Predicting discharge of palliative care inpatients by measuring their heart rate variability
Introduction
“When will I be discharged from the hospital?” is one of the most commonly questions asked by patients. Home discharge is a major challenge for patients with advanced cancer as well as their families and health care professionals (1). The likelihood and the time point of discharge are important for planning discharge management. In contrast to other fields of medicine, we have few validated tools to predict the likelihood of discharge in patients with advanced cancer (1,2). The improvement of symptoms on the Edmonton symptom assessment scale (ESAS) is a validated tool for the assessment of physical symptoms in palliative care. It constitutes an important prognostic factor and is correlated with the improvement of survival (3). However, at the time of admission to a palliative care unit (PCU) one cannot predict whether the patient’s symptoms will improve. Estimation of the probability of discharge in such patients has not been investigated yet. In an EU-wide assessment it was found that friends and relatives provided three billion unpaid care hours (5.2 hours per EU citizen), amounting to about 23.2 billion Euros (4). Thus, discharge is obviously a major challenge for patients with advanced cancer and their families. Referral to palliative care tends to occur rather late. In view of the high cost of palliative care and the fact that functionally dependent patients are unlikely to return home (5,6), it would be meaningful to focus on prognosis as well as the likelihood of discharge. A predictor of home discharge at the time of admission would enable caregivers to accompany patients and family members effectively through this process. It would also permit timely organization of home care, ideally enabling a patient to spend as much time as possible in the home environment. We hypothesized that analysis of the autonomic nervous system and the detection of dysautonomia might influence the likelihood of patients being discharged from a PCU and serve as a predictor. Autonomic dysfunction is associated with shorter survival. Every organ in the body is innervated by the autonomic nervous system. In advanced cancer patients, dysfunction of the autonomic nervous system identified by measuring heart rate variability (HRV) was found to be associated with a lower performance status and shorter survival (7,8). A patient population being admitted to a PCU has not been studied so far. We hypothesized that the degree of autonomic dysfunction is correlated with a shorter survival probability. Analysis of HRV is a means of obtaining data on standardized parameters of the autonomic nervous system. Sinus node cells generate a basal rhythm, which is modulated by the autonomic nervous system. Usually the ECG-RR interval changes with each heartbeat. An unchanged heart rate is regarded as an unfavorable clinical sign. Measurement of HRV provides standard parameters for the function of the autonomic nervous system. It is measured as the standard deviation of total normal R-R intervals. HRV has been poorly investigated in palliative care. Dysregulation of the autonomic nervous system is a common phenomenon in patients with advanced cancer (9). A limited body of data has demonstrated the stability of HRV on 24-hour monitoring, with 24-hour indices being stable and free of the placebo effect (10). Chronic stress causes a vegetative imbalance and weakening of the sympathetic and parasympathetic nervous system. The inflammatory response is regulated by the nervous system, which also controls heart rate and other vital functions. In the absence of precise regulation, deficiencies or excesses of the inflammatory response increase morbidity and reduce life expectancy (11). Pain increases sympathetic activity and decreases vagal-parasympathetic activity (12).
Fairchild et al. evaluated the ability of a multidisciplinary team to predict patients’ discharge and concluded that the most common factors influencing correct prediction were the Karnofsky performance status scale (KPS), the extent of disease, and histology (13).
The purpose of this prospective study was to determine whether measurement of the autonomic nervous system would help in predicting patients’ discharge from a PCU. KPS and palliative performance scale (PPS) were also assessed. KPS and PPS serve to measure the level of patient activity as well as requirements for medical care, and have been widely used for the general assessment of patients suffering from cancer (14-17).
