
Role of bone-modifying agents in advanced cancer
Introduction
Bone involvement represents an important source of morbidity in patients with incurable malignancies. Bone metastases are particularly common in advanced breast cancer, prostate cancer, and non-small cell lung cancer (NSCLC), although they are seen across a wide spectrum of solid tumors. Additionally, nearly all patients with multiple myeloma (MM) will develop skeletal lesions at some point in the course of their disease. The presence of tumor cells in the bone microenvironment causes dysregulation of osteoclast and osteoblast activity, disturbing the normal remodeling process and weakening the structural integrity of bone (1). As a result, patients can experience severe pain, pathologic fractures, hypercalcemia, compression of the spinal cord and/or nerve roots, and systemic muscle weakness (2). Here, we review the evidence for bone-modifying agents (BMAs) including bisphosphonates and denosumab in reducing skeletal morbidity in these palliative patient populations.
Defining skeletal morbidity
Defining clinically meaningful endpoints in the palliative treatment of bone metastases is not straightforward. The term ‘skeletal-related events’ (SREs) denotes a composite endpoint of clinically defined events devised as a quantifiable measure of skeletal morbidity in clinical trials. However, the definition of SREs has evolved over time and even now remains nebulous, frequently varying from one study to another. One of the earliest studies to look at SREs as an endpoint evaluated women with bone metastases from breast cancer treated with an oral bisphosphonate (3). Here, SREs were defined as a composite endpoint of hypercalcemia, radiation or surgery for bone pain, pathologic or imminent fractures and/or a change of systemic therapy due to progression of bone metastases. More recent definitions of SREs generally consider the need for radiation or surgery to bone, pathologic fractures and spinal cord compression, plus or minus hypercalcemia of malignancy (HCM). Even excluding HCM, more than half of patients with bone metastases will experience at least one SRE (4).
Because the various definitions of SREs include asymptomatic events identified on routine imaging or laboratory tests, some have argued that symptomatic skeletal events (SSEs)—SREs accompanied by symptoms—should be preferentially employed (5). Accordingly, both SRE and SSE endpoints have been captured in clinical trials, either as incidences or time-to-event endpoints (6). While such outcomes may be considered clinically meaningful, a frequent criticism of SREs and SSEs as endpoints in studies of BMAs is the pooling of what are arguably very disparate events (7). For example, there is much greater morbidity associated with a pathologic hip or long bone fracture, as compared with the need for palliative radiation to a painful rib or vertebral metastasis. As such, while SREs and SSEs are practical endpoints that are easily captured in studies, it is important to note that they are not measures of pain or quality of life (QoL) per se, nor have they been well-validated as adequate surrogates for such.
Impact of skeletal morbidity on QoL and survival
While not validated as a surrogate endpoint, available evidence does at least support an association between the development of SREs and worse health-related QoL (HRQoL). Compared to women with metastatic breast cancer without a prior SRE, those with a history of SRE have a significantly worse baseline physical and functional well-being (8). In men with metastatic prostate cancer, clinically meaningful and statistically significant declines in physical, functional and emotional well-being were seen after the development of an SRE, specifically after radiation or fracture (9). In the AFFIRM and PREVAIL trials of enzalutamide in metastatic castrate-resistant prostate cancer (CRPC), SREs were also associated with a deterioration of HRQoL (10). In these two trials, the largest impact of SREs on HRQoL was seen in patients with spinal cord compression. SREs are also correlated with shorter overall survival (OS) (6,11,12). However, since both SREs and survival are reflections of overall disease trajectory and efficacy of anticancer treatments, a causal association between them cannot be inferred.
BMAs and skeletal morbidity
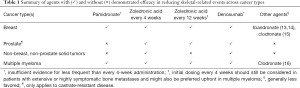
Osteoclast inhibition is an important component of the management of patients with bone involvement from cancer. There is evidence for bisphosphonates as well as for the receptor activator of nuclear factor kappa-B ligand (RANKL) inhibitor denosumab in reducing SREs. The decision regarding which specific agent to use must be individualized (see Table 1).
Full table
Bisphosphonates
Bisphosphonates are analogs of pyrophosphate that bind to the mineral bone matrix and inhibit osteoclast function and viability, thereby decreasing bone resorption and increasing mineralization (17). This class of medications can be subdivided into non-nitrogen containing and nitrogen containing bisphosphonates, with the nitrogen containing agents being more potent osteoclast inhibitors. Of the bisphosphonates in clinical use, zoledronic acid is the most potent and has the most robust evidence for reducing SREs across tumor types (18-20); compared to placebo, zoledronic acid has been shown to reduce the risk of SREs in patients with bone metastases from breast cancer, CRPC, and other solid tumors (see Table 2). It has the additional benefit of a short infusion time, most commonly being administered over 15 minutes.

