Laparoscopic versus open mesh repair for the treatment of recurrent inguinal hernia: a systematic review and meta-analysis
Introduction
Inguinal hernia is one of the most common conditions seen in clinic, and is often treated through the general surgery department (1). Laparoscopic repair and open repair with mesh are the typical treatments for inguinal hernia, and both regimens have proved beneficial in treating inguinal hernia (2). However, recurrence, with a rate as high as 33%, poses a significant problem to the effective treatment of inguinal hernia (3,4). Both surgical approach and the size of the mesh used to repair the primary hernia influence the chance of recurrence. If the inguinal hernia reoccurs, recurrent inguinal hernia repair is a demanding procedure to perform and carries a high risk for recurrence and complications (5). Therefore, increasing the successful rate of hernia repair and reducing the recurrence and complication present a considerable challenge to the management of inguinal hernia.
For the repair of inguinal hernia, some surgeons favor the laparoscopic approach, while others recommend open repair. While open repair can result in more scar tissue and carries higher risk of testicular and nerve injury, it is much cheaper and has a shorter surgical learning curve compared to laparoscopic repair (6). Meanwhile, laparoscopic repair produces less scar tissue and requires less dissection to place the mesh; however, it is more expensive and has a longer surgical learning curve (7). Several previous studies (8-10) have compared the differences between laparoscopic and open mesh repair in the treatment of recurrent inguinal hernia; however, the results are controversial and no consensus has been reached. Moreover, recruiting patients to perform larger-sized randomized controlled trials (RCTs) of recurrent hernia repairs is challenging. Therefore, a systematic review and meta-analysis of studies on the difference between laparoscopic and open mesh repair in the treatment of recurrent inguinal hernia is urgently called for.
There have been few previous meta-analyses to compare the effectiveness of open repair and laparoscopic repair for recurrent inguinal hernia, and those that have been conducted are limited. Therefore, we conducted this meta-analysis to critically evaluate and synthesize the current evidence on the differences between laparoscopic and open mesh repair for treating recurrent inguinal hernia. We present the following article in accordance with the PRISMA reporting checklist (available at http://dx.doi.org/10.21037/apm-20-968).
Methods
Literature search
This meta-analysis was conducted in compliance with the PRISMA guidelines (11). Studies into the effects of laparoscopic and open mesh repair in the treatment of recurrent inguinal hernia were identified via a systematic search of the PubMed, EMBASE, Science Direct, Cochrane Central Register of Controlled Trials, China National Knowledge Infrastructure (CNKI), and Wanfang databases. The electronic search took into account both English- and Chinese-language articles published up to December 30, 2017, and used the following terms and/or combinations: “recurrent inguinal hernia”, “laparoscopic”, “open”, “total extraperitoneal (TEP)”, “transabdominal preperitoneal (TAPP)”, “Lichtenstein”, “RCT”. The reference lists of the retrieved studies were also reviewed and manually searched, and no attempt was made to identify unpublished reports.
Study selection criteria
The titles or abstracts of the studies were screened before a second screening of the full-text articles was conducted. The articles were judged against the following inclusion criteria: (I) the study compared the laparoscopic and open repair for recurrent inguinal hernia; (II) the study was RCT by design, regardless of whether the study was blind or not; and (III) related major outcomes such as the recurrence rate, operative time, and related complications were reported. Studies with duplicated reports and those with unbalanced matching procedures and incomplete outcome data were excluded. When a duplication occurred, we excluded the studies reported as conference proceedings and the earlier publication.
Data extraction
The two authors independently read the retrieved studies against the selection criteria. When a disagreement arose, a consensus was reached through discussion. After the studies that met the inclusion criteria had been identified, the two authors extracted the following data from each article: the authors, year of publication, country of origin, the patient demographics, the repair approach, the duration of the trial, the length of follow-up, and the study results and conclusion. If any of this data was unclear or the results were difficult to extract for meta-analysis, we attempted to contact the corresponding authors to obtain more precise and detailed information.