Materials and methods
We conducted a prospective single-center cohort study to identify the association between measurement of the autonomic nervous system and the likelihood of discharge. The study period extended from August 2012 to August 2013. Sixty consecutive patients suffering from advanced cancer, who were admitted to a PCU, consented to the investigation and were able to communicate, were included in the study. The study assistant visited the ward without prior notice and included all patients admitted on the respective day, who fulfilled the inclusion criteria. The PCU at the Medical University of Vienna is hospital based, comprises 12 beds, and mainly attends to cancer patients. Its principal task in this regard is to improve the health of patients with advanced cancer and assist their families in transferring the patients to home care supported by mobile palliative teams. Based on statistics, about 50% of patients achieve this goal while the remaining patients die at the ward. The mean length of the patients’ stay at the ward is 14 days. Patients with atrial fibrillation, arrhythmias, those taking beta blockers, patients with a pacemaker, and heart- or lung-transplanted patients were excluded from the study because physiologic HRV is no longer present in these conditions. The study was approved by the local ethics committee. Written informed consent was obtained from each patient. KPS and PPS were rated by one of three doctors of the palliative care team. Twenty- to 24-hour peak-to-peak HRV measurement with a sampling rate of 4,000 Hz (Medilog® AR12plus) was performed. HF, LF, total power, PNN50 and LOG LF/HF, serving as benchmarks of total heart rate, were measured (Supplement 1).
Linear correlation was checked between recorded parameters and the number of days of hospitalization (from admission to discharge). Discharge was defined as either the day of discharge from hospital or the day of death. All statistical analysis was performed using the Statistical Package for Social Sciences (SPSS) 17.0 software (SPSS Inc., Chicago, IL, USA). P values <0.05 (α) were considered to indicate statistical significance; all tests were two-sided if not mentioned otherwise. Median, range (minimum to maximum), mean and standard deviation were applied for description of data, as well as percentages (of valid cases). For comparing means/medians in two samples, t-tests (parametric test for two independent samples) or the Mann-Whitney U-test (nonparametric test for two independent samples) were used. Multivariate testing of mean differences between discharged and deceased patients by analysis of variance was not permitted for HRV parameters (homogeneity of variances and covariances was not given), so alternatively t-tests and Bonferroni correction was applied. Multivariate testing was permitted for parameters of mobility (homogeneity of variances and covariances were given). Bivariate linear relations were checked by Pearson’s r (for interval-scaled variables) or Spearman’s ρ correlations (nonparametric).
Results
Sixty patients were included in the study (26 men and 34 women; 43.3% versus 56.7%). Discharge was achieved in 45% of patients (27/60) while 55% of patients (33/60) died at the PCU. On the basis of our exclusion criteria approximately 15% of all patients admitted between August 2012 and August 2013 were excluded from the study.
The study cohort consisted of a heterogeneous group of malignancies, of which lung (36%) and breast cancer (32.4%) were the most common ones (Table 1). The patients’ median age was 64 years (range, 41-88 years). The median duration of stay for discharged patients was 15.2 days (range, 2-37 days) while the median duration of stay for deceased patients was 13.6 days (range, 3-57 days; P=0.541). A significant mean difference could not be determined for any HRV parameter. However, some descriptive differences were observed. Mean HF (vagal activity) and total power (total variability) tended to be higher in patients who were discharged than in those who died, but did not achieve significance (Table 2). Considering the subgroup of patients who were discharged, and correlating HRV parameters with the days until discharge, we noticed a negative correlation (higher HRV values were associated with a lower number of days until discharge), but the correlations were minor and not significant. In deceased patients, the correlation between HRV parameters and the number of days until death was not significant. The absence of significance may have been due to the limited sample size and the heterogeneous nature of the sample (large standard deviations). Median KPS on admission was 56.2 (range, 40-80) for the entire cohort, and was significantly higher in discharged patients (60.7; range 40-80) compared to deceased patients (52.4; range, 40-80; P=0.008 multivariate; P=0.002 univariate). Median PPS on admission was identical with median KPS on admission (56.2; range, 40-80) for the entire group of patients, and was significantly higher in discharged patients (60.7; range, 40-80) than in deceased patients (54.2; range, 40-80; P=0.008 multivariate; P=0.002 univariate). Median PPS was similar in discharged patients (22.3%; range, 16-34) and deceased patients (23.0%; range, 18-35; P= ns). Higher KPS or PPS scores were associated with a greater number of days until death. Among patients who died, lower KPS and PPS scores were correlated with the number of days until death. Higher KPS and PPS were significant predictors of the likelihood of discharge.
