Clinical value of N-acetylcysteine combined with terbutaline sulfate in elderly patients with chronic obstructive pulmonary disease and its effect on apoptosis/anti-apoptosis mechanism
Introduction
Chronic obstructive pulmonary disease (COPD) is a frequent clinical lung disease, and patients with typical clinical features of an incomplete reversible flow limitation. Affected by pulmonary hypertension, infection and other factors, the lung expiratory resistance increases in some patients, which can aggravate respiratory muscle fatigue and result in a large amount of functional residual air, making it difficult for respiratory muscle to maintain normal ventilation and increasing difficulty in treatment. COPD is a common disease with complex pathogenesis, which is mainly related to the imbalance of protease/anti-protease and oxidation/antioxidation, and inflammation of the lungs and respiratory system. At present, expectorant and antispasmodic measures are used clinically to intervene COPD in elderly patients, which can relieve clinical symptoms to a certain extent, but the effect of functional improvement still requires attention (1). Terbutaline sulfate and N-acetylcysteine (NAC) are commonly used in the treatment of COPD. Terbutaline sulfate is a kind of β2 receptor blocker that can effectively relieve spasm of the bronchial smooth muscle, expand bronchial tubes, and improve the gas exchange function of the lungs (2). The drug NAC is used to reduce phlegm by dissolving mucus, and has many effects such as anti-mutagenicity, promotion of pulmonary surfactant production, and anti-oxidation. Use of NAC is also important in alleviating inflammation of the respiratory system and improving lung function (3). In recent years, the function and mechanism of apoptosis/anti-apoptosis in COPD has received widespread attention, where the levels of soluble apoptosis factors Fas receptor/apoptosis antigen 1, soluble Fas (Fas/APO-1, sFas) are abnormally increased, which can cause abnormal apoptosis of inflammatory cells in the whole blood and lungs (4). Therefore, this study firstly combined terbutaline sulfate and NAC for the treatment of COPD in the elderly, and clarified their combined effect on lung function, levels of Fas/APO-1 and sFas. We present the following article in accordance with the CONSORT reporting checklist (available at http://dx.doi.org/10.21037/apm-20-1605).
Methods
General information
A total of 126 elderly COPD patients in our hospital from December 2017 to June 2019 were recruited. According to the differences of drugs on the basis of conventional treatment, they were divided into three groups: control group A (treated with NAC), control group B (treated with terbutaline sulfate) and combination group (treated with both drugs of NAC and terbutaline sulfate), with 42 cases in each group. This study was approved by the ethics committee of the Ningbo Yinzhou No. 2 Hospital.
The participant selection criteria were as follows: (I) patients met the COPD diagnostic criteria in the “Guideline for the management of chronic obstructive pulmonary disease” (5); (II) aged ≥60 years old; (III) mild to severe disease presentation; (IV) no immunosuppressive agents were taken within 3 months before the study; (V) patients were aware of this study and provided signed informed consent; (VI) patients willing to comply and effectively cooperate in the completion of the investigation and research.
Exclusion criteria were as follows: (I) comorbid organic diseases such as kidney and liver disorders; (II) comorbid bronchial tumor, tuberculosis, or asthma; (III) concurrent metabolic, endocrine, or blood system diseases; (IV) comorbid benign or malignant tumors; (V) allergic constitution or a history of allergy to drugs; (VI) glucocorticoids taken within 2 weeks before the study; (VII) short-acting bronchodilators had been stopped ≥24 h, or long-acting bronchodilators had been stopped ≥48 h; (VIII) history of tracheotomy and tracheal intubation.
An additional elimination criterion was made for patients who voluntarily withdrew during the course of study or experienced severe adverse reactions. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by ethics committee of our hospital, and informed consent was taken from all the patients.
Treatment methods
After admission, participants in all 3 groups were treated with anti-infection, antispasmodic, antibiotics, cough relieving, and other conventional therapies. In addition to conventional treatments, patients in the 3 groups were treated with different drugs. Patients in the control group A were treated with NAC (Hainan Zanbang, National Medicine Standard H20080326, China), 0.6 g taken orally 1–2/day; patients in the control group B were treated with terbutaline sulfate (AstraZeneca, National Medicine Standard H10930058, China), 5 mg by compressed nebulized inhalation, 15 mL for 2×/d; and patients in the combination group were treated with the combination of NAC and terbutaline sulfate, with the same dosage as control group A and B. The course of treatment for all 3 groups was 2 weeks.
