death. Typical examples are neuromuscular diseases including MND, late stage parkinsonism and dementia due to various neurodegenerative diseases. These chronic neurological conditions have many aspects in common. They typically have a gradual deteriorating course, disabilities gradually accumulate resulting in patients’ physical and psychological stress and even careers’ burden, mortality is inevitable in the advanced stage.
In out-patient settings, the clinical presentation is usually non-emergent. It requires the vigilance of the attending clinician to identify the palliative needs of the patient. There is a lack of well conducted study investigating the optimal time of PC intervention. Authoritative bodies have suggested triggers to guide referral. The National End of Life Care Programme [2010] of National Health Service (NHS) in England recommended seven triggers for a PC approach to patients with advanced neurological conditions (14,15). They included swallowing problems, recurrent infections, marked decline in physical status; as well as the first episode of aspiration pneumonia, cognitive difficulties, weight loss and significant complex symptoms (Table 6). The complex symptoms include pain, spasticity, nausea and psychosocial and spiritual issues. For individual disease entities, various experts or academic bodies have issued various guidelines to support neurological PC.
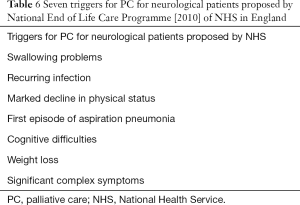
Full table
MND
MND or amyotrophic lateral sclerosis (ALS) is the condition that has attracted extensive studies. It is in fact one of the early condition that has been related to PC. Dame Cicely Saunders who was the pioneer of modern palliative medicine started her work at St. Christopher’s Hospice in London in 1960s. From the beginning, St. Christopher’s Hospice has accommodated beds devoted to MND patients (16). Because of the rapid deteriorating course of MND, early PC intervention is advocated. Difficulties in respiration or feeding could be important triggers for PC (17,18). Breathing is a major determining factor in survival and quality of life (19). Patients typically develop type II respiratory failure with carbon dioxide retention especially at night during sleep. The reasons include relaxation of airway muscles with increased resistance of airway during sleep. Also, the diaphragm is compressed by abdominal content in supine position exacerbated by loss of assistance by gravity. Early symptoms of carbon dioxide retention include daytime sleepiness and morning headache. Clearance of airway secretion is impaired in advanced stage of MND which can further aggregate ventilatory problem. Symptoms may not be a sensitive indicator for early stage of respiratory failure. Instead regular lung function monitoring should be employed once diagnosis of MND is made, even before respiratory symptoms emerge. European Federation of Neurological Societies (EFNS) has issued guideline to advise objective indicators for non-invasive ventilatory support (20).
Nasogastric tube or percutaneous endoscopic gastrostomy (PEG) may be able to lengthen the lifespan of patients with advanced neurological conditions. However, tube feeding is not accepted by all patients or their families as non-oral feeding may be considered as prolongation of suffering and deprivation of dignity. Various indications of gastrostomy have been suggested. These include significant weight loss and emergence of dysphagia (21). PEG, however, may not be suitable for patients with respiratory failure due to technical difficulties and high risk of surgical operation (22). Besides ventilatory and feeding functions, rapid deterioration in mobilization, significant weight loss and psychosocial distress could be triggers for PC.
Parkinsonism
Patients with advanced parkinsonism including terminal Parkinson’s disease (PD) and Parkinsonism-plus syndrome such as multisystem atrophy (MSA) are in need of PC (23). Potential triggers of referral include bulbar symptoms, significant limitation in mobility, non-movement symptoms such as dementia. Among these, dysphagia should be given heavy weighting. Choking can lead to aspiration pneumonia which in turn can cause bronchiectasis if the aspiration is chronic. Dysphagia can lead to food avoidance which in turn can result in insufficient fluid or caloric intake, ending in dehydration and malnutrition. Parkinsonism directly limits mobility. Significant immobility such as chair or bed bound status is associated with need of major assistance in daily activities of living. This can greatly undermine patient’s and career’s quality of life. Parkinsonism has a lot of complex symptoms not limited to mobility. These include dementia, psychosis, affective disorders, autonomic failure and sleep disorders. Also, various movement symptoms due to the disease itself or treatment such as on-off phenomenon, dyskinesia complicating dopaminergic therapy can be very difficult to manage. Specific clinical scoring scale has been proposed to assess the complex symptomatology of parkinsonism. A modified Edmonton Symptom Assessment System Scale for PD (ESAS-PD) consists of 14 items such as constipation, dysphagia, anxiety and pain (24). ESAS-PD has been shown to be effective in assessing symptoms burden in advanced PD. Patients receiving palliative intervention has significant improvement in the scale. It may be advisable to use it as a screening tool as a trigger for PC referral.
