The impact of the COVID-19 pandemic on lung cancer patients
Introduction
The current outbreak of SARS-CoV-2 (COVID-19) is one of the greatest public health crises facing our society, resulting in more than 770,000 deaths worldwide and incalculable economic damage. As the epidemic situation worsened, the World Health Organization declared on March 12, 2020, that COVID-19 is a global pandemic. With much remaining unknown about the novel virus and no effective treatment available, the outbreak continues to wreak havoc across the globe, indefinitely disrupting the lives of billions of people. Guan et al., reported 1,099 COVID-19 hospitalized patients between December 2019 and January 2020 in China, and found that patients with comorbidities were more susceptible to manifest complications of COVID-19 infection. Severe cases were more likely to have a malignancy (50.0%) than non-severe cases (15.6%) (1). In fact, multiple clinically relevant prognostic variables associated with increased 30-day all-cause mortality of COVID-19 were identified, including increasing age, male gender, smoking status (former smoker), cancer status, Eastern Cooperative Oncology Group (ECOG) performance status (≥2), and treatment with hydroxychloroquine plus azithromycin (2). Retrospective analysis confirmed that the risk of new coronavirus infection in cancer patients in the outbreak city was 2.31 times that of the general population. Additionally, compared with the general population, people with tumors or other complications suffered worse prognosis after infection with COVID-19 (3).
Lung cancer (LC) patients represent a central challenge in clinical diagnosis and treatment decision-making in the context of the highly contagious COVID-19 pandemic. Chemotherapy (CT), radiation therapy (RT), surgery, and molecular targeted therapy are keystones in the treatment of early and locally advanced LC with good prognosis. Chemotherapy plus targeted therapy or immunotherapy has also brought substantial survival benefit to recurrent/metastatic (R/M) advanced LC patients. However, frequent visits to hospital during the COVID-19 epidemic and receiving anticancer treatments with immunosuppressive properties might considerably increase the risk of being infected. Therefore, balancing the benefit from in-hospital anti-cancer treatments and the risk of infection may be crucial to the care of LC patients. Even for cancer patients who are non-COVID-19, the disruption of regular hospital service, such as imaging and treatment appointments, can have a significant impact on the physical and mental well-being of these patients. Indeed, our previous survey of 74 hospitals in China indicated that the regular treatment and follow-up of cancer patients during the new epidemic period had been affected (4). The impact of the stress placed on the availability of medical resources and hospitals have reduced the clinical admissions to most other departments, including oncology departments. Consequently, the benefits some cancer patients could have received have been compromised due to treatment delay.
Many clinical guidelines for COVID-19 prevention and management have recently been published, and provide guidance for the standard anticancer treatments to cancer patients with COVID-19. However, little research has been conducted to determine the proper recommendations for cancer patients with COVID-19 who are eligible to receive timely anticancer treatments. One of the few available resources is a patient-friendly brochure issued by the Cancer Council of Australia to familiarize cancer patients with all of the necessary information regarding COVID-19 and the approved measures of prevention (5). In addition, a clinical guideline was issued by the National Institute for Health and Care Excellence (NICE) (6) for guidance of standard anticancer treatments to cancer patients with COVID-19. It provides several recommendations based on the recently evidence regarding many COVID-19-related and cancer-related issues, to maximize the use of the available resources in order to sustain health services to cancer patients until more detailed guidelines are available.
As a COVID-19-designated hospital fighting the epidemic, the diagnosis and treatment of lung cancer patients in our cancer center have been significantly challenged of late. Thus, we initiated a retrospectively study to analyses the impact of COVID-19 on lung cancer patients. In this case series, we describe the clinical characteristics and outcomes of lung cancer patients, who accepted routine anticancer treatment before the epidemic and planned to return to hospital in January and February of 2020. We also discussed the strategies employed to sustain high-quality health services to cancer patients, including hospitalization, follow-up, and health education for after hospital discharge. We present the following article in accordance with the MDAR reporting checklist (available at http://dx.doi.org/10.21037/apm-20-1662).
Methods
From December 1, 2019 to January 15, 2020, lung cancer in patients who received routine anticancer treatment at the Fifth Affiliated Hospital of Sun Yat-sen University and planned to return to hospital during the epidemic in late January and February 2020, were included. The Fifth Affiliated Hospital of Sun Yat-sen University is a 1,650-bed public hospital serving approximately 1,900,000 residents in Zhuhai, China. It is the only designated hospital for receiving and curing COVID-19 patients in Zhuhai.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Prior to data collection, the protocol was approved by the ethics committee of the Fifth Affiliated Hospital of Sun Yat-sen University (No. K196-1). This retrospective study only collected the clinical data of patients, and did not interfere with the treatment plan of patients or bring risks to patients’ physiology, and the requirement for informed consent was waived. De-identified patient data were collected and analyzed using Neusoft Hospital Information System (eHIS). Chest radiographs (computed tomography) were reviewed by an oncologist and a radiologist. Patient outcome data were evaluated by at least two oncologists according to the response evaluation criteria in solid tumor (RECIST 1.1). Admission delayed was defined as delayed more than 21 days later than scheduled. No analysis for statistical significance was performed given the descriptive nature of the study.