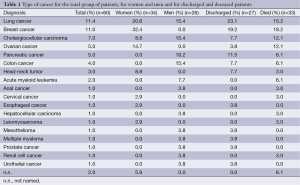
Full table
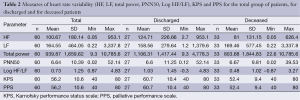
Full table
Discussion
Home discharge after hospital admission to an inpatient PCU is a major challenge for patients with advanced cancer as well as their professional and family caregivers. Data concerning prognosis in this context are scarce. Referral to a specialized palliative care center usually occurs late in the course of the disease (5). Palliative care inpatients defy simple comparison because of the heterogeneity of their malignant diseases and disease-specific demands. It would be useful to predict a patient’s propensity for deterioration at the time of his/her admission to a PCU. Symptoms such as fatigue, weakness, poor intake of food and fluids, reduced cognition, a gaunt appearance, or difficulties in swallowing medicine might be signs of approaching death. The reasons for referral to a PCU are mainly pain and emotional burden by way of anxiety, depression, or grief (18). The circadian rhythm is frequently disturbed in patients undergoing palliative care treatment. Their quality of life may be impaired by the burden of symptoms, pain, fatigue, sleeping difficulties, or a poor performance status.
Measurement of HRV is a simple and non-invasive tool. Although HRV data did not achieve significance in respect of discharge in the present study, the measurement of HRV might provide information about a patient’s circadian rhythm. Patients with advanced cancer are known to have similar HRV components during the day and at night, thus indicating abolishment of circadian fluctuations in HRV. In practical terms, this might serve as an indication for the severity of autonomic dysfunction and could be used to better estimate the chances of patients being discharged. If future studies were to establish the significance of this parameter, it may be easier for clinicians to decide, at the very start of a patient’s hospitalization, whether he/she will be eventually discharged to go home.
Twenty-hour HRV measurement is a non-invasive tool for assessing a patient’s circadian rhythm. In studies conducted thus far, the measurement of HRV has been mainly used in cardiology. The significance of HRV as an independent parameter of cardiovascular risk has been established in several studies (19-23). These studies show that HRV might serve as a prognostic parameter. HRV-measurement is performed with a small portable five-point ECG. This non-invasive and painless procedure was performed over 24 hours after admission and did neither lead to any physical inconvenience nor ethical difficulties in the included patients or their relatives.
Conclusions
We conclude that the subject calls for further investigation. The deterioration of the autonomic nervous system in cancer patients is known to be a predictor of death (8). The mean survival of patients who died was a mere 13.6 days while that of discharged patients was definitely longer, although we did not measure the latter.
Apart from prognostic reasons, the likelihood of discharge from a PCU would give patients the opportunity to organize their lives. Therefore, the probability of discharge from PCUs warrants further investigation. Discharge requires that symptoms such as dyspnea, nausea or pain are on the wane. On the other hand, “the going-home initiative” (24) can not be achieved by symptom control alone, but requires preparation of the home environment as well. Discharge is a difficult, sensitive and complex issue (25). There appears to be a “common pathway toward death” for malignant and nonmalignant diseases, as found by Solano et al., who investigated characteristic symptoms among end-stage patients with cancer, acquired immunodeficiency syndrome (AIDS), heart disease, chronic obstructive pulmonary disease, or renal disease. Pain, breathlessness, and fatigue were registered in more than 50% of patients for all five diseases (26). In the best interest of patients it would be meaningful to take their wishes into account. Therefore, it would be helpful to draft a realistic plan of achievable goals between the palliative care team, the patients, and their families.