Interventions and outcome definitions
There are several definitions that need to be clarified: early recurrence was defined as the recurrence of the hernia during the first two months of follow-up; TEP referred to laparoscopic hernia repair with extra-peritoneal mesh placement; TAPP referred to laparoscopic hernia repair via the peritoneal cavity with extra-peritoneal mesh placement; Lichtenstein (LI) procedure referred to open tension-free mesh hernia repair; and giant prosthetic reinforcement of the visceral sac (GPRVS) was one of the methods of open preperitoneal repair with mesh.
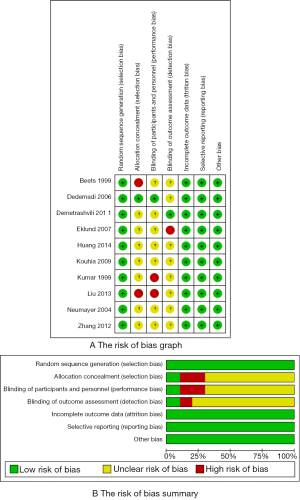
The study quality assessment
The quality of the included RCTs was assessed using the Cochrane Collaboration’s “risk of bias” tool, which includes seven domains: sequence generation, allocation concealment, blinding of participants, personnel and outcome evaluators, incomplete outcome data, selective outcome reporting, and other sources of bias. No conflicts of interest were reported or found in the study design, data collection, results analysis, and interpretation. The study quality was assessed independently by the two authors, and any discrepancies in the evaluation of study quality were discussed to reach a consensus.
Data synthesis
Data analysis was carried out using RevMan Version 5.2. The pooled estimates of outcomes were calculated using a fixed effects model or random effects model according to the difference in heterogeneity. Tests for heterogeneity and overall effects were conducted for each outcome analysis. The chi-squared statistical method was used to test for heterogeneity between the included RCTs, and the I2 statistic was adopted to detect any inconsistency. When homogeneity (if P value of χ2 test >0.10 and I2>50%) was detected, a fixed effects model was adopted, while a random effects model was used when obvious heterogeneity (P value of χ2 test >0.10 and I2>50%) was present. Dichotomous variables for each trial were expressed as an odds ratio (OR) with 95% confidence intervals (CIs), and continuous outcomes were reported as inverse variance weighted mean differences (MDs). Forest plots were used to display synthesized results. To detect publication bias, funnel plots were drawn and Egger’s test was used to test for asymmetry. The bias between studies was assessed with sensitivity analysis by removing the included studies from the data results one by one to see if the overall effect size was changed.
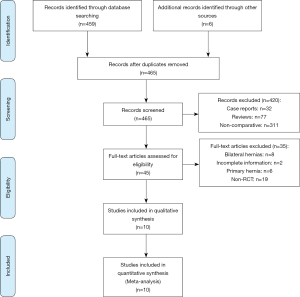
Literature search
Figure 1 shows the flowchart of study selection from the primary results of publication searches to the studies eventually included for analysis. Briefly, the first database searches and manual searching of review lists resulted in 465 citations for further crossover check. The titles and abstracts of 465 papers were accessed and examined, and we identified 45 studies as being potentially relevant for full-text review. After careful screening, 10 RCTs (12-21) were finally included for data assessment.
Study characteristics
The basic characteristics of the study population and results for various outcome measures of the eligible RCTs are summarized in Table 1. A total of 1,017 patients were involved in the 10 RCTs included for analysis, of whom 521 underwent laparoscopic mesh repair and 496 underwent open mesh repair. The included RCTs originated from different countries, with three from China, two from the USA, and one each from the Netherlands, Greece, Sweden, Finland, and the UK. The patients ranged in age from 41 to 75 years old. TAPP and TEP were used for laparoscopic mesh repair, while GPRVS and LI were used for open mesh repair. Most of the included studies had a follow-up period of more than 18 months, but four studies did not mention the follow-up period.
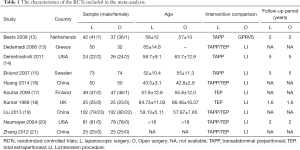
Full table
The methodological quality of the 10 RCTs is shown in Figure 2. All of the included studies reported the methods used to generate randomized sequences, such as computer-generated sequence; however, only one study reported the allocation concealment. Two studies reported that the study personnel were blinded. For blinding outcome assessment, one study was double blind, in one study the outcome evaluator was blinded, and the other studies reported no blind design. No incomplete outcome data, selective reporting, or other biases were found.