Results
A total of 161 cases of lung cancer in our center were included. The clinical characteristics of cases are shown in Table 1. The median age was 57.58 years (range, 25–80 years), and 58.38% of cases were male. The most common histology was non-small cell lung cancer (n=147, 91.3%), the most frequent cancer stage was stage IV (n=109, 67.7%), and 40.99% patients had tumor-associated genetic mutations. All patients accepted regular antitumor treatment, including chemotherapy (n=109, 67.7%), radiotherapy (n=4, 2.48%), molecular targeted therapy (n=47, 29.19%), and/or immunotherapy (n=21, 13.04%).
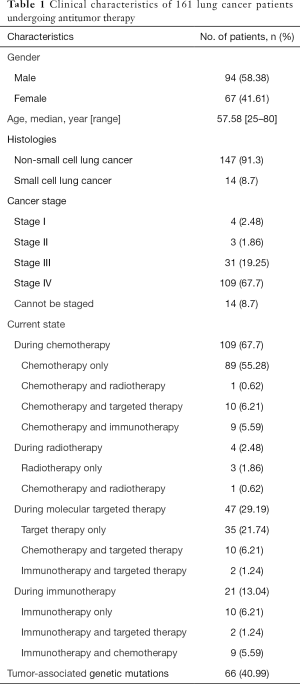
Full table
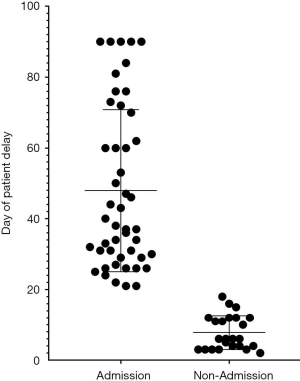
As of April 15, 95 patients had delayed their return visit, and 47 cases were finally designated to have had delayed admission during the epidemic and to have discontinued or delayed their regular anticancer treatments. Of these 47 cases, 33 had tumor status evaluated using computed tomography, 6 of whom (18.18%) had progressive disease (PD), and 5 of whom never returned for visit (Figure 1).
Discussion
In our study, a significant increase in admission delayed rate in our center (n=47/161, 29.19%) in lung cancer patients during the epidemic was detected compared to lung cancer patients before the epidemic (<5%). Of the 47 delayed cases, 33 were evaluated as tumor status, 6 (18.18%) of whom were identified as PD. for patients who continue to return to our center, we still continue to follow up, and the result will be reported in another article later. The strict screening and admittance criteria instilled by hospitals during the pandemic might have affected the treatment course. Furthermore, the epidemic might have also incurred a decrease in income and family and social support, traffic inconvenience, and other negative impacts. Most lung patients were present for regular anticancer treatments, especially chemotherapy (67.7%), molecular targeted therapy (29.19%), and immunotherapy (13.04%). Once the routine treatment process is interrupted, the tumor can progress and even threaten the life safety of cancer patients.
de Joode et al. investigated a study of 5,302 tumor patients during the COVID-19 pandemic in the Netherlands. Their research showed that the COVID-19 pandemic has had a significant impact on their oncological care. Similar to our study, the most frequently adjusted therapies were immunotherapy (32%) and chemotherapy (30%). Moreover, 30% of patients experienced consequences regarding their anticancer treatment or follow-up, mostly initiated by the hospital. Additionally, 50% of patients had contact with their hospital about their individual treatment, while 19% of patients were more reluctant to contact the doctor. Among patients with delayed admission and discontinued treatment, more than half of patients (55% and 63%) were very concerned about the consequences of the COVID-19 outbreak. Some patients might have also feared not to being allowed admittance into the intensive care unit if they were infected with COVID-19 (7).
Oncology physicians are very concerned about the impact of the COVID-19 pandemic on oncological care. Lian et al. investigated how to manage cancer patients with fever during radiotherapy. Their study showed that for cancer patients receiving radiotherapy, especially for lung cancer patients, old age and late disease staging, combined with cardiovascular or cerebrovascular diseases and combined with chemotherapy, leukocyte abnormality, and hypoalbuminemia as a cause of fever are more likely to happen during radiotherapy. In order to ensure the safety treatment for these patients and other patients without fever, rapid screening and other prevention and control measures were necessary (8). An expert’s guidance is essential to help patients get through the crisis. Oral medications may help to reduce dependence on intravenous for and hospital visits. Our work suggests that the continuation of in-hospital treatment with curative purposes under proper protection and a switch to oral therapy for chemotherapy/molecular targeted therapy LC patients were suitable in the quarantine period.