Detection methods
A total of 5 mL of venous blood was extracted in a fasted state and centrifuged to obtain the supernatant (3,000 r/min, 10 min). The indexes for apoptosis/anti-apoptosis were then determined by enzyme-linked immunosorbent assay (ELISA) using the Bio-RAD 550 microplate reader and supporting kits (Bio-RAD, Hercules, CA, USA), including the levels of apoptosis-related indicators (Fas/APO-1, sFas), oxidative stress indicators [malondialdehyde (MDA), reactive oxygen species (ROS), superoxide dismutase (SOD), and glutathione peroxide enzyme (GSH-PX)].
Observation indicators
Lung function indexes were detected including forced vital capacity (FVC), peak expiratory flow (PEF), and mean maximal flow (MMF) before and 2 weeks after the drug treatment in the 3 groups. The blood gas indexes [oxygenation index (OI), oxygen saturation (SaO2), partial pressure of carbon dioxide (PaCO2)] were counted before and 2 weeks after treatment in the 3 groups. Recording the 6-min walking distance (6MWD) and CAT score before and 2 weeks after treatment in three groups. The COPD assessment test (CAT) included 10 items such as cough, sputum, restriction of daily life, chest tightness, and dyspnea. Each item had a total score of 5 points, giving a total overall CAT score of 50 points, and the lower the score, the better the treatment efficacy (6). The apoptosis/anti-apoptosis related indexes (Fas/APO-1, sFas) were analyzed before and 2 weeks after treatment in the 3 groups. The levels of oxidative stress indicators (MDA, ROS, SOD, GSH-PX) were analyzed before and 2 weeks after treatment in the 3 groups. Finally, any adverse reactions in the 3 groups were recorded.
Statistical methods
Data were analyzed using the SPSS 22.0 (SPSS Inc., IBM Company, Chicago, IL, USA). The measurement data were expressed as (
Results
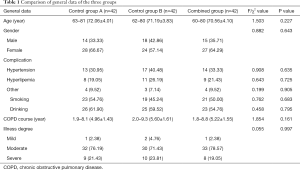
General clinical data of the three groups
There was no significant difference in the clinical data regarding gender, age, complicating diseases, smoking and drinking status, course of COPD, and degree of illness between the 3 groups (7) (P>0.05, Table 1), and the 3 groups were balanced and comparable.
Full table
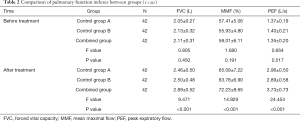
Comparison of lung function of the three groups
There was no significant difference in FVC, MMF, and PEF levels among the 3 groups before treatment (P>0.05). After treatment, the levels of FVC, MMF, and PEF in the 3 groups were higher than they were before treatment; the levels of the combination group were significantly higher than those of the other 2 groups (both P<0.05, Table 2).
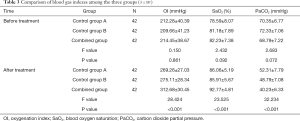
Comparison of blood gas indexes of the three groups
There was no significant difference in OI, SaO2, and PaCO2 levels among the 3 groups before treatment (P>0.05). After treatment, OI and SaO2 levels in the 3 groups were higher than those before treatment, while the PaCO2 level was lower than before treatment. After treatment, OI and SaO2 in the combined group were higher than those in the control groups A and B, and the PaCO2 level was significantly lower than that of the other 2 groups (P<0.05, Table 3).
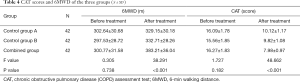
Comparison of CAT score and 6MWD of the three groups
There was no significant difference in 6MWD and CAT score among the 3 groups before treatment (P>0.05). After treatment, the 6MWD of the 3 groups had increased, and the CAT score was lower than it was prior to treatment. The 6MWD of the combination group had increased more than that of the control groups A and B, while the CAT score was more significantly reduced than in the other 2 groups (P<0.05, Table 4).