Results
Recurrence rate
Eight RCTs reported the rate of recurrence after recurrent inguinal hernia repair in both the laparoscopic repair group and the open mesh repair group. No significant difference was found in the rates of recurrence between the two groups (P=0.23; OR: 0.74, 95% CI: 0.45–1.21) (Figure 3A).
Incision infection
Six RCTs reported the incidence of incision infection after recurrent inguinal hernia repair in both the laparoscopic repair group and the open mesh repair group. There was a significant difference between the rates of incision infection in the two groups (P=0.02; OR: 0.28, 95% CI: 0.10–0.81) (Figure 3B).
Hematoma
Six RCTs reported the incidence of hematoma after recurrent inguinal hernia repair in both the laparoscopic repair group and the open mesh repair group. No significant difference was found in the incidence of hematoma between the two groups (P=0.47; OR: 0.71, 95% CI: 0.28–1.79) (Figure 3C).
Urinary retention
Five RCTs reported urinary retention after recurrent inguinal hernia repair in both the laparoscopic repair group and the open mesh repair group. No significant difference was found in urinary retention between the two groups (P=0.94; OR: 0.97, 95% CI: 0.46–2.07) (Figure 3D).
Acute pain
Two RCTs reported the incidence of acute pain after recurrent inguinal hernia repair in both the laparoscopic repair group and the open mesh repair group. There was no significant difference in the incidence of acute pain between the two groups (P=0.71; OR: 0.74, 95% CI: 0.14–3.76) (Figure 4A).
Chronic pain
Four RCTs reported the incidence of chronic pain after recurrent inguinal hernia repair in both the laparoscopic repair group and the open mesh repair group. There was a significant difference in the incidence of chronic pain experienced between the two groups (P=0.01; OR: 0.40, 95% CI: 0.20–0.82) (Figure 4B).
Operative time
Seven RCTs reported the operative time after recurrent inguinal hernia repair in both the laparoscopic repair group and the open mesh repair group. There was a significant difference in operative time between the two groups (P=0.0002; MD: 20.30, 95% CI: 9.60–31.01) (Figure 4C).
Length of hospital stay
Seven RCTs reported the length of hospital stay after recurrent inguinal hernia repair in both the laparoscopic repair group and the open mesh repair group. Length of hospital stay was significantly longer in the open mesh repair group than in the laparoscopic repair group (P<0.0001; MD: −3.65, 95% CI: −4.76 to −2.53) (Figure 4D).
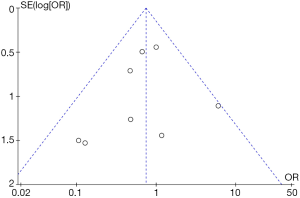
Publication bias and sensitivity analysis
According to the data reported in the included studies, the funnel plot of the recurrence rate was calculated (Figure 5). The point distribution in the funnel plot was mainly symmetrical, implying that no significant publication bias existed. For sensitivity analysis, we removed the study data one by one to compare the size of statistical effect. The results were basically the same before and after exclusion, indicating that the synthesized results were solid and reliable.
Discussion
The treatment for recurrent inguinal hernia is relatively more complex than that for the primary hernia, as surgery for recurrent inguinal hernia repair has to avoid the trauma caused by the previous surgery (20). To avoid further injury, the recurrent inguinal hernia should be treated with the application of meshes (22). Several surgical methods can be used to address this problem, including the open and laparoscopic approaches. With the rapid development of surgical techniques and equipment in recent years, surgeons have become more likely to use laparoscopic surgery to repair recurrent inguinal hernia (23). However, the differences in cost-effectiveness, patient satisfaction, and the recurrence rate between open and laparoscopic repair are still the focus of attention, and a consensus is yet to be reached regarding surgical options for recurrent inguinal hernia.