Dementia
It is widely accepted that PC can benefit patients with advanced dementia. However, whether palliative intervention should be introduced in early or later stage of dementia is controversial. In the early stage of dementia, most commonly due to Alzheimer’s disease, there are mainly cognitive symptoms with minimal somatic complaints. However, it may be a critical juncture to introduce end-of-life issues including advanced care planning and advanced directive as the patient still has the mental capacity for decision. However, patients, families or even the health care providers may have hesitance in contracting PC when there is no major physical disability (25). More focused study should be conducted on the optimal timing and delivery model of PC in dementia.
Conclusions
Involvement of PC in neurology is an emerging trend, though it has existed for long in history. The demand of neurological PC is great in view of aging populations in many countries and the incurable nature of many neurological diseases. The provision of service requires recourses and staff with palliative medicine expertise. On the other hand, more high-quality research is urgently needed. Studies on the trajectories of various neurological diseases, relationships between various symptoms and quality of life and psychosocial needs of patients with advanced neurological conditions can provide data that help to improve neurology PC.
Different models of service delivery have to be explored. Local factors including infrastructure, staff, and physical and financial stress on the patient have to be considered. Handing over from a neurologist to a PC specialist may be administratively simple and cost-saving. However, it may be less acceptable to patients and families as they may feel being abandoned. Anxiety may arise as they have to leave a physician who know well about their conditions. Another approach is that patients concomitantly attend separate clinics of the neurologist and PC specialist. However, it may mean extra burden of travelling and consultation charges for the ill patients. A combined clinic jointly attended by both the neurologist and PC specialist may enhance patient’s and family’s satisfaction. Patients can be ensured they will have continuity of care while they are introduced about the concept of PC.
Acceptance of the patient and family has great implication on the success of PC delivery. It depends on various factors including the mode of the service delivery, doctor-patient relationship and cultural background. Public education on PC approach and end-of-life issues may help to promote the development of neurology palliative service.
Above all, the vital part in developing neurology PC is the education of frontline medical staff. Common misconception among professionals includes mixing up PC with hospice care. PC aims at symptoms alleviation in physical, psychological and even spiritual and social aspects not necessary in cancer patients only. Other non-cancer group such as patients with end-stage renal failure opted for conservative treatment are also service target of PC (26). It could be introduced relatively early in the course of disease after diagnosis. There is no contradiction to any curative or disease modifying treatment. Hospice cares refer to the management at the final stage of the disease (1). The physician, nurse, allied health, social worker and supporting staff should bear the concept of palliative approach in management. Misunderstanding should be clarified by education and communication. Providing comfort, not just avoiding death, can also bring hope to patients and their families.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Boersma I, Miyasaki J, Kutner J, et al. Palliative care and neurology: time for a paradigm shift. Neurology 2014;83:561-7. [Crossref] [PubMed]
- Oliver DJ, Borasio GD, Caraceni A, et al. A consensus review on the development of palliative care for patients with chronic and progressive neurological disease. Eur J Neurol 2016;23:30-8. [Crossref] [PubMed]
- World Health Organization. WHO Definition of Palliative Care. Available online: http://www.who.int/cancer/palliative/definition/en/
- Palliative care in neurology. The American Academy of Neurology Ethics and Humanities Subcommittee. Neurology 1996;46:870-2. [PubMed]
- Norton SA, Hogan LA, Holloway RG, et al. Proactive palliative care in the medical intensive care unit: effects on length of stay for selected high-risk patients. Crit Care Med 2007;35:1530-5. [Crossref] [PubMed]
