
Convulsive status epilepticus as the initial presentation of superwarfarin poisoning: a case report
Introduction
Bromadiolone, a second-generation 4-hydroxycoumarin derivative, is used for the rodent control worldwide (1). Bromadiolone could act as a long-acting anticoagulant by competitively binding with vitamin K 2,3-epoxide reductase enzyme to disrupt the coagulation system of organism (2,3). Thus, bromadiolone is also termed superwarfarin. The wide use and relatively easy access of bromadiolone increases the risk of human poisoning. Patients of bromadiolone poisoning often present with multiorgan hemorrhage, such as skin, urinary system and digestive tract (4). However, neurological symptoms are seldom reported. We present herein a rare case of an 18-year-old male with convulsive status epilepticus as the initial presentation of bromadiolone poisoning. The manuscript was written following the CARE reporting checklist (available at http://dx.doi.org/10.21037/apm-20-1506).
Case presentation
An 18-year-old man was referred to our department with sudden-onset limb weakness, loss of consciousness and generalized tonic-clonic seizures for 8 hours. The seizures lasted 1 to 2 minutes each time. During the interval, the patient was comatose. His medical history was unremarkable. At admission, he was at a consciousness twilight state, with a Glasgow coma score of 8. Upon examination, he was incooperative. Scattered bruises and petechiae over his arms and legs, as well as blood in his nasal cavity were noted. His body temperature was 36.8 °C and the blood pressure was 133/118 mmHg. His neck was supple and the Babinski sign was negative bilaterally. His families denied the history and family history of nervous system disease.
Blood routine test revealed a hemoglobin level of 100 g/L, a leukocyte count of 5.5×109/L and a platelet count of 300×109/L. Urinalysis revealed microscopic hematuria. The prothrombin time (PT) was 30.2 s (normal range, 11–13 s) seconds and the activated partial thromboplastin time (APTT) 47.3 s (normal range, 24–36 s) seconds. The thrombin time and the plasma fibrinogen level were normal. The results of factor assays pointed to vitamin K deficiency: the level of factor II was 0.20 U/mL (normal range, 0.70–1.30 U/mL), of factor VII 0.13 U/mL (normal range, 0.70–1.30 U/mL) and of factor X 0.15 U/mL (normal range, 0.70–1.30 U/mL); the levels of factors V and VIII were within the normal range. Warfarin abuse was hence suspected; however, analysis of two blood samples for warfarin yielded negative results. Lumbar puncture was contraindicated in this situation and was not performed.
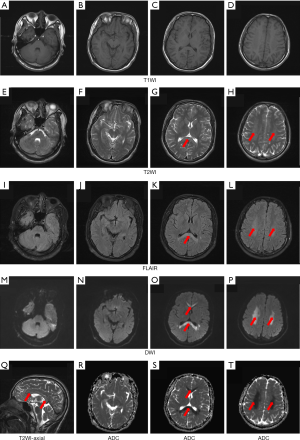
Brain computed tomography (CT) revealed no anomalies. Magnetic resonance imaging (MRI) was performed and lesions in the corpus callosum were found (Figure 1, red arrows). Hyperintensity in T2-weighted imaging (T2WI), fluid-attenuated inversion recovery (FLAIR) and diffusion-weighted imaging (DWI), and hypointensity in apparent diffusion coefficient (ADC) solely involved the whole corpus callosum (Figure 1).
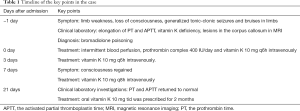
Although warfarin was undetectable in the blood, intoxication was suspected and a serum sample was sent to the Institute for Translational Medicine, the First Hospital of Jinlin University. High-performance liquid chromatography coupled with electrospray ionization tandem mass spectrometry investigation by a reported method revealed the presence of bromadiolone (4,5). The patient was therefore given intermittent blood perfusion and treated with prothrombin complex (factors II, VII, IX, and X) 400 IU/day intravenously for 3 days. Continuous administration of vitamin K (10 mg, q6h) intravenously was given after admission. The patient regained consciousness 7 days after intensive care and treatment. Other neurological symptoms also diminished. We adjusted the dosage of vitamin K to 10 mg q8h intravenously. Further medical history inquiry disclosed that he drank unknown beverage given by a stranger 1 day before his admission. His PT and APTT gradually returned to normal 3 weeks later. Oral vitamin K with the dosage of 10 mg tid was prescribed for 2 months. The time line and key points were shown in Table 1.
Full table
The study conformed to the provisions of the Declaration of Helsinki (as revised in 2013). Written informed consent was signed by the patient for publication of clinical data and the head MRI image.
Discussion
Bromadiolone is a warfarin-like vitamin K antagonist, which inhibits hepatic synthesis of coagulation factors II, VII, IX and X, as well as proteins C and S (6,7). The superwarfarin family include 11 members, i.e., eight 4-hydroxycoumarin namely brodifacoum, bromadiolone, coumachlor, coumafuryl, coumatetralyl, difenacoum, difethialone, and flocoumafen, and three indandione namely chlorophacinone, diphacinone and pindone (8). The identification of some of the superwarfarin compounds in human blood and tissue samples is currently possible only in reference laboratories (1,9,10). Patients who have ingested superwarfarin usually present with unexplained bleeding. However, bleeding was not prominent in some cases. Atypical clinical manifestations, such as unsteady gait, arthralgia, constipation and so forth (Table 2), were occasionally reported (7,11), which may lead to the misdiagnosis of superwarfarin poisoning. In this case, the patient presented with sudden onset limb weakness, loss of consciousness and generalized tonic-clonic seizures. Interestingly, the corpus callosum involvement was the sole neuroimaging manifestation.