For both doctors and patients, hernia recurrence is a major problem after hernia repair (24). The recurrence rate of inguinal hernia has been reported to range from 1.1% to 33.0% depending on size, the surgical technique, and the patch used to repair the primary hernia (25,26). Due to the longer learning curve of laparoscopic hernia repair, the recurrence rate differs greatly in patients between different doctors (27). Some investigators believe doctors need to have at least experience of 30 to 250 cases of laparoscopic surgery (28). Another factor affecting the recurrence rate is the follow-up period. Recurrent inguinal hernia after laparoscopic surgery usually occurs within 12 months after the operation, whereas recurrent inguinal hernia after open surgery mainly occurs within 30 to 60 months (29). Most of our included studies had follow-up periods of longer than 18 months, and the results indicated there to be no difference in the recurrence rate between laparoscopic repair and open hernia repair, which is consistent with previous meta-analyses (8,30).
Although the use of patches in hernia repair has significantly reduced the recurrence rate, it has also made the procedure more complex and has increased the incidence of local infection (range after surgery, 0 to 9%) through the inflammatory response it induces (31). Laparoscopic surgery, as a minimally invasive approach, can reduce the incidence of infection-related complications, mainly because it eliminates the need for extensive dissection or separation of tissue (32). Our meta-analysis showed that the laparoscopic group had less wound infection than the open tension-free group, indicating that laparoscopic hernia repair is more advantageous over the open hernia repair in reducing the rate of incision infection.
Postoperative hematoma is also very common in clinical practice, and conservative treatments are used in most condition. Several previous studies (33,34) have shown that wound hematoma or hematoma is more common in open repair groups when compared with laparoscopic surgery groups. In our meta-analysis, the incidence of hematoma was similar between the open tension-free and laparoscopic surgery groups. This result may be attributed to it being more difficult to detect the retroperitoneal hematoma in laparoscopic surgery than in open repair surgery.
Urinary retention is a concern of peritoneal surgery. A retrospective analysis showed that, rather than hernia type and surgical site selection, anesthesia may be the most closely related factor to urinary retention owing to its direct pharmacological effect on bladder function. In our meta-analysis, almost all of the laparoscopic procedures were performed under general anesthesia, while a variety of anesthesia methods were used in the open group, but no statistically significant difference was found between the groups.
Pain after the hernia repair is extremely common, and is one of the two most common causes of patient complaints. With the development of material technology, chronic pain has been shown to be lower after patch repair than after suture repair (35). Chronic pain after hernia repair may be neurogenic (36,37), but the relation with surgery is still unclear. In our meta-analysis, the results revealed no significant difference in postoperative acute pain, while the incidence of chronic pain in the laparoscopic group was significantly lower than that in the open repair group, which may be because the laparoscopic approach reduces the risk of damaging the inguinal nerve.
There are variations in the operative times reported for laparoscopic and open hernia repair surgery, but most studies agree that the operative time of laparoscopic surgery is longer than that of open repair. We believe that the length of operative time mainly depends on the proficiency of the surgeon; the learning curve for laparoscopic hernia repair is much longer than that of open repair, but as the number of laparoscopic approach cases performed by the surgeon rises, the operation time can be significantly shortened (38).
Due to the significant difference in the length of hospital stay between the groups, we performed subgroup analysis based on countries. The subgroup analysis also showed that the postoperative hospital stay in the laparoscopic group was significantly shorter than that in the open repair group. With less injury caused by the incision in the laparoscopic approach, it is clear why its recovery time is considerably shorter (39).