Full table
In certain cancer types, however, there are reasonable data for alternative agents (13-16,18,21). For example, in the metastatic breast cancer population, several intravenous and oral bisphosphonates have evidence for efficacy versus placebo. An updated Cochrane meta-analysis published in 2017, which included 2,810 women with breast cancer and bone metastases from 9 studies, found that treatment with bisphosphonates was associated with a lower risk of SREs compared to placebo or no bisphosphonate (RR 0.86; 95% CI: 0.78–0.95; P=0.003) (22). Specific agents included intravenous pamidronate, ibandronate and zoledronic acid, as well as oral clodronate, ibandronate and pamidronate. This benefit was preserved across agents, and bisphosphonate treatment was also associated with a delay in median time to SRE, reduced bone pain, and slightly higher QoL scores compared to placebo or no bisphosphonate. There was no impact on OS. Pamidronate, most frequently administered as a monthly 90 mg infusion over 2 hours, has been consistently shown to reduce SREs in the metastatic breast cancer population (21,23,24). Pamidronate also reduces SREs compared to placebo in patients with MM (25). In contrast, a combined analysis of two randomized placebo-controlled studies of pamidronate in men with metastatic CRPC failed to demonstrate a significant overall treatment benefit in palliation of bone pain or reduction of SREs (26).
Zoledronic acid and pamidronate (each given every 3 to 4 weeks) were compared in a large randomized controlled trial of 1,648 patients with stage III MM or advanced breast cancer and at least one bone lesion (27). The proportion of patients with at least one SRE and the median time to first SRE were similar between agents. The event rate for radiation treatment to bone was significantly lower in the zoledronic acid group (15% versus 20%; P=0.031) with a similar incidence of adverse events (AEs). In the breast cancer population, zoledronic acid was more effective than pamidronate after two years of treatment in reducing the risk of SREs (RR 0.80; 95% CI: 0.66–0.97; P=0.025) (28). In a mixed-treatment meta-analysis undertaken to compare the efficacy of various bisphosphonates in patients with SREs due to metastatic breast and prostate cancer and MM, zoledronic acid seemed to be more efficacious than clodronate, pamidronate, and ibandronate (intravenous and oral) for reducing the risk of SREs (29).
Denosumab
Denosumab is a fully human monoclonal antibody against RANKL (30). In the palliative treatment of MM or bone metastases from solid tumors, it is generally administered as a 120 mg dose given subcutaneously every four weeks. The inhibition of RANKL reduces the formation, function, and survival of osteoclasts, which results in decreased bone resorption and the prevention of SREs.
Denosumab has been compared in studies mainly with the bisphosphonate zoledronic acid. Several similarly designed large international, randomized phase 3 clinical trials have been carried out in bisphosphonate naïve populations across different tumor types. In one study, 2,046 patients with breast cancer and bone metastases were randomized to receive either subcutaneous denosumab 120 mg and intravenous placebo or intravenous zoledronic acid 4 mg and subcutaneous placebo every 4 weeks (31). Denosumab was superior to zoledronic acid in delaying time to first on-study SRE (HR 0.82; 95% CI: 0.71–0.95; P=0.01 for superiority) and time to first and subsequent (multiple) on-study SREs. OS, disease progression, as well as rates of AEs and serious AEs were similar between groups. Similarly, a study of 1,904 men with metastatic CRPC randomised to denosumab or zoledronic acid also found that time to first on-study SRE was longer in the denosumab arm (HR 0.82; 95% CI: 0.71–0.95; P=0.008 for superiority) (32). Again, there were no significant differences in OS, disease progression or overall occurrences of AEs between groups. A study of 1,776 patients with MM or bone metastases from solid tumors excluding breast and prostate cancer (40% NSCLC, 10% MM, 50% other tumor types) found that denosumab was non-inferior to zoledronic acid in delaying time to first on-study SRE (HR 0.84; 95% CI: 0.71–0.98; P=0.0007 for non-inferiority) (33). Finally, a study of 1,718 patients with MM randomized to either denosumab or zoledronic acid also met its primary endpoint of non-inferiority for time to first SRE (HR 0.98; 95% CI: 0.85–1.14; P=0.010 for non-inferiority) (34).
Analgesic properties of BMAs
There is evidence to support the analgesic properties of BMAs in malignant bone pain; however, the effect is inconsistent across studies and is modest at best. As such, BMAs should be regarded as adjunct rather than primary analgesic agents for symptomatic bone metastases. In a Cochrane review evaluating women with metastatic breast cancer and bone metastases, bisphosphonates were shown to reduce bone pain (6 out of 11 studies; moderate-quality evidence) compared to placebo or no bisphosphonate (22). In men with prostate cancer and bone metastases, zoledronic acid was also more likely than placebo to be associated with clinically meaningful reductions in pain (overall mean rate 33% versus 25%; P=0.036) (35). Additionally, a non-inferiority trial of 470 patients with prostate cancer and metastatic bone pain found that a single bisphosphonate infusion (ibandronate 6 mg) was similar to a single 8 Gy dose of radiotherapy in terms of pain response (36). However, a more rapid initial response was observed with radiotherapy. In an open-label study of 604 patients with cancer (majority breast, lung, prostate and MM) and bone lesions, treatment with zoledronic acid was associated with a decrease in mean visual analog score value for pain and mean analgesic score (37). However, lack of a control group and the concomitant administration of anticancer treatments make it difficult to infer a direct treatment benefit.
