
A clinical study on the ability of the integrative weaning index to predict weaning from mechanical ventilation
Introduction
Mechanical ventilation (MV) is commonly used in the intensive care unit (ICU). Aside from its lifesaving role, lung injury caused by MV has also been emphasized. Weaning from the mechanical ventilator is one such critical issue that affects ICU patient outcomes. There are many reasons for the failure of weaning clinically, such as: uncontrolled primary disease, fluid overload, heart failure, respiratory muscle weakness, etc. The prolongation of weaning time is positively correlated with the poor prognosis of patients, resulting in ventilator-associated complications like pneumonia, upper gastrointestinal bleeding, bacteremia, barotrauma, etc. Early weaning and extubation may save medical resources as well as reduce the incidence of related complications and improve the prognosis of patients (1-3). However, obtaining an optimal weaning decision, depending on the patient complexity, the number of parameters, and the demand for expert’s clinical experiences, has always been a substantial challenge for clinicians. As a comprehensive indicator, integrative weaning index (IWI) includes Static compliance of the respiratory system (Cst, Rs), arterial oxygen saturation (SaO2), and rapid shallow breathing index (RSBI). Multi-angle evaluation of mechanically ventilated patients may increase the success rate of weaning.
Weaning process
The weaning process can be divided into two steps: planned ventilator assisted breathing and removal of the tracheal tube. The first step commonly takes up 40–50% of the total MV time. According to the age, primary disease, physical condition, etc. of the patient, the patient-specific weaning can be separated into simple weaning, difficulty weaning, and even inability to wean. Shorting the weaning time has always been a problematic topic in MV, especially for patients with MV time greater than 72 hours (4).
Clinical parameters
Various clinical parameters are used to predict weaning from MV and extubation outcomes. Among the most used in practice are Rapid Shallow Breathing Index (RSBI), maximum inspiratory pressure (MIP), and independent parameter combinations. Derivative parameters, including the Integrative Index (CROP), etc. (5). We outline the role of these parameters in the weaning decision below.
Proposed by Yang (6) RSBI is considered the most exact parameter for predicting the success of weaning. Patients with RSBI less than 105 breaths/min/liter are highly likely to be successfully extubated (7). And its predictive power was confirmed in later studies (6,8). However, it is still controversial on the method to measure the RSBI value on different ventilation modes. In Europe, about 49% of private hospitals and 50% of public hospital respiratory therapists apply the continuous positive airway pressure (CPAP) method that measures the RSBI value (9). Monaco et al. believe the RSBI value measured by the CPAP method is of little clinical value for predicting the outcome 24 hours after weaning (10). The study in Patel et al. (11,12) proposed that the RSBI value measured by the CPAP method is lower than the RSBI value measured by the tidal volume meter. However, it does not affect the clinical value of RSBI prediction of weaning. Bien et al. applied the five methods, including CPAP and tidal volume meter, to measure the same group of patients and found there was no significant difference in the obtained RSBI value (13). Therefore, this study chose to use the tidal volume meter to calculate the first minute of the patient’s spontaneous breathing trial (SBT). The shallow fast breathing index, the research on the RSBI value obtained by different measurement methods, and its related derivative parameters on the significance of the weaning prediction should be further explored in future clinical work.
The dynamic change of RSBI is also an essential factor for its prediction ability. Different studies have been a focus on this point. Segal et al. measured the RSBI value at multiple time points of SBT for 2 hours and compared it with the traditional single measurement method. It was found the RSBI at 30 minutes after the start of SBT was easier to wean than the patient whose RSBI value increased by <5% at the first minute. Continuous measurement of RSBI values could be more exact than single-shot measurements for weaning predictions (14).
Conversely, Teixeria et al., which is like Segal’s application, concluded that the continuous observation of RSBI values is of little value in predicting the failure of the weaning (15). There are different opinions on the best threshold of RSBI. Sassoon and others believe RSBI ≤60 breath/min/liter period has the greatest predictive ability for weaning (16), and Armando J included 59 patients who were ready to wean and found that 30.5% of the cases failed offline with RSBI ≤105 breaths/min/liter, and the RSBI values of these patients were between 80 and 105 (17).
