Impact of a dedicated palliative radiation oncology service on the use of single fraction and hypofractionated radiation therapy among patients with bone metastases
Introduction
Bone metastases are common manifestations of metastatic cancer that can be complicated by severe and debilitating pain, spinal cord compression, and pathologic fracture. Radiotherapy (RT) has been shown to effectively palliate painful bone metastases in 50–80% of patients, with up to one-third of patients achieving complete pain relief at treated sites (1,2).
Recently updated consensus guidelines from the American Society of Radiation Oncology (ASTRO) recommend single-fraction (SF) or hypo-fractionated (5 fractions or less) RT as standard of care for painful uncomplicated bone metastases (3). Multiple randomized controlled trials and meta-analyses have demonstrated equivalent pain relief with SF- and hypo-RT compared to longer treatment courses (1,4-6). Additionally, shorter treatment protocols optimize patient and caregiver convenience, carry fewer acute side effects, and are considered to be more cost-effective (4,7). The Choosing Wisely campaign has featured radiation to bone metastases to limit unnecessary treatment, and the American Academy of Hospice and Palliative Medicine recommended routine use of SF-RT for uncomplicated painful bone metastases (8,9). In spite of this evidence, shorter treatment protocols are currently underutilized in the United States and globally, and longer courses of radiation (typically 30 Gy in 10 fractions) remain more standardly used (10-12).
The Supportive and Palliative Radiation Oncology (SPRO) service was initiated at the Dana-Farber/Brigham and Women’s Cancer Center Department of Radiation Oncology on July 1, 2011 to improve the overall quality of palliative cancer care, including the improved application of evidence-base practices such as the use of short fractionation schemes among advanced cancer patients (13). The SPRO team consists of a weekly-rotating attending physician, resident, and nurse, as well as a dedicated nurse practitioner and administrative staff person. The service conducts daily rounds of palliative cancer patients under treatment and new consultation referrals. Inpatient consults are seen the same day, and outpatient consults are immediately triaged when received. Depending on the indication, outpatients may be seen the same day or up to several weeks later (e.g., post-operatively). We have previously shown that SPRO implementation improved provider-reported perceptions of the quality of palliative cancer care (14), but we have not yet investigated a possible effect on clinical endpoints. In this study, we aimed to assess the impact of the SPRO service on the frequency of SF-RT and hypo-RT delivery among patients receiving palliative cancer care for symptomatic bone metastases.
Methods
We retrospectively collected data from all patients treated with palliative-intent RT from Dana-Farber Cancer Institute/Brigham and Women’s Cancer Center Department of Radiation Oncology and three non-SPRO affiliated satellites (Libbey Park, Milford Radiation Oncology, and South Shore Radiation Oncology). We extracted age, gender, tumor type (lung, breast, prostate, or other), treatment site (non-spine or spine), date of RT, and dose fractionation from an existing database of patients receiving palliative RT. We included all patients treated between April 10, 2008 and September 17, 2014 to allow for an equivalent period before and after the introduction of the SPRO service in July 2011. We restricted our analyses to patients with bone metastases (complicated and uncomplicated) and excluded patients receiving stereotactic radiation treatments spine and non-spinal bones.
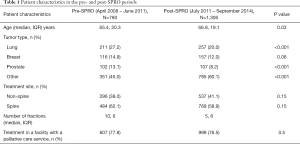
We compiled demographic and clinical characteristics as frequencies for categorical variables and as medians and interquartile ranges (IQRs) for continuous variables. We compared descriptive statistics in the pre- and post-SPRO periods with λ2-square tests for categorical variables and t-tests for continuous variables.
We used λ2 tests and multivariable logistic regression analysis (MVA) to explore the relationship between potential explanatory variables (age, sex, cancer type, treatment site, whether or not the RT facility had a dedicated palliative service, and whether or not RT occurred in the post-SPRO period) and the likelihood of receiving SF-RT or hypo-RT. We calculated the average total fractions delivered and number of RT courses per month and compared these in the pre- and post-SPRO periods using two-sided t-tests.
All analyses were performed using R version 3.1.2 and 2-sided P values <0.05 were considered significant.
Results
Between April 2008 and September 2010, we identified 2,086 instances of palliative RT for bone metastases; of these, 1,606 (77%) were delivered at the SPRO affiliated site (Dana-Farber/Brigham and Women’s Cancer Center Department of Radiation Oncology) whereas 480 (23%) were delivered at sites without a dedicated palliative radiation oncology service. Patient characteristics are listed in Table 1. Approximately 37% of our patients were treated in the pre-SPRO period, prior to July 2011; and 63% of patients were treated in the post-SPRO period. Overall, ‘other’ cancers were the most common tumor type at 54%, and the majority of bone metastases patients (60%) were referred for radiation to the spine.