Denosumab might be somewhat superior to zoledronic acid in reducing pain from malignant bone disease. In an above-mentioned study of patients with breast cancer and bone metastases randomized to either denosumab or zoledronic acid, fewer patients in the denosumab arm reported a clinically meaningful worsening of pain severity from baseline (38). There was also a trend toward delayed time to pain worsening with denosumab compared to zoledronic acid (8.5 versus 7.4 months; P=0.08). Additionally, fewer denosumab-treated patients shifted from no or low analgesic use to strong opioid analgesic use. A pooled analysis of three comparative studies of denosumab and zoledronic acid across different tumor types found that denosumab delayed the median time of onset of moderate/severe pain compared with zoledronic acid (6.5 vs. 4.7 months; HR 0.83; 95% CI: 0.76–0.92; P<0.001) (39). Denosumab also delayed the median time to clinically meaningful increases in pain interference with activity and affect compared with zoledronic acid (10.3 vs. 7.7 months; HR 0.83; 95% CI: 0.75–0.92; P<0.001).
Risks associated with BMAs
The risks of BMAs must be considered prior to their use in patients with advanced malignancies. Bisphosphonates and denosumab share many of the same adverse effects; however, there are certain side effects that are unique to each class.
Risks common to bisphosphonates and denosumab
Osteonecrosis of the jaw (ONJ) is a potentially serious complication of both bisphosphonates and denosumab. First described in 2003 (40), ONJ is characterized by current or previous treatment with antiresorptive or antiangiogenic agents, exposed bone or bone that can be probed through an intraoral or extraoral fistula in the maxillofacial region that has persisted for greater than 8 weeks, and no history of radiation treatment or metastatic disease to the jaw (41). The pathophysiology of ONJ is not entirely clear. Hypothesized mechanisms include inhibition of bone resorption and remodeling, inflammation and infection, inhibition of angiogenesis, direct soft tissue toxicity and immune dysfunction (42). Risk factors for ONJ include prolonged exposure to BMAs, dentoalveolar surgery, pre-existing inflammatory dental disease and concomitant medications including antiangiogenic agents and possibly corticosteroids (41). The rate of ONJ in prospective clinical trials appears to be in the range of 1–2%, with data from a meta-analysis suggesting a slight but not statistically significant increased risk with denosumab compared to bisphosphonates (43). Preventative measures include assessment and optimization of oral and dental health, and pre-treatment completion of any required dental procedures. In the event of ONJ, the patient should be referred to an oral and maxillofacial surgeon or dental oncologist, and the risks and benefits of surgical versus conservative management must be considered (44,45).
Hypocalcemia and electrolyte imbalances can occur with BMA treatment. Given that bone plays an integral role in calcium homeostasis (46), disruption of osteoclast function can lead to hypocalcemia and hypophosphatemia. Pre-existing impairment of compensatory mechanisms, such as vitamin D deficiency or alterations in parathyroid function, might increase the risk of significant hypocalcemia (47). In prospective phase III trials, the rates of hypocalcemia with anti-resorptive therapy range from 6–15%, with higher rates among those receiving denosumab (31-33). Periodic monitoring of calcium levels should be performed in patients receiving denosumab or bisphosphonates, and supplemental calcium and vitamin D should be considered if no contraindications exist (48).
Atypical femoral fractures have been documented in patients treated with bisphosphonates and denosumab (49,50). Thigh or groin pain may precede the fracture by several months, and the fracture may occur with minimal or no trauma (51). The pathophysiology is not entirely clear, but evidence suggests that inhibition of bone turnover can lead to the accumulation of microcracks and stress related damage, ultimately culminating in a fragility fracture (49). These are rare events, with incidence rates between 3.2 to 50 per 100,000 person-years (52). Upon identification of an incomplete or complete subtrochanteric or femoral shaft fracture not related to a malignant bone lesion, antiresorptive therapy should be discontinued, dietary calcium and vitamin D status should be assessed and supplemented as indicated, and referral to orthopedic surgery should be arranged for consideration of surgical versus conservative management.
Risks specific to bisphosphonates
Intravenous pamidronate and zoledronic acid have been associated with nephrotoxicity, including acute tubular necrosis and collapsing focal segmental glomerulosclerosis (53). The risks of nephrotoxicity appear to be increased with faster infusion times and higher dosages; hence, longer infusion times, regular monitoring of serum creatinine, and appropriate dose adjustments for renal function may reduce these risks. Acute phase reactions caused by a transient release of pro-inflammatory cytokines can occur in 15–40% of patients (54). These reactions—characterized by transient fever, myalgias and malaise—are most common with the first infusion, occurring infrequently with subsequent doses. Bisphosphonate use might also be associated with severe musculoskeletal pain independent of acute phase reaction, although data on this adverse event is mixed (55,56). Rare ocular toxicities have been documented, including uveitis and scleritis, which require prompt ophthalmology referral (57). A modest increase in the risk of atrial fibrillation and stroke has also been reported in patients receiving intravenous bisphosphonates (58).