The tracheal airway occlusion pressure P0.1 reflects the patient’s respiratory center is the driving force. Its normal value is 0.5–1.5 cmH2O, and P0.1 >4.2 cmH2O often predicts the weaning failure. MIP reflects the patient’s respiratory muscle strength; healthy men and women have MIP values between −111±34 and −72±26 cmH2O. Patients with MIP value −20 to −30 cmH2O is expected to have a higher weaning successive rate. P0.1/MIP is also a high-power offline predictor of weaning outcome. In clinical practice, P0.1/MIP <0.14 is often used to predict the success or failure of the weaning. A recent comparison P0.1, MIP, P0.1/MIP three guiding significance weaning success, it considers P0.1 sensitivity/MIP over the earlier two high (18). P0.1 and MIP are easy to obtain clinically. In this study, statistical software was used to plot the working characteristic curves of each parameter, and the statistical difference of the area under the curve was compared. Compared with the above three, IWI can integrate the indicators commonly used in clinical practice to reflect the patient’s respiratory system to reflect the accuracy of its successful prediction of weaning.
Static respiratory compliance (Cst, Rs) roughly reflects the global elasticity of lung tissue. It refers to volume changes caused by the pressure changes. Cst obtains static respiratory compliance, Rs=Vt/Pplat-PEEP-PEEPi. Cst, Rs has been used as an indicator to guide the evacuation of ventilators in clinical use.
Integrative weaning index (IWI)
Nemer et al. (19) roposed a new index of the IWI, composing several parameters. IWI is a composite parameter of Cst, Rs, SaO2, and RSBI:
IWI = Cst, Rs × SaO2/RSBI
with unit mL/cmH2O breath/minute/liter. The change of concentration will affect the SaO2 value. In this study, MV patients with an oxygen concentration of 0.35 were included. Expanding the study on patients with a further range of oxygen concentration might be worthwhile to investigate the clinical significance of IWI. To help evacuate the patient’s MV. For patients in ICUs greater than 24 hours, studies have shown IWI predicts the ability to withdraw from the machine successfully is better than the above three independent parameters and other parameters like P0.1, RSBI × P0.1, PaO2/FiO2, VT, etc. (19). We present the following article in accordance with the STARD reporting checklist (available at http://dx.doi.org/10.21037/apm-20-1335).
Methods
Object
This is a prospective study. The inclusion criteria: (I) patients who required MV and MV for more than 72 hours; (II) all patients are above 18 years old and are suffering from respiratory failure due to distinct reasons.
These patients are admitted to the Department of Critical Care Medicine, the Fourth Hospital of Hebei Medical University. The exclusion criteria are (I) dyscrasia caused by advanced malignancy; (II) MV patients who have undergone tracheostomy; (III) patients with chronic obstructive pulmonary disease; (IV) patients with neuromuscular disease leading to spontaneous ventilation damage.
This study meets the requirements of medical ethics and has been approved by the Ethics Committee of the Fourth Hospital of Hebei Medical University (No. 2019150). All patients have signed informed consent from their immediate family members. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013).
Data collection
Patients were divided into two groups; those which unaccepted MV with FiO2 =40% and FiO2 =35% separately. There are 25 patients in each group. For each group, such a FiO2 setting was fixed for more than 30 min before the weaning, and the support pressure ≤8 cmH2O, the positive end expiratory pressure(PEEP) ≤5 cmH2O. Weaning was considered successful when the patient remained extubated without any ventilatory assistance for 24 hours. The outcome, recording the success or failure of the weaning, for each group was analyzed.
General conditions, vital signs, main causes of respiratory failure, acute physiology, and chronic health evaluation (APACHE II), as well as days under MV, are documented. MV related settings like expiratory tidal volume (VT), intrinsic positive end-expiratory pressure (PEEPi), SaO2, and other indicators of arterial blood gas analysis are recorded for each patient. Clinical parameters, including Cst, Rs, P0.1, MIP, P0.1/MIP, RSBI, and IWI, are calculated.
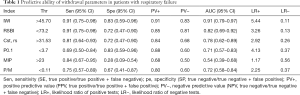
Statistical analysis
Statistical analysis was performed on general data using SPSS 13.0 software, and receiver operating characteristic curve (ROC) curve analysis was performed using Medcalc 11.4 statistical software. The data were obtained as a mean ± standard deviation (mean ± s), and the independent sample t-test was used to compare the data between the two groups. A chi-square test was used to compare the sample rates between the two groups. The prediction ability of the weaning prediction parameters is compared using the area under the curve (AUC). P<0.05 was considered statistically significant.