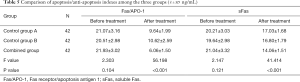
Comparison of apoptosis and anti-apoptosis indicators of the three groups
Before treatment, there was no significant difference in the Fas/APO-1 and sFas levels among the groups (P>0.05). After treatment, the Fas/APO-1 and sFas levels in the 3 groups were lower than those before treatment, and the levels in the combined group were significantly lower than in the control groups A and B (P<0.05, Table 5).
Full table
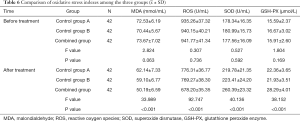
Comparison of oxidative stress indicators of the three groups
Before treatment, there was no significant difference in serum MDA, ROS, SOD, and GSH-PX levels among the 3 groups (P>0.05). Following treatment, the levels of MDA and ROS in the 3 groups were lower than those before treatment, while SOD and GSH-PX levels were higher than those before treatment. After treatment, the levels of MDA and ROS in the combined group were lower than those of control groups A and B, and the levels of SOD and GSH-PX in the combined group were significantly higher than those of the other 2 groups (P<0.05, Table 6).
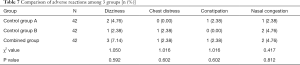
Comparison of adverse reactions of the three groups
There was no significant difference in the incidence of adverse reactions among all 3 groups: combination group, control group A, and control group B (P>0.05, Table 7).
Full table
Discussion
There is a high incidence of COPD amongst elderly patients. During the pathogenesis of this disease, inflammatory cells in the central airway infiltrate the surface epithelium, and the subsequent increase of goblet cells and enlargement of mucus secretion glands leads to an increased secretion of mucus. Due to the weakened cough reflex, the respiratory tract mucosa shrinks, cilia motility is poor, and the power of expectoration is weakened. Thus the secretions easily accumulate in the bronchus and airway, which increases the difficulty of diagnosing and treating COPD (8).
Traditionally, expectorants and oxygen inhalation are administered in the treatment of COPD, but the overall effect still requires a large degree of improvement. In order to further improve the treatment efficacy and comprehensively intervene, it is necessary to combine other drugs instead of relying on solitary drug performance. Terbutaline sulfate is an important therapeutic drug for COPD, which can act on the respiratory tract at a higher concentration after compressed nebulization and inhalation, activating adenosine cyclase and increasing the content of cyclic adenosine and ribonucleic acid in cells. As a kind of short-acting β2 receptor agonist, terbutaline sulfate can also excite β2 receptors to relax the smooth muscle of the respiratory tract, inhibit the production of inflammatory mediators, expand airways, enhance cilia movement, promote sputum discharge, and finally improve the ventilation function of the lung (9). Concurrently, terbutaline sulfate can stimulate alveolar type II cells to synthesize and secrete pulmonary surfactant, which can reduce the viscosity of mucopolysaccharides, and promote sputum secretion (10). Additionally, terbutaline sulfate can reduce the adhesion of bacteria to airway epithelial cells, thereby reducing the incidence of acute episodes of COPD. It has been reported that after treatment with terbutaline sulfate on the basis of conventional intervention, the lung function of patients with an acute exacerbation of COPD can be significantly improved (11). The drug NAC is also commonly used in the treatment of COPD. It is a natural derivative of L-arginine with active groups that can block mucin disulfide bonds, decompose mucin, dilute sputum, and enhance the physiological transport function of the mucus cilia system (12). By inhibiting the neutrophils to infiltrate into the lungs, NAC can remove ROS. It can also decompose hydrogen peroxide by combining with GSH-PX, thereby reducing lipid peroxidation, and the inflammatory stress response. Another study pointed out that NAC could effectively reverse the decrease in SOD and GSH activity caused by smoking, thus it is useful as an antioxidant to promote the balance of the oxidation-antioxidant system, thereby reducing the oxidative damage of the lungs (13,14).