Risks specific to denosumab
Rebound vertebral fractures have been documented in patients after discontinuation of denosumab, which can lead to a rapid elevation in markers of bone turnover and a subsequent decrease in bone mineral density (59). A period of treatment with a bisphosphonate (or at minimum one intravenous dose) should be considered in patients who discontinue denosumab. Rebound hypercalcemia with denosumab discontinuation has also been documented in young patients being treated for giant cell tumor of bone (60). There is a theoretical risk of infectious complications, but significant increases in infection rates have not been demonstrated in clinical trials for patients with cancer (31-33). Hypersensitivity reactions are rare with denosumab, but skin reactions and angioedema have been documented (61).
Extending treatment intervals for BMAs
The ability to de-escalate therapy without compromising efficacy is attractive across all areas of medicine and this holds particularly true in the palliative setting. To this end, multiple trials have examined less frequent dosing intervals of BMAs. The evidence for this approach is most robust for zoledronic acid in the metastatic breast cancer population. The ZOOM trial was a phase 3, prospective, randomised, open-label, non-inferiority trial conducted in 62 centres across Italy (62). In this study, 425 women with bone metastases from breast cancer who had already completed 12 to 15 months of zoledronic acid every 3 to 4 weeks were randomly assigned to receive zoledronic acid 4 mg once every 12 weeks or once every 4 weeks. The number of SREs was the same in both groups (15%). Additionally, there were no significant differences in bone pain or analgesic use between groups. The OPTIMIZE-2 trial was a prospective, randomized, double-blind, multicenter clinical study conducted in the United States (63). In this study, 416 women with metastatic breast cancer to bone who had received at least 9 doses of zoledronic acid or pamidronate, were randomized to zoledronic acid every 4 or 12 weeks. There was no difference in the overall rate of SREs between the more and less frequent administration groups (22.0% and 23.2%, respectively). Additionally, time to first on-study SRE was not statistically significantly different between groups.
In 121 patients with MM who received between one and two years of prior bisphosphonate therapy, the single-arm Z-MARK study evaluated the efficacy and safety of less frequent zoledronic acid administration (64). Dosing interval was based on levels of urinary N-telopeptide of type I collagen (a marker of bone turnover), which were monitored over the course of the study. The majority of patients received treatment every 12 weeks throughout the study and the investigators found that this schedule maintained a low SRE rate. Finally, the effect of longer-interval dosing of zoledronic acid was evaluated in a broader cancer population in the CALGB 70604 (Alliance) trial, which randomized 1,822 patients with bone involvement from metastatic breast cancer (46.9%), metastatic prostate cancer (37.8%), or MM (15.3%) to zoledronic acid every 4 weeks or every 12 weeks (65). In contrast to the prior de-escalation studies, patients were ineligible if they had received prior intravenous bisphosphonates or denosumab. Again, there was no statistically significant difference in the proportion of patients who developed at least one SRE between the every 4-week and every 12-week treatment groups (29.5% and 28.6%, respectively). There were also no significant differences in time to first SRE or pain scores.
While these data support the less frequent administration of zoledronic acid for patients with bone involvement from metastatic breast cancer, and to a somewhat lesser extent prostate cancer and MM, it is unclear whether this is generalizable to other tumor types or other antiresorptive agents. Reassuringly, a recently reported pragmatic trial of 263 patients with bone metastases from either breast or prostate cancer randomised to receive a BMA of their choosing (56% denosumab, 24% zoledronic acid, 20% pamidronate) on either an every 12-week or every 4-week dosing schedule found no significant difference in HRQoL measures or SSE rates between dosing schedules (66). Results of the phase III non-inferiority REDUSE trial evaluating denosumab administered every 12 versus 4 weeks in patients with breast or prostate cancer and bone metastases are pending (67). Notwithstanding these and other results, it is important to recognize that there might still exist a subgroup of patients who benefit from more frequent administration of BMAs at least upfront, such as those with extensive or highly-symptomatic bone metastases. In the MM population, extended interval treatment is likely most appropriate in those patients with responsive or stable disease.
Duration of therapy
There are no randomized trials informing the optimal duration of treatment with BMAs. However, retrospective claims-based data suggest that greater treatment persistency is associated with lower rates of SREs (68,69). ASCO guidelines for the treatment of metastatic breast cancer with bone metastases recommend indefinite treatment (70), while ASCO guidelines for the treatment of MM suggest that treatment with BMAs continue for a period of up to two years with recommencement of treatment upon relapse or with new-onset SREs (71). At least one small pilot study has demonstrated the safety and feasibility of administering zoledronic acid in the community setting to palliative patients with advanced malignancies near the end of life (72). It is important to note, however, that the patients enrolled on this study were deemed likely by their palliative care team to benefit from ongoing BMA treatment due to hypercalcemia and/or malignant bone pain. Not all patients with bone metastases and short expected survival will derive meaningful benefit from ongoing therapy, and the decision to stop treatment should be made on a case-by-case basis.