The serious epidemic was really much too sudden. At the time we couldn't have anticipated the dimensions of the epidemic. All the medical workers in the region made their best efforts to help to put down the epidemic. To reduce the deviation of retrospective research, we enrolled all the lung inpatients in our center from December 1, 2019 to January 15, 2020. To expanding the observation of the small sample size, maybe a further follow up for all cases contain both outpatients and inpatients could be analyzed.
In addition to this, psycho-oncological support is urgently needed for patients, especially for cancer patients with delayed admission. The cancer patients were more likely to associate physical discomfort with COVID-19 and were very sensitive to their physiological changes, especially worried about coughing, dyspnea, fatigue and other symptoms. Besides, the epidemic would also bring economic income falling, family and social support reduction, traffic inconvenience and other impacts. The rapid transmission of COVID-19, high fatality rates in subpopulations, lack of regularly anti-tumor treatments, and mass quarantine measures have affected the psychological status of cancer patients, even led to mental health problems. We initiated a prospective study to research the psychological changes of cancer patients during the COVID-19 epidemic. Before initiation of the trial, the protocol was approved by the ethics committee of the Fifth Affiliated Hospital of Sun Yat-sen University (approval No. 2020K18-1) and registered on chictr.org.cn (ChiCTR2000029830). Our results showed that the SAS scores and SDS scores of cancer patients were statistically different, compared those before the outbreak to those during the epidemic. The depression of cancer patients, especially of women patients, increased significantly during the epidemic period. The results were contributed in progress. Regrettably, for these 47 delayed patients, the changes of anxiety (SAS, GDA-7) and depression (SDS, PHQ-9) scores were fragmentary. It is necessary to help the patients to balance the various dynamics of life at hospital and home. Psychological counseling could be performed to associate emotions (anxiety, sadness, fear, anger) to their somatic reactions (headache, stomachache, difficulty relaxing, and sleeping). Convenient tools, such as mindfulness-based stress reduction techniques (MSRT), could be used to manage stress, pain perception, and reduce physical symptoms (9).
Conclusions
This is the first study to investigate the impact of COVID-19 on non-COVID-19 lung cancer patients during the pandemic. The study demonstrates the significant impact of the COVID-19 crisis on oncological care, indicating the need for appropriate change of treatment decisions and continued follow-up and psycho-oncological support during this pandemic.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the MDAR reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-1662
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-1662
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-1662). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Prior to data collection, the protocol was approved by the ethics committee of the Fifth Affiliated Hospital of Sun Yat-sen University (No. K196-1). This retrospective study only collected the clinical data of patients, and did not interfere with the treatment plan of patients or bring risks to patients’ physiology, and the requirement for informed consent was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Guan WJ, Ni ZY, Hu Y, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med 2020;382:1708-20. [Crossref] [PubMed]
- Kuderer NM, Choueiri TK, Shah DP, et al. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet 2020;395:1907-18. [Crossref] [PubMed]
- Liang W, Guan W, Chen R, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol 2020;21:335-7. [Crossref] [PubMed]
- Wei W, Jiang H, Chen W, et al. How should we implement radiotherapy for cancer patients in China during the endemic period of COVID-19? Radiother Oncol 2020;147:100-2. [Crossref] [PubMed]
- Cancer Council Australia. Information and support regarding cancer and COVID-19.Available online: https://www.cancer.org.au/support-and-services/cancer-and-covid-19, accessed March 27, 2020.
- National Institute for Health and Care Excellence. COVID-19 rapid guideline: delivery of systemic anticancer treatments. March 20, 2020. Available online: https://www.guidelines.co.uk/infection/covid-19-rapid-guideline-delivery-of-systemic-anticancer-treatments/455238.article, accessed March 26, 2020.
- de Joode K, Dumoulin DW, Engelen V, et al. Impact of the coronavirus disease 2019 pandemic on cancer treatment: the patients' perspective. Eur J Cancer 2020;136:132-9. [Crossref] [PubMed]
- Lian X, Shen J, Sun Y, et al. Under the coronavirus disease 2019 (COVID-19) pandemic circumstance, how to administrate cancer patients with fever during radiotherapy. Radiother Oncol 2020;150:15-7. [Crossref] [PubMed]
- Gregucci F, Caliandro M, Surgo A, et al. Cancer patients in Covid-19 era: Swimming against the tide. Radiother Oncol 2020;149:109-10. [Crossref] [PubMed]