Symptomatic palliation with radiotherapy in extensive heterotopic ossifications
Introduction
Heterotopic ossification (HTO) is the dystrophic formation of mature lamellar bone in non-osseous tissues such as muscles, connective tissue, or nerves (1,2). The most commonly affected sites are the hips followed by the elbows, knees, and temporomandibular joints (3). While its etiology can be divided into neurological, genetic and traumatic, its exact pathophysiology remains unknown. It is a potential consequence of traumatic injuries, elective surgeries, neurological insults or severe burns. The predisposing risk factors for HTO formation include male gender, diffuse idiopathic skeletal hyperostosis, ankylosing spondylitis, osteoarthritis, and previous HTO formation (2,4). Other factors which may contribute to HTO proliferation include hypercalcemia, tissue hypoxia, alterations in sympathetic nerve activity, prostaglandin activity specifically PGE2, and imbalances between parathyroid hormone and calcitonin activities (5,6).
Radiation therapy is a common prophylactic therapeutic modality administered during the perioperative period for the prevention of HTO formation which often results from major orthopedic procedures. Most of the existing literature to date describes the efficiency of radiotherapy in correspondence with surgical interventions. To our knowledge, this is the first reported case of the use of radiotherapy for HTO resulting in symptom alleviation in the absence coinciding surgeries.
Case presentation
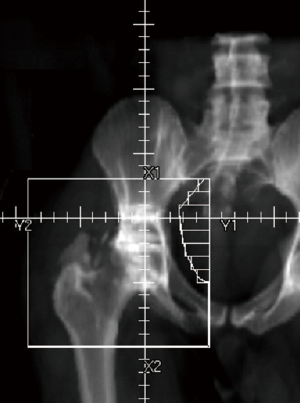
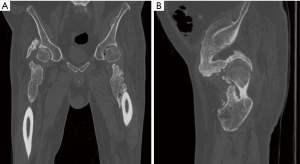
A 55-year-old wheelchair bound patient was seen at our institution for assessment of bilateral hip pain secondary to extensive HTOs (Figure 1) categorized as Brooker classification grade III. His past medical history was remarkable for C5 quadriplegia resulting from a remote motor vehicle accident, ankylosing spondylitis, hyperostosis, depression and severe obstructive sleep apnea. His medications include baclofen, acetaminophen, naproxen, pregabalin and diazepam. In view of his poor pain control, both the anesthesia and physiatry services at our institution were consulted for pain optimization but were without much success. Additionally, given his poor functional status and the high risk of recurrence, the patient was advised to forgo any surgical interventions on the advice of several orthopedic surgeons. However, due to the severity of his symptoms, he was referred to the radiation oncology service for a trial of radiation treatment as a last resort for pain management. Following a thorough discussion regarding the inherent risks and benefits of the procedure, a single 800 cGy parallel opposed external beam radiation treatment was administered to the whole pelvis and bilateral femurs (Figure 2). He tolerated the procedure well and did not experience any immediate complications.
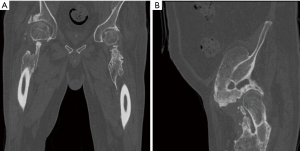
At the 6-month follow-up appointment, the patient reported significant palliation of symptoms without long-term irradiation complications. The radiographic appearance of the ossifications stabilized without signs of disease progression (Figure 3). In the end, the patient was satisfied with the results and did not require additional courses of treatment.
Discussion
Many patients who present with clinically significant HTOs suffer from severe pain, mobility limitations, functional impairment and an overall reduced quality of life (7). While those identified in the early stages of disease may be adequately addressed with physiotherapy alone, surgical excision is often thought to be necessary in the treatment of severe cases. In this patient presentation, surgical interventions were not an option due to his co-morbidities and burden of disease. Instead, he experienced a good clinical outcome towards the palliation of pain with radiotherapy alone. This in turn raises the question of patient directed goals in the treatment for HTO. While surgery remains the primary option for those with restricted range of motion, an aspect of care that radiotherapy does not address, considerations should be made for radiation as a primary option for patients whose goals are to improve the overall quality of life through pain relief and not necessarily increased mobility.