Results
General clinical data
Within a total of 50 patients with respiratory failure, which consists of 34 males and 16 females, 32 patients (64%) were successful in weaning, and 18 patients (36%) failed. The SaO2 value of the 0.40 group was higher than the 0.35 group SaO2 (96.73±1.65 vs. 95.47±2.23, P<0.05). Among the patients receiving MV with FiO2 =40%, 17 cases (68%) got successful weaning, and 8 cases (32%) failed. Within the 0.35 group, 15 patients (60%) with successful weaning, and ten patients (30%) with weaning failure. There was no difference in age, gender, APACHE II score, MV days, and weaning success rate between the two groups (P>0.05). Furthermore, there were no differences in IWI, RSBI, Cst, Rs, MIP, P0.1, P0.1/MIP between the two groups (P>0.05).
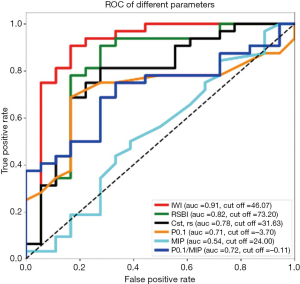
FiO2 40% group
IWI >50.40 is the cut-point value to predict the outcome of weaning. This cut-point is obtained by analyzing Youden’s index combined with the ROC curve (Figure 1). The sensitivity for predicting the success of the weaning was 0.82, and the specificity was 0.88. The AUC of the ROC of IWI was 0.846±0.117 (95% CI: 0.646–0.958) (Figure 1 and Table 1). There was a statistically significant difference compared with MIP (P<0.05). There is no significant difference (P>0.05) from RSBI, Cst, Rs, P0.1, P0.1/MIP, SaO2. There was a statistically significant difference in the mean values of IWI, RSBI, and P0.1 between the successful patients with weaning and those with failed weaning (P<0.05) (Figure 2). Successful weaning and weaning failure patients Cst, RS, the MIP, P0.1/MIP, SaO2 mean no significant difference (P>0.05) (Figure 2).
Full table
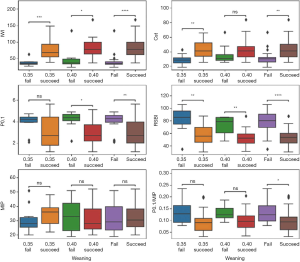
FiO2 35% group
IWI >39.33 (Table 1) is the best cut-point, the sensitivity of predicting the success of weaning was 93.33%, and the specificity was 0.90. The AUC ROC for IWI was 0.953±0.0394 (95% CI: 0.787–0.998) (Figure 1 and Table 1). There was a statistically significant difference between IWI and P0.1, MIP, P0.1/MIP, SaO2 (P<0.05). There is no statistically significant difference between IWI and RSBI, Cst, Rs (P>0.05). There was a statistically significant difference in the mean values of IWI, RSBI, Cst, Rs between the patients with successful weaning and those with failed weaning (P<0.05), while there was no statistical difference between P0.1, MIP and P0.1/MIP (P>0.05) (Figure 2).
All patients
IWI >45.70 (Table 1) is determined to be the cut-point for prediction, the sensitivity of predicting the success of weaning was 0.91, the specificity was 0.83, the positive predictive value was 0.91, and the negative predictive value was 0.88. The AUC of the ROC was 0.908±0.055 (Figure 1 and Table 1), which was significantly different from Cst, Rs, P0.1, MIP, P0.1/MIP, and SaO2 (P<0.05). However, there was no statistically significant difference (P>0.05) from the area under the curve of RSBI. The IWI, RSBI, Cst, Rs, P0.1, and SaO2 values of patients with successful weaning were significantly different (P<0.05), and there was no significant difference between MIP and P0.1/MIP (P>0.05).
Discussion
Analysis in this study indicated IWI has certain predictability according to the Swets (20) (0.5≤ AUC ≤0.7, lower predicted; 0.7≤ AUC ≤0.9, a certain predictive ability; AUC >0.9, high predictive ability). This parameter predicts the weaning outcome consistently well within FiO2 0.35 and FiO2 0.40 group, although with different cut points.
The ROC curve of the RSBI is 0.82 (Figure 1 and Table 1), which is consistent with those reported in earlier studies (between 0.77 and 0.89) (6,19,21,22). The RSBI threshold for this study was 73.2 (Table 1), also like that reported in a previous study (60 breaths/min/liter) (23).