The limitations of the present study include the small sample size and the heterogeneous nature of the patient population. At this point we have to refer to our exclusion criteria. Patients who did not give their consent or who were not able to communicate appropriately were excluded from the study. All of the patients that fulfilled the inclusion criteria agreed to participate. Due to the study design and the fact that almost all patients were admitted to the PCU for the first time, we were unable to compare the obtained HRV parameters with earlier measurements of HRV. We recommend further studies to investigate the association between reduced HRV parameters and a lower likelihood of discharge. KPS and the PPS are established tools (27,28) and did provide important information in the present study. The data indicate that KPS and PPS are reliable, simple, easy to assess, and of significant importance in palliative care. As time-consuming assessment is not always possible in clinical routine, KPS and PPS might serve as important guides for discharge. Furthermore, discharge management should receive the clinician’s attention at the very beginning of a patient’s in-hospital stay.
Supplementary material
Supplement 1: Components of HRV
HF: High frequency is a band of power spectrum ranging from 0.15 to 0.4 Hz, and reflects parasympathetic (vagal) activity. It is calculated in milliseconds squared (ms²), and is also known as the ‘respiratory band’ because of variations due to respiration. Heart rate increases during inhalation and decreases during exhalation, which is known as respiratory sinus arrhythmia.
LF: Low frequency is a band of power spectrum ranging from 0.04 to 0.15 Hz. It reflects both sympathetic and parasympathetic (vagal) activity, and is calculated in milliseconds squared (ms²). Generally it is a strong indicator of sympathetic activity. When the respiratory rate is lower than 7, parasympathetic influence is represented by LF. LF values may be high in a relaxed state, indicating parasympathetic activity.
TP: Total power is the subsumption of measurements between 0.003-0.4 Hz, and serves as a benchmark of total variability. It is calculated in milliseconds squared (ms²) and reflects overall autonomic activity, where sympathetic activity is a primary contributor.
PNN50: Measure of the percentage of successive RR intervals which differ from one another by more than 50 ms; higher parasympathetic (vagal) activity results in higher pNN50 values.
LOG LF/HF: Ratio between the power of low-frequency and high-frequency bands. It indicates overall balance between sympathetic and parasympathetic (vagal) activity. Higher values reflect domination of the sympathetic system, lower levels reflect domination of the parasympathetic system. LOG LF/HF indicates overall balance between the sympathetic and parasympathetic system and can be used to quantify the overall balance between the sympathetic and parasympathetic system.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Alonso-Babarro A, Bruera E, Varela-Cerdeira M, et al. Can this patient be discharged home? Factors associated with at-home death among patients with cancer. J Clin Oncol 2011;29:1159-67. [PubMed]
- Glare P, Sinclair C, Downing M, et al. Predicting survival in patients with advanced disease. Eur J Cancer 2008;44:1146-56. [PubMed]
- Narducci F, Grande R, Mentuccia L, et al. Symptom improvement as prognostic factor for survival in cancer patients undergoing palliative care: a pilot study. Support Care Cancer 2012;20:1221-6. [PubMed]
- Luengo-Fernandez R, Leal J, Gray A, et al. Economic burden of cancer across the European Union: a population-based cost analysis. Lancet Oncol 2013;14:1165-74. [PubMed]
- Wentlandt K, Krzyzanowska MK, Swami N, et al. Referral practices of oncologists to specialized palliative care. J Clin Oncol 2012;30:4380-6. [PubMed]