- Creutzfeldt CJ, Wunsch H, Curtis JR, et al. Prevalence and Outcomes of Patients Meeting Palliative Care Consultation Triggers in Neurological Intensive Care Units. Neurocrit Care 2015;23:14-21. [Crossref] [PubMed]
- Bradley CT, Brasel KJ. Developing guidelines that identify patients who would benefit from palliative care services in the surgical intensive care unit. Crit Care Med 2009;37:946-50. [Crossref] [PubMed]
- Frankel MR, Morgenstern LB, Kwiatkowski T, et al. Predicting prognosis after stroke: a placebo group analysis from the National Institute of Neurological Disorders and Stroke rt-PA Stroke Trial. Neurology 2000;55:952-9. [Crossref] [PubMed]
- Saposnik G, Kapral MK, Liu Y, et al. IScore: a risk score to predict death early after hospitalization for an acute ischemic stroke. Circulation 2011;123:739-49. [Crossref] [PubMed]
- Johnston KC, Wagner DP, Wang XQ, et al. Validation of an acute ischemic stroke model: does diffusion-weighted imaging lesion volume offer a clinically significant improvement in prediction of outcome? Stroke 2007;38:1820-5. [Crossref] [PubMed]
- Hemphill JC 3rd, Bonovich DC, Besmertis L, et al. The ICH score: a simple, reliable grading scale for intracerebral hemorrhage. Stroke 2001;32:891-7. [Crossref] [PubMed]
- Clarke JL, Johnston SC, Farrant M, et al. External validation of the ICH score. Neurocrit Care 2004;1:53-60. [Crossref] [PubMed]
- Holloway RG, Arnold RM, Creutzfeldt CJ, et al. Palliative and end-of-life care in stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2014;45:1887-916. [Crossref] [PubMed]
- Hussain J, Adams D, Allgar V, et al. Triggers in advanced neurological conditions: prediction and management of the terminal phase. BMJ Support Palliat Care 2014;4:30-7. [Crossref] [PubMed]
- Neurological Alliance of Ireland. End of Life Care in Long Term Neurological Conditions. Available online: http://www.nai.ie/go/resources/guidance_policy_standards/guidance_policy_standards_uk_international/end-of-life-care-in-long-term-neurological-conditions
- Borasio GD. The role of palliative care in patients with neurological diseases. Nat Rev Neurol 2013;9:292-5. [Crossref] [PubMed]
- O'Neill CL, Williams TL, Peel ET, et al. Non-invasive ventilation in motor neuron disease: an update of current UK practice. J Neurol Neurosurg Psychiatry 2012;83:371-6. [Crossref] [PubMed]
- Stavroulakis T, Baird WO, Baxter SK, et al. Factors influencing decision-making in relation to timing of gastrostomy insertion in patients with motor neurone disease. BMJ Support Palliat Care 2014;4:57-63. [Crossref] [PubMed]
- Carratu P, Spicuzza L, Cassano A, et al. Early treatment with noninvasive positive pressure ventilation prolongs survival in Amyotrophic Lateral Sclerosis patients with nocturnal respiratory insufficiency. Orphanet J Rare Dis 2009;4:10. [Crossref] [PubMed]
- Andersen PM, Borasio GD, Dengler R, et al. EFNS task force on management of amyotrophic lateral sclerosis: guidelines for diagnosing and clinical care of patients and relatives. Eur J Neurol 2005;12:921-38. [Crossref] [PubMed]
- Rooney J, Byrne S, Heverin M, et al. A multidisciplinary clinic approach improves survival in ALS: a comparative study of ALS in Ireland and Northern Ireland. J Neurol Neurosurg Psychiatry 2015;86:496-501. [Crossref] [PubMed]
- Farrero E, Anton A, Egea CJ, et al. Guidelines for the management of respiratory complications in patients with neuromuscular disease. Sociedad Espanola de Neumologia y Cirugia Toracica (SEPAR). Arch Bronconeumol 2013;49:306-13. [PubMed]
- Hudson PL, Toye C, Kristjanson LJ. Would people with Parkinson's disease benefit from palliative care? Palliat Med 2006;20:87-94. [Crossref] [PubMed]
- Miyasaki JM, Long J, Mancini D, et al. Palliative care for advanced Parkinson disease: an interdisciplinary clinic and new scale, the ESAS-PD. Parkinsonism Relat Disord 2012;18 Suppl 3:S6-9. [Crossref] [PubMed]
- van der Steen JT, Radbruch L, de Boer ME, et al. Achieving consensus and controversy around applicability of palliative care to dementia. Int Psychogeriatr 2016;28:133-45. [Crossref] [PubMed]
- Chan KY, Yip T, Yap DY, et al. Enhanced Psychosocial Support for Caregiver Burden for Patients With Chronic Kidney Failure Choosing Not to Be Treated by Dialysis or Transplantation: A Pilot Randomized Controlled Trial. Am J Kidney Dis 2016;67:585-92. [Crossref] [PubMed]