Although the development of an SRE while on treatment with a BMA might reasonably be deemed a failure of osteoclast inhibition and/or anti-cancer therapy, osteoclast inhibition should generally be continued in these cases. As there are limited data to inform the best management, consideration could be given to an alternate agent or dosing schedule. For example, after experiencing an SRE on bisphosphonate therapy, one might consider switching to denosumab (73). Similarly, after experiencing an SRE on a 12-week dosing schedule, one might reasonably switch to a 4-week schedule (71). That said, even continuing with the same BMA and schedule might improve the time to subsequent SREs (31).
Conclusions
In summary, BMAs are indicated for the prevention of SREs in most patients with skeletal involvement from metastatic solid tumors or MM. Exceptions might include those patients with a minimal burden of bone disease unlikely to develop an SRE and/or rapidly progressive visceral involvement and limited expected survival. The choice of specific agent and dosing schedule should be determined on a case-by-case basis taking into account patient preferences and disease characteristics. Zoledronic acid and denosumab have the best evidence for reducing SREs across different cancer types. In some clinical trials, denosumab has demonstrated a modest additional benefit when compared to zoledronic acid. Denosumab has the added advantage of subcutaneous administration, though is more expensive than bisphosphonates. In the MM and metastatic breast and CRPC populations, there are data to support an extended dosing interval for zoledronic acid of 12 weeks, while the evidence to support less frequent administration of other BMAs is less robust. As such, the convenience of less frequent dosing of zoledronic acid might also factor into patient preference for selected populations. In general, administration of BMAs should continue for as long as therapy is tolerated and remains in keeping with patient goals of care. In addition to capturing SREs, future trials of BMAs in patients with advanced cancer should place a greater emphasis on QoL measures and other patient reported outcomes.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Jan Gaertner, Charles B. Simone II and Fiona Lim) for the series “Clinical Challenges and Pitfalls in Early Palliative Care: Practical Knowledge and Guidance from other Medical Specialties” published in Annals of Palliative Medicine. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm.2019.08.07). The series “Clinical Challenges and Pitfalls in Early Palliative Care: Practical Knowledge and Guidance from other Medical Specialties” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Roodman GD. Mechanisms of bone metastasis. N Engl J Med 2004;350:1655-64. [Crossref] [PubMed]
- Waning DL, Guise TA. Cancer-associated muscle weakness: What's bone got to do with it? Bonekey Rep 2015;4:691. [Crossref] [PubMed]
- van Holten-Verzantvoort AT, Bijvoet OL, Cleton FJ, et al. Reduced morbidity from skeletal metastases in breast cancer patients during long-term bisphosphonate (APD) treatment. Lancet 1987;2:983-5. [Crossref] [PubMed]
- Oster G, Lamerato L, Glass AG, et al. Natural history of skeletal-related events in patients with breast, lung, or prostate cancer and metastases to bone: a 15-year study in two large US health systems. Support Care Cancer 2013;21:3279-86. [Crossref] [PubMed]
- Smith MR, Coleman RE, Klotz L, et al. Denosumab for the prevention of skeletal complications in metastatic castration-resistant prostate cancer: comparison of skeletal-related events and symptomatic skeletal events. Ann Oncol 2015;26:368-74. [Crossref] [PubMed]
- Cook RJ, Major P. Methodology for treatment evaluation in patients with cancer metastatic to bone. J Natl Cancer Inst 2001;93:534-8. [Crossref] [PubMed]
- Gomez Garcia S, Clemons M, Amir E. Rethinking end-points for bone-targeted therapy in advanced cancer. Eur J Cancer 2016;63:105-9. [Crossref] [PubMed]
- Weinfurt KP, Castel LD, Li Y, et al. Health-related quality of life among patients with breast cancer receiving zoledronic acid or pamidronate disodium for metastatic bone lesions. Med Care 2004;42:164-75. [Crossref] [PubMed]
- Weinfurt KP, Li Y, Castel LD, et al. The significance of skeletal-related events for the health-related quality of life of patients with metastatic prostate cancer. Ann Oncol 2005;16:579-84. [Crossref] [PubMed]
- Saad F, Ivanescu C, Phung D, et al. Skeletal-related events significantly impact health-related quality of life in metastatic castration-resistant prostate cancer: data from PREVAIL and AFFIRM trials. Prostate Cancer Prostatic Dis 2017;20:110-6. [Crossref] [PubMed]