Full table
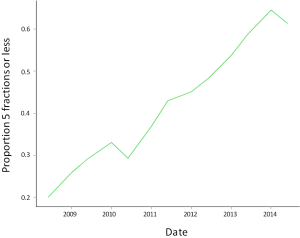
After SPRO’s implementation, the proportion of patients receiving SF-RT increased from 6.4% to 22.3% (P<0.001) and the proportion receiving hypo-RT (5 fractions or less) increased from 27.6% to 53.5% (P<0.001). Figure 1 demonstrates this rise in use of SF-RT and hypo-RT before and after SPRO’s implementation. In MVA adjusted for clinical and demographic characteristics (Table 2), patients were more likely to receive SF-RT and hypo-RT after SPRO’s implementation in July 2011. Patients receiving care at the SPRO-affiliated department were more likely to receive SF-RT and hypo-RT for bone metastases than patients at sites without a dedicated palliative service (Table 2).

Full table
Although implementation of a dedicated palliative service was associated with a reduction in dose fractionation per patient, the overall use of palliative RT increased at the SPRO affiliated site. After SPRO’s implementation, the average number of RT courses delivered for bone metastases increased from 17.4 to 25.6 per month, (+8.3, 95% CI: 4.99–11.55, P<0.001). The average total fractions per month of palliative RT for bone metastases increased from 163.5 pre-SPRO to 166.8 post-SPRO, though this was not significant (+3.22, P = NS).
Discussion
In this analysis, implementation of a dedicated palliative radiation service was associated with increased use of SF and hypo-RT as compared to longer fractionation schedules. Additionally, total courses of palliative RT increased after implementation of the palliative radiation oncology service. These results suggest that that a dedicated palliative RT service improves quality, as demonstrated by adherence to guidelines, as well as utilization of palliative RT.
To our knowledge, ours is the first study to demonstrate improvement in a clinical endpoint after implementation of a dedicated palliative RT service. Previous studies have either lacked a control period (15,16), or have reported on non-clinical endpoints (14), Research from the Rapid Response Radiotherapy Program in Toronto, Canada reported a median time from referral to consultation of 4 days, and same-day consultation of 82% of patients with metastatic bone pain and 69% of patients with brain metastases (16), After the creation of the Rapid Access Palliative Radiotherapy Program in Edmonton, Canada, 89% of patients were prescribed SF-RT for bone metastases, with treatment assessment and completion within the same day (15), While these institutions have made impressive contributions to increasing the speed and efficiency of referral and treatment, it is unclear whether these programs have altered practice patterns or led to changes in clinical outcomes.
Current data suggests that SF and hypo-RT are underutilized despite ASTRO and other national guidelines recommending their use (10-12), Barriers to the use of SF- and hypo-RT include a lack of training among healthcare providers (17), misalignment between physicians and patients on the goal of RT (18), and concerns that shorter treatments courses will result in an overall decrease in the use of RT for palliative care. The latter concern was not validated in our study; in fact, the number of RT courses and total number of treatment fractions increased after implementation of a dedicated palliative radiation oncology service.
National guidelines are increasingly recommending the integration of palliative care and radiation oncology services in order to facilitate individualized cancer care at the end of life (19). In addition to improving clinical metrics, dedicated palliative care services present an opportunity to advance education and research in palliative cancer care. Research conducted among lung cancer patients has shown that early integration of palliative care services facilitate discussions about treatment goals, prognosis, and quality of life, and decrease the likelihood of providing unnecessary care immediately before death (20). At Dana-Farber/Brigham and Women’s Cancer Center, we have previously reported improvements in physician-reported quality of communication with patients, staff experience, time spent on technical aspects of palliative cancer care, appropriateness of treatment recommendations, appropriateness of dose/fractionation decision-making, and patient follow-up after creation of the SPRO service (14).
While our study has several strengths, including its large size, multi-site pre and post design, and use of a clinical endpoint, it also has several limitations. First, the use of SF-and hypo-RT for bone metastases may depend on variables we did not include in our analysis such as patient preference, distance of the patient’s home from the treatment facility, ECOG status, concurrent systemic therapy, and tumor burden or genetics. Additionally, we were not able to characterize bone metastases as complicated (e.g., malignant spinal cord compression, pathological fracture) or uncomplicated, which may influence dose fractionation patterns. Notably, if the increase in hypofractionation is in part due to increased frequency or proportion of uncomplicated bone metastasis referral, this could be construed as a significant benefit of SPRO as patients receive palliative RT before skeletal-related events develop. Furthermore, although only one site in our analysis had a dedicated palliative radiation oncology service, practice patterns at the non-SPRO sites could have been affected by the establishment of SPRO, since all the sites are in the same network, and have some crossover between providers. However, this would only be likely to create bias towards the null, and would suggest that our estimates of the impact of the SPRO service are conservative. Finally, SPRO may not be an appropriate model for all radiation oncology institutions; given the resources required for a dedicated service, a sufficient patient volume and provider commitment are needed to support its presence.