Conclusions
In conclusion, there were no statistically significant differences in the recurrence rate or the incidence of hematoma, urinary retention, or acute pain between the laparoscopic and open group in the treatment of recurrent inguinal hernia. The incision infection rate is much lower with the laparoscopic approach and the length of hospital is much shorter than with open repair, but the laparoscopic approach does carry a longer operative time. Ultimately, the choice between laparoscopic and open mesh repair for the treatment of recurrent inguinal hernia should be based on the patient’s specific conditions and the proficiency of the operating surgeon.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-968
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-968). The authors have no conflicts of interest to declare
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Burcharth J, Pommergaard HC, Bisgaard T, et al. Patient-related risk factors for recurrence after inguinal hernia repair: a systematic review and meta-analysis of observational studies. Surg Innov 2015;22:303-17. [Crossref] [PubMed]
- Yang X, Aihemaiti M, Zhang H, et al. Mesh-preservation approach to treatment of mesh infection after large incisional ventral hernia repair—how I do it. Ann Transl Med 2019;7:698. [Crossref] [PubMed]
- Burcharth J. The epidemiology and risk factors for recurrence after inguinal hernia surgery. Dan Med J 2014;61:B4846. [PubMed]
- Burcharth J, Andresen K, Pommergaard HC, et al. Recurrence patterns of direct and indirect inguinal hernias in a nationwide population in Denmark. Surgery 2014;155:173-7. [Crossref] [PubMed]
- Dedemadi G, Kalaitzopoulos I, Loumpias C, et al. Recurrent inguinal hernia repair: what is the evidence of case series? A meta-analysis and metaregression analysis. Surg Laparosc Endosc Percutan Tech 2014;24:306-17. [Crossref] [PubMed]
- Dallas KB, Froylich D, Choi JJ, et al. Laparoscopic versus open inguinal hernia repair in octogenarians: a follow-up study. Geriatr Gerontol Int 2013;13:329-33. [Crossref] [PubMed]
- Esposito C, Escolino M, Turra F, et al. Current concepts in the management of inguinal hernia and hydrocele in pediatric patients in laparoscopic era. Semin Pediatr Surg 2016;25:232-40. [Crossref] [PubMed]
- Pisanu A, Podda M, Saba A, et al. Meta-analysis and review of prospective randomized trials comparing laparoscopic and Lichtenstein techniques in recurrent inguinal hernia repair. Hernia 2015;19:355-66. [Crossref] [PubMed]
- Esposito C, St Peter SD, Escolino M, et al. Laparoscopic versus open inguinal hernia repair in pediatric patients: a systematic review. J Laparoendosc Adv Surg Tech A 2014;24:811-8. [Crossref] [PubMed]
- O'Reilly EA, Burke JP, O'Connell PR. A meta-analysis of surgical morbidity and recurrence after laparoscopic and open repair of primary unilateral inguinal hernia. Ann Surg 2012;255:846-53. [Crossref] [PubMed]
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. [Crossref] [PubMed]
- Beets GL, Dirksen CD, Go PM, et al. Open or laparoscopic preperitoneal mesh repair for recurrent inguinal hernia? A randomized controlled trial. Surg Endosc 1999;13:323-27. [Crossref] [PubMed]
- Dedemadi G, Sgourakis G, Karaliotas C, et al. Comparison of laparoscopic and open tension-free repair of recurrent inguinal hernias: a prospective randomized study. Surg Endosc 2006;20:1099-104. [Crossref] [PubMed]
- Demetrashvili Z, Qerqadze V, Kamkamidze G, et al. Comparison of Lichtenstein and laparoscopic transabdominal preperitoneal repair of recurrent inguinal hernias. Int Surg 2011;96:233-8. [Crossref] [PubMed]
- Eklund A, Rudberg C, Leijonmarck CE, et al. Recurrent inguinal hernia: randomized multicenter trial comparing laparoscopic and Lichtenstein repair. Surg Endosc 2007;21:634-40. [Crossref] [PubMed]
- Huang G, Wen G. Laparoscopic inguinal hernia repair treatment of recurrent inguinal hernia treatment. Huaihai Medicine 2014;32:39-40.
- Kouhia ST, Huttunen R, Silvasti SO, et al. Lichtenstein hernioplasty versus totally extraperitoneal laparoscopic hernioplasty in treatment of recurrent inguinal hernia--a prospective randomized trial. Ann Surg 2009;249:384-7. [Crossref] [PubMed]
- Kumar S, Nixon SJ, MacIntyre IM. Laparoscopic or Lichtenstein repair for recurrent inguinal hernia: one unit's experience. J R Coll Surg Edinb 1999;44:301-2. [PubMed]
- Liu D. Effect of peritoneal laparoscopic tonic hernia repair on recurrent inguinal hernia in the elderly. China Health Industry 2013;8:12-6.