- Saad F, Lipton A, Cook R, et al. Pathologic fractures correlate with reduced survival in patients with malignant bone disease. Cancer 2007;110:1860-7. [Crossref] [PubMed]
- Cetin K, Christiansen CF, Jacobsen JB, et al. Bone metastasis, skeletal-related events, and mortality in lung cancer patients: a Danish population-based cohort study. Lung Cancer 2014;86:247-54. [Crossref] [PubMed]
- Body JJ, Diel IJ, Lichinitzer M, et al. Oral ibandronate reduces the risk of skeletal complications in breast cancer patients with metastatic bone disease: results from two randomised, placebo-controlled phase III studies. Br J Cancer 2004;90:1133-7. [Crossref] [PubMed]
- Body JJ, Diel IJ, Lichinitser MR, et al. Intravenous ibandronate reduces the incidence of skeletal complications in patients with breast cancer and bone metastases. Ann Oncol 2003;14:1399-405. [Crossref] [PubMed]
- Paterson AH, Powles TJ, Kanis JA, et al. Double-blind controlled trial of oral clodronate in patients with bone metastases from breast cancer. J Clin Oncol 1993;11:59-65. [Crossref] [PubMed]
- McCloskey EV, MacLennan IC, Drayson MT, et al. A randomized trial of the effect of clodronate on skeletal morbidity in multiple myeloma. MRC Working Party on Leukaemia in Adults. Br J Haematol 1998;100:317-25. [Crossref] [PubMed]
- Fleisch H. Bisphosphonates: mechanisms of action. Endocr Rev 1998;19:80-100. [Crossref] [PubMed]
- Kohno N, Aogi K, Minami H, et al. Zoledronic acid significantly reduces skeletal complications compared with placebo in Japanese women with bone metastases from breast cancer: a randomized, placebo-controlled trial. J Clin Oncol 2005;23:3314-21. [Crossref] [PubMed]
- Saad F, Gleason DM, Murray R, et al. A randomized, placebo-controlled trial of zoledronic acid in patients with hormone-refractory metastatic prostate carcinoma. J Natl Cancer Inst 2002;94:1458-68. [Crossref] [PubMed]
- Rosen LS, Gordon D, Tchekmedyian NS, et al. Long-term efficacy and safety of zoledronic acid in the treatment of skeletal metastases in patients with nonsmall cell lung carcinoma and other solid tumors: a randomized, Phase III, double-blind, placebo-controlled trial. Cancer 2004;100:2613-21. [Crossref] [PubMed]
- Lipton A, Theriault RL, Hortobagyi GN, et al. Pamidronate prevents skeletal complications and is effective palliative treatment in women with breast carcinoma and osteolytic bone metastases: long term follow-up of two randomized, placebo-controlled trials. Cancer 2000;88:1082-90. [Crossref] [PubMed]
- O'Carrigan B, Wong MH, Willson ML, et al. Bisphosphonates and other bone agents for breast cancer. Cochrane Database Syst Rev 2017;10:CD003474. [PubMed]
- Theriault RL, Lipton A, Hortobagyi GN, et al. Pamidronate reduces skeletal morbidity in women with advanced breast cancer and lytic bone lesions: a randomized, placebo-controlled trial. Protocol 18 Aredia Breast Cancer Study Group. J Clin Oncol 1999;17:846-54. [Crossref] [PubMed]
- Hultborn R, Gundersen S, Ryden S, et al. Efficacy of pamidronate in breast cancer with bone metastases: a randomized, double-blind placebo-controlled multicenter study. Anticancer Res 1999;19:3383-92. [PubMed]
- Berenson JR, Lichtenstein A, Porter L, et al. Long-term pamidronate treatment of advanced multiple myeloma patients reduces skeletal events. Myeloma Aredia Study Group. J Clin Oncol 1998;16:593-602. [Crossref] [PubMed]
- Small EJ, Smith MR, Seaman JJ, et al. Combined analysis of two multicenter, randomized, placebo-controlled studies of pamidronate disodium for the palliation of bone pain in men with metastatic prostate cancer. J Clin Oncol 2003;21:4277-84. [Crossref] [PubMed]
- Rosen LS, Gordon D, Kaminski M, et al. Zoledronic acid versus pamidronate in the treatment of skeletal metastases in patients with breast cancer or osteolytic lesions of multiple myeloma: a phase III, double-blind, comparative trial. Cancer J 2001;7:377-87. [PubMed]
- Rosen LS, Gordon D, Kaminski M, et al. Long-term efficacy and safety of zoledronic acid compared with pamidronate disodium in the treatment of skeletal complications in patients with advanced multiple myeloma or breast carcinoma: a randomized, double-blind, multicenter, comparative trial. Cancer 2003;98:1735-44. [Crossref] [PubMed]
- Palmieri C, Fullarton JR, Brown J. Comparative efficacy of bisphosphonates in metastatic breast and prostate cancer and multiple myeloma: a mixed-treatment meta-analysis. Clin Cancer Res 2013;19:6863-72. [Crossref] [PubMed]
- Lewiecki EM. Denosumab: an investigational drug for the management of postmenopausal osteoporosis. Biologics 2008;2:645-53. [PubMed]