- Fainsinger RL, Demoissac D, Cole J, et al. Home versus hospice inpatient care: discharge characteristics of palliative care patients in an acute care hospital. J Palliat Care 2000;16:29-34. [PubMed]
- Bruera E, Chadwick S, Fox R, et al. Study of cardiovascular autonomic insufficiency in advanced cancer patients. Cancer Treat Rep 1986;70:1383-7. [PubMed]
- Fadul N, Strasser F, Palmer JL, et al. The association between autonomic dysfunction and survival in male patients with advanced cancer: a preliminary report. J Pain Symptom Manage 2010;39:283-90. [PubMed]
- Walsh D, Nelson KA. Autonomic nervous system dysfunction in advanced cancer. Support Care Cancer 2002;10:523-8. [PubMed]
- Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation 1996;93:1043-65. [PubMed]
- Tracey KJ. The inflammatory reflex. Nature 2002;420:853-9. [PubMed]
- Koenig J, Jarczok MN, Ellis RJ, et al. Heart rate variability and experimentally induced pain in healthy adults: A systematic review. Eur J Pain 2013. [Epub ahead of print]. [PubMed]
- Fairchild A, Debenham B, Danielson B, et al. Comparative multidisciplinary prediction of survival in patients with advanced cancer. Support Care Cancer 2014;22:611-7. [PubMed]
- Schag CC, Heinrich RL, Ganz PA. Karnofsky performance status revisited: reliability, validity, and guidelines. J Clin Oncol 1984;2:187-93. [PubMed]
- Anderson F, Downing GM, Hill J, et al. Palliative performance scale (PPS): a new tool. J Palliat Care 1996;12:5-11. [PubMed]
- Morita T, Tsunoda J, Inoue S, et al. Validity of the palliative performance scale from a survival perspective. J Pain Symptom Manage 1999;18:2-3. [PubMed]
- Virik K, Glare P. Validation of the palliative performance scale for inpatients admitted to a palliative care unit in Sydney, Australia. J Pain Symptom Manage 2002;23:455-7. [PubMed]
- Sasahara T, Watakabe A, Aruga E, et al. Assessment of reasons for referral and activities of hospital palliative care teams using a standard format: a multicenter 1000 case description. J Pain Symptom Manage 2014;47:579-587.e6.
- Bigger JT Jr, Kleiger RE, Fleiss JL, et al. Components of heart rate variability measured during healing of acute myocardial infarction. Am J Cardiol 1988;61:208-15. [PubMed]
- Tsuji H, Venditti FJ Jr, Manders ES, et al. Determinants of heart rate variability J Am Coll Cardiol 1996;28:1539-46. [PubMed]
- La Rovere MT, Bigger JT Jr, Marcus FI, et al. Baroreflex sensitivity and heart-rate variability in prediction of total cardiac mortality after myocardial infarction. ATRAMI (Autonomic Tone and Reflexes After Myocardial Infarction) Investigators. Lancet 1998;351:478-84. [PubMed]
- Casolo GC, Stroder P, Signorini C, et al. Heart rate variability during the acute phase of myocardial infarction. Circulation 1992;85:2073-9. [PubMed]
- Schroeder EB, Liao D, Chambless LE, et al. Hypertension, blood pressure, and heart rate variability: the Atherosclerosis Risk in Communities (ARIC) study. Hypertension 2003;42:1106-11. [PubMed]
- Lusardi P, Jodka P, Stambovsky M, et al. The going home initiative: getting critical care patients home with hospice. Crit Care Nurse 2011;31:46-57. [PubMed]
- Kd Vries, Wells J, Plaskota M. Evaluation of an admission and discharge programme at a UK specialist palliative day hospice. Int J Palliat Nurs 2012;18:275-81. [PubMed]
- Solano JP, Gomes B, Higginson IJ. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage 2006;31:58-69. [PubMed]
- Kutner JS, Meyer SA, Beaty BL, et al. Outcomes and characteristics of patients discharged alive from hospice. J Am Geriatr Soc 2004;52:1337-42. [PubMed]
- Harrold J, Rickerson E, Carroll JT, et al. Is the palliative performance scale a useful predictor of mortality in a heterogeneous hospice population? J Palliat Med 2005;8:503-9. [PubMed]