The AUC of the ROC of P0.1 is 0.71 (Figure 1 and Table 1) [ranges from 0.47 to 0.93 in (18,24,25)]. In this study, P0.1 <3.7 cmH2O was used as the threshold for prediction. The sensitivity of the weaning was 0.69, the specificity was 0.83, the positive predictive value was 0.88, and the negative predictive value was 0.60. Among all the cases included in this trial, there was a statistically significant difference in the mean P0.1 between successful and failed weaning.
Although the MIP value is widely used, the accuracy of predicting the result of the weaning is not high. According to the AUC (0.54) of MIP (Figure 1 and Table 1) we conclude the predicted value is low [between 0.52 to 0.71 in previous studies (6,18,24)]. The recovery of individual respiratory muscle strength is not a criterion for successful weaning; that is, respiratory muscles may resist breathing during the respiratory cycle.
P0.1/MIP as a composite parameter of the two, Capdevila XJ, has reported it has a higher predictive value (25). However, more studies have shown the area under the curve predicting the success of the weaning is 0.71–0.78 (18,24). The predictive power of P0.1/MIP is controversial. The AUC of P0.1/MIP obtained in this study is 0.73 (Figure 1). When P0.1/MIP <0.11, the sensitivity of predicting the success of weaning is 0.72, and the specificity is 0.78 (Table 1). These results show its certain predictive power; however, the parameter P0.1/MIP has no significant difference between success or failure in weaning patients. The clinical value of this predictor needs to be discussed.
In this study, the prediction parameter Cst, Rs has a sensitivity of 0.81, a specificity of 0.72, a positive predictive value of 0.84, a negative predictive value of 0.68 (Table 1), and an area under the curve of 0.78 [like a previous study by Nemer (19), which shows its predictive power. However, within the group FiO2 =0.40, there is no significant difference between patients with different weaning outcomes.
The acquisition of clinical weaning parameters should be objective, easy to obtain, and does not interfere with the treatment of patients. The physiological mechanisms leading to respiratory failure are different. Different weaning parameters will focus on one aspect of the pathophysiological mechanism. At present, the evidence of using the weaning index alone to improve the prognosis of patients with MV is insufficient. Patients with adequate oxygenation and blood flow the three criteria of smooth dynamics and adequate spontaneous breathing ability can be applied to shorten the patient’s MV time, and the value of relying on a single parameter cannot be used as the golden rule for predicting the weaning (21). The evacuation of a ventilator is a complex dynamic process. Compared with individual predictive indicators, many objective indicators are jointly obtained. The parameters have certain advantages in guiding the weaning. In future research, the analysis over different parameters should be confirmed by large-scale clinical trials. Moreover, the patient’s long-term prognosis, like ICU stay, total hospital stay, and mortality, can be included for evaluation.
Conclusions
According to this retrospective study, the parameter IWI has a higher predictive ability over weaning outcomes than the other parameters. The 0.40 IWI predictive ability was lower than the 0.35 group. Before the SBT, setting the FiO2 to 0.35 for more than 30 min may have a better-guided significance for MV evacuation.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STARD reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-1335
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-1335
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-1335). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study meets the requirements of medical ethics and has been approved by the Ethics Committee of the Fourth Hospital of Hebei Medical University (No.: 2019150). All patients have signed informed consent from their immediate family members. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Eskandar N, Apostolakos MJ. Weaning from Mechanical Ventilation. Critical Care Clinics 2007;23:263-74. [Crossref] [PubMed]
- Navalesi P, Bruni A, Garofalo E, et al. Weaning off mechanical ventilation: much less an art, but not yet a science. Ann Transl Med 2019;7:S353. [Crossref] [PubMed]