Radiotherapy can provide needed symptom palliation for patients with bony metastases. Current guidelines recommend the use of SF- and hypo-RT for bone metastases in advanced cancer patients, however these modalities remain severely underutilized. We found that implementation of a dedicated palliative radiation oncology service increased the use of SF- and hypo-RT and overall utilization of palliative radiotherapy. Our results suggest that a dedicated palliative radiation oncology service is a promising means of both improving both the quality and utilization of palliative RT.
Acknowledgements
This work was supported by an internal grant from the Dana-Farber Cancer Institute.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the institutional ethics board of Dana-Farber/Harvard Cancer Center (protocol no. DFHCC 10-284).
References
- Chow E, Zeng L, Salvo N, et al. Update on the systematic review of palliative radiotherapy trials for bone metastases. Clin Oncol (R Coll Radiol) 2012;24:112-24. [Crossref] [PubMed]
- Chow E, Harris K, Fan G, et al. Palliative radiotherapy trials for bone metastases: a systematic review. J Clin Oncol 2007;25:1423-36. [Crossref] [PubMed]
- Lutz S, Balboni T, Jones J, et al. Palliative radiation therapy for bone metastases: Update of an ASTRO Evidence-Based Guideline. Pract Radiat Oncol 2017;7:4-12. [Crossref] [PubMed]
- Hartsell WF, Scott CB, Bruner DW, et al. Randomized trial of short- versus long-course radiotherapy for palliation of painful bone metastases. J Natl Cancer Inst 2005;97:798-804. [Crossref] [PubMed]
- Sze WM, Shelley MD, Held I, et al. Palliation of metastatic bone pain: single fraction versus multifraction radiotherapy--a systematic review of randomised trials. Clin Oncol (R Coll Radiol) 2003;15:345-52. [Crossref] [PubMed]
- Wu JS, Wong R, Johnston M, et al. Meta-analysis of dose-fractionation radiotherapy trials for the palliation of painful bone metastases. Int J Radiat Oncol Biol Phys 2003;55:594-605. [Crossref] [PubMed]
- Konski A, James J, Hartsell W, et al. Economic analysis of radiation therapy oncology group 97-14: multiple versus single fraction radiation treatment of patients with bone metastases. Am J Clin Oncol 2009;32:423-8. [Crossref] [PubMed]
- Hahn C, Kavanagh B, Bhatnagar A, et al. Choosing wisely: the American Society for Radiation Oncology's top 5 list. Pract Radiat Oncol 2014;4:349-55. [Crossref] [PubMed]
- Fischberg D, Bull J, Casarett D, et al. Five things physicians and patients should question in hospice and palliative medicine. J Pain Symptom Manage 2013;45:595-605. [Crossref] [PubMed]
- Fairchild A, Barnes E, Ghosh S, et al. International patterns of practice in palliative radiotherapy for painful bone metastases: evidence-based practice? Int J Radiat Oncol Biol Phys 2009;75:1501-10. [Crossref] [PubMed]
- Chow E, Hahn CA, Lutz ST. Global reluctance to practice evidence-based medicine continues in the treatment of uncomplicated painful bone metastases despite level 1 evidence and practice guidelines. Int J Radiat Oncol Biol Phys 2012;83:1-2. [Crossref] [PubMed]
- Popovic M, den Hartogh M, Zhang L, et al. Review of international patterns of practice for the treatment of painful bone metastases with palliative radiotherapy from 1993 to 2013. Radiother Oncol 2014;111:11-7. [Crossref] [PubMed]
- Gorman D, Balboni T, Taylor A, et al. The Supportive and Palliative Radiation Oncology Service: A Dedicated Model for Palliative Radiation Oncology Care. J Adv Pract Oncol 2015;6:135-40. [PubMed]
- Tseng YD, Krishnan MS, Jones JA, et al. Supportive and palliative radiation oncology service: impact of a dedicated service on palliative cancer care. Pract Radiat Oncol 2014;4:247-53. [Crossref] [PubMed]
- Fairchild A, Pituskin E, Rose B, et al. The rapid access palliative radiotherapy program: blueprint for initiation of a one-stop multidisciplinary bone metastases clinic. Support Care Cancer 2009;17:163-70. [Crossref] [PubMed]
- de Sa E, Sinclair E, Mitera G, et al. Continued success of the rapid response radiotherapy program: a review of 2004-2008. Support Care Cancer 2009;17:757-62. [Crossref] [PubMed]
- Tseng YD, Krishnan MS, Sullivan AJ, et al. How radiation oncologists evaluate and incorporate life expectancy estimates into the treatment of palliative cancer patients: a survey-based study. Int J Radiat Oncol Biol Phys 2013;87:471-8. [Crossref] [PubMed]
- Chen AB, Cronin A, Weeks JC, et al. Expectations about the effectiveness of radiation therapy among patients with incurable lung cancer. J Clin Oncol 2013;31:2730-5. [Crossref] [PubMed]
- Peppercorn JM, Smith TJ, Helft PR, et al. American society of clinical oncology statement: toward individualized care for patients with advanced cancer. J Clin Oncol 2011;29:755-60. [Crossref] [PubMed]
- Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 2010;363:733-42. [Crossref] [PubMed]