- Stopeck AT, Lipton A, Body JJ, et al. Denosumab compared with zoledronic acid for the treatment of bone metastases in patients with advanced breast cancer: a randomized, double-blind study. J Clin Oncol 2010;28:5132-9. [Crossref] [PubMed]
- Fizazi K, Carducci M, Smith M, et al. Denosumab versus zoledronic acid for treatment of bone metastases in men with castration-resistant prostate cancer: a randomised, double-blind study. Lancet 2011;377:813-22. [Crossref] [PubMed]
- Henry DH, Costa L, Goldwasser F, et al. Randomized, double-blind study of denosumab versus zoledronic acid in the treatment of bone metastases in patients with advanced cancer (excluding breast and prostate cancer) or multiple myeloma. J Clin Oncol 2011;29:1125-32. [Crossref] [PubMed]
- Raje N, Terpos E, Willenbacher W, et al. Denosumab versus zoledronic acid in bone disease treatment of newly diagnosed multiple myeloma: an international, double-blind, double-dummy, randomised, controlled, phase 3 study. Lancet Oncol 2018;19:370-81. [Crossref] [PubMed]
- Weinfurt KP, Anstrom KJ, Castel LD, et al. Effect of zoledronic acid on pain associated with bone metastasis in patients with prostate cancer. Ann Oncol 2006;17:986-9. [Crossref] [PubMed]
- Hoskin P, Sundar S, Reczko K, et al. A Multicenter Randomized Trial of Ibandronate Compared With Single-Dose Radiotherapy for Localized Metastatic Bone Pain in Prostate Cancer. J Natl Cancer Inst 2015. [Crossref] [PubMed]
- Kretzschmar A, Wiege T, Al-Batran SE, et al. Rapid and sustained influence of intravenous zoledronic Acid on course of pain and analgesics consumption in patients with cancer with bone metastases: a multicenter open-label study over 1 year. Support Cancer Ther 2007;4:203-10. [Crossref] [PubMed]
- Cleeland CS, Body JJ, Stopeck A, et al. Pain outcomes in patients with advanced breast cancer and bone metastases: results from a randomized, double-blind study of denosumab and zoledronic acid. Cancer 2013;119:832-8. [Crossref] [PubMed]
- von Moos R, Body JJ, Egerdie B, et al. Pain and health-related quality of life in patients with advanced solid tumours and bone metastases: integrated results from three randomized, double-blind studies of denosumab and zoledronic acid. Support Care Cancer 2013;21:3497-507. [Crossref] [PubMed]
- Edwards BJ, Gounder M, McKoy JM, et al. Pharmacovigilance and reporting oversight in US FDA fast-track process: bisphosphonates and osteonecrosis of the jaw. Lancet Oncol 2008;9:1166-72. [Crossref] [PubMed]
- Ruggiero SL, Dodson TB, Fantasia J, et al. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw--2014 update. J Oral Maxillofac Surg 2014;72:1938-56. [Crossref] [PubMed]
- Aghaloo T, Hazboun R, Tetradis S. Pathophysiology of Osteonecrosis of the Jaws. Oral Maxillofac Surg Clin North Am 2015;27:489-96. [Crossref] [PubMed]
- Qi WX, Tang LN, He AN, et al. Risk of osteonecrosis of the jaw in cancer patients receiving denosumab: a meta-analysis of seven randomized controlled trials. Int J Clin Oncol 2014;19:403-10. [Crossref] [PubMed]
- Ruggiero S, Gralow J, Marx RE, et al. Practical guidelines for the prevention, diagnosis, and treatment of osteonecrosis of the jaw in patients with cancer. J Oncol Pract 2006;2:7-14. [Crossref] [PubMed]
- Khan AA, Sandor GK, Dore E, et al. Canadian consensus practice guidelines for bisphosphonate associated osteonecrosis of the jaw. J Rheumatol 2008;35:1391-7. [PubMed]
- Li Z, Kong K, Qi W. Osteoclast and its roles in calcium metabolism and bone development and remodeling. Biochem Biophys Res Commun 2006;343:345-50. [Crossref] [PubMed]
- Rosen CJ, Brown S. Severe hypocalcemia after intravenous bisphosphonate therapy in occult vitamin D deficiency. N Engl J Med 2003;348:1503-4. [Crossref] [PubMed]
- Dhesy-Thind S, Fletcher GG, Blanchette PS, et al. Use of Adjuvant Bisphosphonates and Other Bone-Modifying Agents in Breast Cancer: A Cancer Care Ontario and American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol 2017;35:2062-81. [Crossref] [PubMed]
- Saita Y, Ishijima M, Kaneko K. Atypical femoral fractures and bisphosphonate use: current evidence and clinical implications. Ther Adv Chronic Dis 2015;6:185-93. [Crossref] [PubMed]
- Yang SP, Kim TW, Boland PJ, et al. Retrospective Review of Atypical Femoral Fracture in Metastatic Bone Disease Patients Receiving Denosumab Therapy. Oncologist 2017;22:438-44. [Crossref] [PubMed]
- Khan AA, Kaiser S. Atypical femoral fracture. CMAJ 2017;189:E542. [Crossref] [PubMed]
- Shane E, Burr D, Abrahamsen B, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 2014;29:1-23. [Crossref] [PubMed]