In this study, we were the first to combine NAC and terbutaline sulfate to implement comprehensive treatment for COPD patients in our hospital. The results showed the improvement of lung function and blood gas indexes in the combined group to be more significant than those of control groups A and B. The combined group scores of 6MWD and CAT were higher than those of control groups A and B, and SOD and GSH-PX levels were higher than in control groups A and B, while MDA and ROS levels were lower than those in the control groups A and B. Among these indexes, MDA, ROS, SOD, and GSH-PX are commonly used for clinical evaluation of the stress response, so the above results indicated that the combination of NAC and terbutaline sulfate was more effective in relieving the oxidative stress response, and improving blood gas state and lung function in elderly COPD patients. These therapeutic actions enable the recovery of the patients’ exercise capacity to be promoted. The results of this study can be explained by these 4 reasons: (I) terbutaline sulfate promotes the conversion of adenosine triphosphate (ATP1) to cyclic adenosine monophosphate (cAMP), which can expand the bronchus, and relieve airway spasm. The nebulizer method can increase the local drug concentration to lengthen the drug effect, which can effectively initiate the physiological activity of adenylyl cyclase in bronchial mucosal cells; (II) the nebulized inhalation of terbutaline sulfate can enhance the scavenging ability of bronchial cilia, reduce vascular permeability, and inhibit the generation of inflammatory mediators by mast cells, thereby improving the pulmonary function and hemodynamic status, and reversing hypoxemia; (III) the activation of inflammatory cytokines such as tumor necrosis factor-α (TNF-α) and nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κβ) can be prevented by NAC, which in turn blocks macrophages and epithelial cells from secreting inflammatory factors, and prevents the accumulation of excess neutrophils in the lung; (IV) anti-proteases can be activated by NAC, and this can prevent polymorphonuclear leukocytes from producing elastase and causing alveolar elastase, which can improve the ventilation function of the lungs, protect alveolar elasticity, prevent α1-antitrypsin from being inactivated by hydrogen peroxide, and reduce the expression of TGF-β1. Finally, NAC plays an important role in inhibiting airway remodeling and restoring lung function.
In addition, our current research included a comparative study on the changes of apoptotic cytokines before and after treatment on the basis of previous studies. The results showed that after treatment, the Fas/APO-1 and sFas levels of the combined group were significantly lower than those of control groups A and B. As a transmembrane glycoprotein of the TNF family, Fas can bind to the corresponding antibody and natural ligand (FasL) in the form of a trimer, which can aggravate cell apoptosis. Studies have shown that the abnormal apoptosis pathway mediated by Fas/APO-1 causes abnormal apoptosis of T lymphocytes, macrophages, neutrophils, and other inflammatory cells in COPD patients, and accelerates the progress of COPD (15). At the same time, the high expression of sFas can inhibit the apoptosis of neutrophils, and promote their accumulation in the lung tissues and blood vessels to produce more free radicals, interleukin 8 (IL-8), and TNF-α. The increase of inflammatory factors encourages further inflammatory infiltration of the lungs, and triggers the production of multiple proteases, which directly damage the lung parenchymal cells. Meanwhile, elastases such as matrilysin (MMP-7) can also be regulated by sFas to cause macrophages to lose the ability of smoothly distinguishing and engulfing neutrophils, which allows neutrophils to persist in exacerbating inflammatory injury (16). Therefore, the above results indicated that NAC combined with terbutaline sulfate can diminish the inflammatory response, reduce inflammatory damage, and accelerate recovery of the lung function of COPD patients by regulating the apoptosis mechanism. The increased efficacy of the combination of NAC and terbutaline sulfate might be due to the 2 drugs inhibiting the production and expression of inflammatory factors through different and complementary mechanisms.