- Neumayer L, Giobbie-Hurder A, Jonasson O, et al. Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 2004;350:1819-27. [Crossref] [PubMed]
- Zhang P. Tension-free hernia repair surgery for recurrent inguinal hernia treatment. Modern Diagnosis and Treatment 2012;23:1978-83.
- Bisgaard T, Bay-Nielsen M, Christensen IJ, et al. Risk of recurrence 5 years or more after primary Lichtenstein mesh and sutured inguinal hernia repair. Br J Surg 2007;94:1038-40. [Crossref] [PubMed]
- Aufenacker TJ, de Lange DH, Burg MD, et al. Hernia surgery changes in the Amsterdam region 1994-2001: decrease in operations for recurrent hernia. Hernia 2005;9:46-50. [Crossref] [PubMed]
- Wang YT, Mehes MM, Naseem HR, et al. Assessing the impact of short-term surgical education on practice: a retrospective study of the introduction of mesh for inguinal hernia repair in sub-Saharan Africa. Hernia 2014;18:549-56. [Crossref] [PubMed]
- Batabyal P, Haddad RL, Samra JS, et al. Inguinal hernia repair with Parietex ProGrip mesh causes minimal discomfort and allows early return to normal activities. Am J Surg 2016;211:24-30. [Crossref] [PubMed]
- Lourenço A, da Costa RS. The ONSTEP inguinal hernia repair technique: initial clinical experience of 693 patients, in two institutions. Hernia 2013;17:357-64. [Crossref] [PubMed]
- Al Chalabi H, Larkin J, Mehigan B, et al. A systematic review of laparoscopic versus open abdominal incisional hernia repair, with meta-analysis of randomized controlled trials. Int J Surg 2015;20:65-74. [Crossref] [PubMed]
- Mathur S, Lin SY. The learning curve for laparoscopic inguinal hernia repair: a newly qualified surgeon perspective. J Surg Res 2016;205:246-51. [Crossref] [PubMed]
- Alkhaffaf B, Decadt B. Litigation following groin hernia repair in England. Hernia 2010;14:181-6. [Crossref] [PubMed]
- Bobo Z, Nan W, Qin Q, et al. Meta-analysis of randomized controlled trials comparing Lichtenstein and totally extraperitoneal laparoscopic hernioplasty in treatment of inguinal hernias. J Surg Res 2014;192:409-20. [Crossref] [PubMed]
- Falagas ME, Kasiakou SK. Mesh-related infections after hernia repair surgery. Clin Microbiol Infect 2005;11:3-8. [Crossref] [PubMed]
- Bliziotis IA, Kasiakou SK, Kapaskelis AM, et al. Mesh-related infection after hernia repair: case report of an emerging type of foreign-body related infection. Infection 2006;34:46-8. [Crossref] [PubMed]
- Paganini AM, Lezoche E, Carle F, et al. A randomized, controlled, clinical study of laparoscopic vs open tension-free inguinal hernia repair. Surg Endosc 1998;12:979-86. [Crossref] [PubMed]
- McCormack K, Scott NW, Go PM, et al. Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev 2003.CD001785. [PubMed]
- EU Hernia Trialists Collaboration. Repair of groin hernia with synthetic mesh: meta-analysis of randomized controlled trials. Ann Surg 2002;235:322-32. [Crossref] [PubMed]
- Poobalan AS, Bruce J, King PM, et al. Chronic pain and quality of life following open inguinal hernia repair. Br J Surg 2001;88:1122-6. [Crossref] [PubMed]
- Callesen T. Inguinal hernia repair: anaesthesia, pain and convalescence. Dan Med Bull 2003;50:203-18. [PubMed]
- Bisgaard T, Bay-Nielsen M, Kehlet H. Re-recurrence after operation for recurrent inguinal hernia. A nationwide 8-year follow-up study on the role of type of repair. Ann Surg 2008;247:707-11. [Crossref] [PubMed]
- Hamza Y, Gabr E, Hammadi H, et al. Four-arm randomized trial comparing laparoscopic and open hernia repairs. Int J Surg 2010;8:25-8. [Crossref] [PubMed]