With that said, HTOs are often operated on as a secondary indication particularly in the case of revision procedures. As such, in these situations, radiotherapy should remain as a prophylactic modality for prevention of HTO progression. However, if a primary surgical indication does not exist, consideration for a trial of radiotherapy may be considered prior to undertaking a surgical approach, especially in high risk populations.
Most of the literature to date describes radiotherapy as an effective prophylactic measure for prevention of HTOs progression in patients undergoing surgical interventions. In both the preoperative and postoperative periods, it has been shown that the application of external beam radiation may reduce the risk of HTO development by as much as 80–90% (8). In such circumstances, it has been proposed that a low-dose single fraction of 700 cGy regimen provides efficacious prophylaxis while minimizing patient burden (2). However, there is limited robust evidence on the effective dose of radiotherapy for non-operative patients who require radiation for palliation of pain from HTOs. This is a topic that warrants further exploration in future research.
It is important to note that the use of radiotherapy is not without its own inherent risks and limitations. Ionization radiation acts on the relatively radiosensitive pluripotent mesenchymal stem cells. While this effectively inhibits osteoblast differentiation within the osteogenic pathway, it also potentiates the possibility of carcinogenesis and dysmorphological changes in other radiosensitive cells. A study conducted by Patel et al. demonstrated that in male patients receiving 800 cGy of hip irradiation for HTO prophylaxis, the mean absorption dose beneath the testicular shield was 20.2 cGy which is significant as sperm abnormalities have been reported with a dose as low as 15 cGy (9). Additional limitations also include the availability and costs associated with radiation administration. Ultimately, for all patients experiencing symptomatic HTO, therapeutic considerations should be made based on patient-centered goals and management options should be consistent with such goals.
Conclusions
Currently, an accepted practice for management of clinically significant symptomatic HTOs is combining surgical excision with prophylactic external beam radiation. This case study presents a patient who received pain alleviation and improvement in quality of life with radiotherapy alone which warrants the consideration of radiation therapy as a primary therapeutic option for HTOs in the future.
Acknowledgements
We thank the generous support of Bratty Family Fund, Michael and Karyn Goldstein Cancer Research Fund, Joey and Mary Furfari Cancer Research Fund, Pulenzas Cancer Research Fund, Joseph and Silvana Melara Cancer Research Fund, and Ofelia Cancer Research Fund.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Oral informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Baird EO, Kang QK. Prophylaxis of heterotopic ossification - an updated review. J Orthop Surg Res 2009;4:12. [Crossref] [PubMed]
- Popovic M, Agarwal A, Zhang L, et al. Radiotherapy for the prophylaxis of heterotopic ossification: a systematic review and meta-analysis of published data. Radiother Oncol 2014;113:10-7. [Crossref] [PubMed]
- Balboni TA, Gobezie R, Mamon HJ. Heterotopic ossification: Pathophysiology, clinical features, and the role of radiotherapy for prophylaxis. Int J Radiat Oncol Biol Phys 2006;65:1289-99. [Crossref] [PubMed]
- Taussky D, Cserhati M, Pescia R. Preoperative radiotherapy without femoral shielding for prevention of heterotopic ossification in hydroxyapatite-coated hip prostheses. Arch Orthop Trauma Surg 2001;121:271-3. [Crossref] [PubMed]
- Shehab D, Elgazzar AH, Collier BD. Heterotopic ossification. J Nucl Med 2002;43:346-53. [PubMed]
- Board TN, Karva A, Board RE, et al. The prophylaxis and treatment of heterotopic ossification following lower limb arthroplasty. J Bone Joint Surg Br 2007;89:434-40. [Crossref] [PubMed]
- Garland DE. A clinical perspective on common forms of acquired heterotopic ossification. Clin Orthop Relat Res 1991.13-29. [PubMed]
- Seegenschmiedt MH, Keilholz L, Martus P, et al. Prevention of heterotopic ossification about the hip: final results of two randomized trials in 410 patients using either preoperative or postoperative radiation therapy. Int J Radiat Oncol Biol Phys 1997;39:161-71. [Crossref] [PubMed]
- Patel H, Silverman CL, Carrascosa L, et al. Evaluation of scrotal and testicular radiation doses for heterotopic ossification prophylaxis. Am J Orthop (Belle Mead NJ) 2008;37:E163-6. [PubMed]