The neurological symptom is rarely found in bromadiolone poisoning. Wang et al. firstly reported a 41-year-old male poisoned by bromadiolone with the major chief complaint of dizziness, unsteady gait, and abnormal behaviors (11). They also found lesions in the corpus callosum in heat MRI of the patient. Unlikely, tonic-clonic seizures were notable in our case, which indicated the abnormal electric activity caused by the injury of corpus callosum. According to the limited number of studies, superwarfarins, such as brodifacoum and bromadiolone, could diffuse through the blood-brain barrier because of their lipophilic property (11), and further induce neuroinflammation and neuropathology other than intracranial hemorrhage (12). A proteomic analysis indicated that superwarfarins may change several functional pathways involving of mitochondria function, RNA handling and cell metabolism in astrocytes and microglia (12). The potential mechanism might be the dysfunction of vitamin K-dependent proteins in brain, such as the γ-glutamyl carboxylase (GGC) and growth arrest-specific 6 (GAS6), caused by superwarfarins (4,13). The consumption of vitamin K could reduce the activation of GGC leading to the reduction of sulfatide synthesis and destruction of myelin sheath (14). The reduced function of GAS6 may directly lead to inflammatory activation in glial cells (6). Thus, the supplement of vitamin K would be the etiological treatment for correcting the coagulopathy as well as the neuropathology. Intermittent hemofiltration could eliminate the bromadiolone to avoid the serious accumulation in the central nervous system. In our case, both the central nervous system symptoms and coagulopathy were improved after vitamin K treatment and blood perfusion.
The atypical and initial symptoms of bromadiolone poisoning could present as neurological disorders, such as limb weakness, loss of consciousness, seizures, etc., which increase the difficulty of diagnosis. The unexplained coagulopathy and related drug exposure history would be important clues in our case. For acute neurological symptoms combined with bleeding tendency, poisoning should be considered. Toxicological analysis may help reach an etiological diagnosis which allows prompt therapy.
Conclusions
Bromadiolone poisoning could cause demyelination of the central nervous system and presented as neurological disorders, which is rare but critical and potentially lethal. Timely toxicological identification is necessary for diagnosis and differential diagnosis. The vitamin K treatment is effective for both coagulopathy and central nervous system disorders.
Acknowledgments
Thanks for all nurses of the First Hospital of Jilin University who participated in the treatment of this case.
Funding: This study was supported by grants from Beijing Excellent Talents Training Foundation (No. 2018000020124G144).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-1506
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-1506). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zuo W, Zhang X, Chang JB, et al. Bromadiolone poisoning leading to subarachnoid haemorrhage: A case report and review of the literature. J Clin Pharm Ther 2019;44:958-62. [Crossref] [PubMed]
- King N, Tran MH. Long-Acting Anticoagulant Rodenticide (Superwarfarin) Poisoning: A Review of Its Historical Development, Epidemiology, and Clinical Management. Transfus Med Rev 2015;29:250-8. [Crossref] [PubMed]
- Park BK, Leck JB. A comparison of vitamin K antagonism by warfarin, difenacoum and brodifacoum in the rabbit. Biochem Pharmacol 1982;31:3635-9. [Crossref] [PubMed]
- Feinstein DL, Akpa BS, Ayee MA, et al. The emerging threat of superwarfarins: history, detection, mechanisms, and countermeasures. Ann N Y Acad Sci 2016;1374:111-22. [Crossref] [PubMed]
- Jin MC, Ren YP, Xu XM, et al. Determination of bromadiolone in whole blood by high-performance liquid chromatography coupled with electrospray ionization tandem mass spectrometry. Forensic Sci Int 2007;171:52-6. [Crossref] [PubMed]
- Card DJ, Francis S, Deuchande K, et al. Superwarfarin poisoning and its management. BMJ Case Rep 2014;2014:bcr2014206360 [Crossref] [PubMed]
- Kelkar AH, Smith NA, Martial A, et al. An Outbreak of Synthetic Cannabinoid-Associated Coagulopathy in Illinois. N Engl J Med 2018;379:1216-23. [Crossref] [PubMed]
- Lo VM, Ching CK, Chan AY, et al. Bromadiolone toxicokinetics: diagnosis and treatment implications. Clin Toxicol (Phila) 2008;46:703-10. [Crossref] [PubMed]
- Rutović S, Dikanović M, Mirković I, et al. Intracerebellar hemorrhage caused by superwarfarin poisoning. Neurol Sci 2013;34:2071-2. [Crossref] [PubMed]
- Ma M, Zhang M, Tang X, et al. Massive neonatal intracranial hemorrhage caused by bromadiolone: A case report. Medicine (Baltimore) 2017;96:e8506 [Crossref] [PubMed]
- Wang M, Yang Y, Hou Y, et al. Effects of bromadiolone poisoning on the central nervous system. Neuropsychiatr Dis Treat 2017;13:2297-300. [Crossref] [PubMed]
- Kalinin S, Marangoni N, Kowal K, et al. The Long-Lasting Rodenticide Brodifacoum Induces Neuropathology in Adult Male Rats. Toxicol Sci 2017;159:224-37. [Crossref] [PubMed]
- Binder MD, Cate HS, Prieto AL, et al. Gas6 deficiency increases oligodendrocyte loss and microglial activation in response to cuprizone-induced demyelination. J Neurosci 2008;28:5195-206. [Crossref] [PubMed]
- Eckhardt M. The role and metabolism of sulfatide in the nervous system. Mol Neurobiol 2008;37:93-103. [Crossref] [PubMed]