In summary, the combined treatment of terbutaline sulfate and NAC in elderly COPD patients can effectively improve lung function and blood gas status, and strengthen the body’s capacity for exercise by reducing oxidative stress and regulating apoptosis cytokines. However, there are still some limitations in this study, such as a small sample size. Therefore, it is still necessary to expand the scope of sample selection and increase the sample size to further explore and confirm whether the results have broad validity.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-1605
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-1605
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-1605). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by ethics committee of our hospital, and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sidhaye VK, Nishida K, Martinez FJ. Precision medicine in COPD: where are we and where do we need to go? Eur Respir Rev 2018;27:180022. [Crossref] [PubMed]
- Beltaief K, Msolli MA, Zorgati A, et al. Nebulized Terbutaline and Ipratropium Bromide Versus Terbutaline Alone in Acute Exacerbation of Chronic Obstructive Pulmonary Disease Requiring Noninvasive Ventilation: A Randomized Double-blind Controlled Trial. Acad Emerg Med 2019;26:434-42. [Crossref] [PubMed]
- Hirai DM, Jones JH, Zelt JT, et al. Oral N-acetylcysteine and exercise tolerance in mild chronic obstructive pulmonary disease. J Appl Physiol 1985;2017:1351-61. [PubMed]
- Yasuda N, Gotoh K, Minatoguchi S, et al. An increase of soluble Fas, an inhibitor of apoptosis, associated with progression of COPD. Respir Med 1998;92:993-9. [Crossref] [PubMed]
- Abdool-Gaffar MS, Ambaram A, Ainslie GM, et al. Guideline for the management of chronic obstructive pulmonary disease--2011 update S Afr Med J 2011;101:63-73. [published correction appears in S Afr Med J. 2011 May;101(5):288]. [PubMed]
- Karloh M, Fleig Mayer A, Maurici R, et al. The COPD a Assessment Test: What do we know so far? A systematic review and meta-analysis about clinical outcomes prediction and classification of patients into GOLD stages. Chest 2016;149:413-25. [Crossref] [PubMed]
- Yoon HK, Park YB, Rhee CK, et al. Committee of the Korean COPD Guideline 2014. Summary of the Chronic Obstructive Pulmonary Disease Clinical Practice Guideline Revised in 2014 by the Korean Academy of Tuberculosis and Respiratory Disease. Tuberc Respir Dis (Seoul) 2017;80:230-40. [Crossref] [PubMed]
- Onk D, Özçelik F, Onk OA, et al. Assessment of renal and hepatic tissue-protective effects of N-Acetylcysteine via ammonia metabolism: A prospective randomized study. Med Sci Monit 2018;24:1540-6. [Crossref] [PubMed]
- Beng H, Zhang H, Jayachandra R, et al. Enantioselective resolution of Rac-terbutaline and evaluation of optically pure R-terbutaline hydrochloride as an efficient anti-asthmatic drug. Chirality 2018;30:759-68. [Crossref] [PubMed]
- Xiong G, Xu L, Wei L, et al. Atomization inhalation of terbutaline and budesonide efficiently improved immunity and lung function of AECOPD patients. Cell Mol Immunol 2008;5:287-91. [Crossref] [PubMed]
- Morandini R, Ghanem G, Portier-Lemarié A, et al. Action of cAMP on expression and release of adhesion molecules in human endothelial cells. Am J Physiol 1996;270:H807-16. [PubMed]
- Yang B, Choi H, Lim JH, et al. The disease burden of bronchiectasis in comparison with chronic obstructive pulmonary disease: a national database study in Korea. Ann Transl Med 2019;7:770. [Crossref] [PubMed]
- Ansari SF, Memon M, Brohi N, et al. N-acetylcysteine in the management of Acute exacerbation of chronic obstructive pulmonary disease. Cureus 2019;11:e6073. [PubMed]
- Sudheer AR, Muthukumaran S, Kalpana C, et al. Protective effect of ferulic acid on nicotine-induced DNA damage and cellular changes in cultured rat peripheral blood lymphocytes: a comparison with N-acetylcysteine. Toxicol In Vitro 2007;21:576-85. [Crossref] [PubMed]
- Takabatake N, Nakamura H, Inoue S, et al. Circulating levels of soluble Fas ligand and soluble Fas in patients with chronic obstructive pulmonary disease. Respir Med 2000;94:1215-20. [Crossref] [PubMed]
- Paunel-Görgülü A, Flohé S, Scholz M, et al. Increased serum soluble Fas after major trauma is associated with delayed neutrophil apoptosis and development of sepsis. Crit Care 2011;15:R20. [Crossref] [PubMed]
(English Language Editor: J. Jones)