- Perazella MA, Markowitz GS. Bisphosphonate nephrotoxicity. Kidney Int 2008;74:1385-93. [Crossref] [PubMed]
- Olson K, Van Poznak C. Significance and impact of bisphosphonate-induced acute phase responses. J Oncol Pharm Pract 2007;13:223-9. [Crossref] [PubMed]
- Caplan L, Pittman CB, Zeringue AL, et al. An observational study of musculoskeletal pain among patients receiving bisphosphonate therapy. Mayo Clin Proc 2010;85:341-8. [Crossref] [PubMed]
- Wysowski DK, Chang JT. Alendronate and risedronate: reports of severe bone, joint, and muscle pain. Arch Intern Med 2005;165:346-7. [PubMed]
- French DD, Margo CE. Postmarketing surveillance rates of uveitis and scleritis with bisphosphonates among a national veteran cohort. Retina 2008;28:889-93. [Crossref] [PubMed]
- Wilkinson GS, Baillargeon J, Kuo YF, et al. Atrial fibrillation and stroke associated with intravenous bisphosphonate therapy in older patients with cancer. J Clin Oncol 2010;28:4898-905. [Crossref] [PubMed]
- Cummings SR, Ferrari S, Eastell R, et al. Vertebral Fractures After Discontinuation of Denosumab: A Post Hoc Analysis of the Randomized Placebo-Controlled FREEDOM Trial and Its Extension. J Bone Miner Res 2018;33:190-8. [Crossref] [PubMed]
- Uday S, Gaston CL, Rogers L, et al. Osteonecrosis of the Jaw and Rebound Hypercalcemia in Young People Treated With Denosumab for Giant Cell Tumor of Bone. J Clin Endocrinol Metab 2018;103:596-603. [Crossref] [PubMed]
- Gutierrez-Fernandez D, Cruz MJ, Foncubierta-Fernandez A, et al. Monoclonal antibody desensitization in a patient with a generalized urticarial reaction following denosumab administration. Allergy Asthma Clin Immunol 2015;11:29. [Crossref] [PubMed]
- Amadori D, Aglietta M, Alessi B, et al. Efficacy and safety of 12-weekly versus 4-weekly zoledronic acid for prolonged treatment of patients with bone metastases from breast cancer (ZOOM): a phase 3, open-label, randomised, non-inferiority trial. Lancet Oncol 2013;14:663-70. [Crossref] [PubMed]
- Hortobagyi GN, Van Poznak C, Harker WG, et al. Continued Treatment Effect of Zoledronic Acid Dosing Every 12 vs 4 Weeks in Women With Breast Cancer Metastatic to Bone: The OPTIMIZE-2 Randomized Clinical Trial. JAMA Oncol 2017;3:906-12. [Crossref] [PubMed]
- Raje N, Vescio R, Montgomery CW, et al. Bone Marker-Directed Dosing of Zoledronic Acid for the Prevention of Skeletal Complications in Patients with Multiple Myeloma: Results of the Z-MARK Study. Clin Cancer Res 2016;22:1378-84. [Crossref] [PubMed]
- Himelstein AL, Foster JC, Khatcheressian JL, et al. Effect of Longer-Interval vs Standard Dosing of Zoledronic Acid on Skeletal Events in Patients With Bone Metastases: A Randomized Clinical Trial. JAMA 2017;317:48-58. [Crossref] [PubMed]
- Clemons MJ, Ong M, Stober C, et al. A randomized trial comparing four-weekly versus 12-weekly administration of bone-targeted agents (denosumab, zoledronate, or pamidronate) in patients with bone metastases from either breast or castration-resistant prostate cancer. J Clin Oncol 2019;37:11501. [Crossref]
- Templeton AJ, Stalder L, Bernhard J, et al. Prevention of symptomatic skeletal events with denosumab administered every 4 weeks versus every 12 weeks: A noninferiority phase III trial (SAKK 96/12, REDUSE). J Clin Oncol 2014;32. [Crossref]
- Henk HJ, Kaura S. Retrospective database analysis of the effect of zoledronic acid on skeletal-related events and mortality in women with breast cancer and bone metastasis in a managed care plan. J Med Econ 2012;15:175-84. [Crossref] [PubMed]
- Hatoum HT, Lin SJ, Smith MR, et al. Zoledronic acid and skeletal complications in patients with solid tumors and bone metastases: analysis of a national medical claims database. Cancer 2008;113:1438-45. [Crossref] [PubMed]
- Van Poznak C, Somerfield MR, Barlow WE, et al. Role of Bone-Modifying Agents in Metastatic Breast Cancer: An American Society of Clinical Oncology-Cancer Care Ontario Focused Guideline Update. J Clin Oncol 2017;35:3978-86. [Crossref] [PubMed]
- Anderson K, Ismaila N, Flynn PJ, et al. Role of Bone-Modifying Agents in Multiple Myeloma: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol 2018;36:812-8. [Crossref] [PubMed]
- Marr HK, Stiles CR, Boyar MA, et al. Feasibility of administering zoledronic acid in palliative patients being cared for in the community: results of a pilot study. Curr Oncol 2010;17:69-74. [Crossref] [PubMed]
- Fizazi K, Lipton A, Mariette X, et al. Randomized phase II trial of denosumab in patients with bone metastases from prostate cancer, breast cancer, or other neoplasms after intravenous bisphosphonates. J Clin Oncol 2009;27:1564-71. [Crossref] [PubMed]