- Schweickert WD, Gehlbach BK, Pohlman AS, et al. Daily interruption of sedative infusions and complications of critical illness in mechanically ventilated patients. Crit Care Med 2004;32:1272-6. [Crossref] [PubMed]
- Burns SM. Weaning from Mechanical Ventilation Where Were We Then, and Where Are We Now? Crit Care Nurs Clin North Am 2012;24:457-68. [Crossref] [PubMed]
- Vallverdú I, Calaf N, Subirana M, et al. Clinical Characteristics, Respiratory Functional Parameters, and Outcome of a Two-Hour T-Piece Trial in Patients Weaning from Mechanical Ventilation. Am J Respir Crit Care Med 1998;158:1855-62. [Crossref] [PubMed]
- Yang KL, Tobin MJ. A Prospective Study of Indexes Predicting the Outcome of Trials of Weaning from Mechanical Ventilation. N Engl J Med 1991;324:1445-50. [Crossref] [PubMed]
- McConville JF, Kress JP. Weaning patients from the ventilator. N Engl J Med 2012;367:2233-9. [Crossref] [PubMed]
- Tobin MJ, Jubran A. Meta-analysis under the spotlight: Focused on a meta-analysis of ventilator weaning. Crit Care Med 2008;36:1-7. [Crossref] [PubMed]
- Mont'Alverne DGB, Lino JA, Bizerril DO. Variations in the measurement of weaning parameters of mechanical ventilation in Fortaleza hospitals. Revista Brasileira De Terapia Intensiva 2008;20:149-53. [PubMed]
- Monaco F, Drummond GB, Ramsay P, et al. Do simple ventilation and gas exchange measurements predict early successful weaning from respiratory support in unselected general intensive care patients? Br J Anaesth 2010;105:326-33. [Crossref] [PubMed]
- Patel KN, Ganatra KD, Bates JHT, et al. Variation in the rapid shallow breathing index associated with common measurement techniques and conditions. Respir Care 2009;54:1462-6. [PubMed]
- El-Khatib MF, Zeineldine SM, Jamaleddine GW. Effect of pressure support ventilation and positive end expiratory pressure on the rapid shallow breathing index in intensive care unit patients. Intensive Care Med 2008;34:505-10. [Crossref] [PubMed]
- Bien MY, Lin YS, Shie HG, et al. Rapid Shallow Breathing Index and Its Predictive Accuracy Measured under Five Different Ventilatory Strategies in the Same Patient Group. Chinese Journal of Physiology 2010;53:1-10. [Crossref] [PubMed]
- Segal LN, Oei E, Oppenheimer BW, et al. Evolution of pattern of breathing during a spontaneous breathing trial predicts successful extubation. Intensive Care Med 2010;36:487-95. [Crossref] [PubMed]
- Teixeira C, Zimermann Teixeira PJ, Hohër JA, et al. Serial measurements of f/VT can predict extubation failure in patients with f/VT < or = 105? J Crit Care 2008;23:572-6. [Crossref] [PubMed]
- Sassoon CS, Mahutte CK. Airway Occlusion Pressure and Breathing Pattern as Predictors of Weaning Outcome. Am Rev Respir Dis 1993;148:860-6. [Crossref] [PubMed]
- Huaringa AJ, Wang A, Haro MH, et al. The Weaning Index as Predictor of Weaning Success. J Intensive Care Med 2013;28:369-74. [Crossref] [PubMed]
- Evaluation of maximal inspiratory pressure, tracheal airway occlusion pressure, and its ratio in the weaning outcome. J Crit Care 2009;24:441-6. [Crossref] [PubMed]
- Nemer SN, Barbas C, Caldeira JB, et al. A new integrative weaning index of discontinuation from mechanical ventilation. Crit Care 2009;13:R152. [Crossref] [PubMed]
- Swets JA. Measuring the accuracy of diagnostic systems. Science 1988;240:1285-93. [Crossref] [PubMed]
- Epstein SK. Routine use of weaning predictors: not so fast. Crit Care 2009;13:197. [Crossref] [PubMed]
- Delisle S, Francoeur M, Albert M, et al. Preliminary Evaluation of a New Index to Predict the Outcome of a Spontaneous Breathing Trial. Respiratory Care 2011;56:1500-5. [Crossref] [PubMed]
- Sassoon CSH, Mahutte CK. Airway Occlusion Pressure and Breathing Pattern as Predictors of Weaning Outcome. Am Rev Respir Dis 1993;148:860-6. [Crossref] [PubMed]
- Conti G, Montini L, Pennisi MA, et al. A prospective, blinded evaluation of indexes proposed to predict weaning from mechanical ventilation. Intensive Care Med 2004;30:830-6. [Crossref] [PubMed]
- Capdevila XJ, Perrigault PF, Perey PJ, et al. Occlusion Pressure and Its Ratio to Maximum Inspiratory Pressure Are Useful Predictors for Successful Extubation Following T-Piece Weaning Trial. Chest 1995;108:482-9. [Crossref] [PubMed]


