The predictive value of postoperative C-reactive protein (CRP), procalcitonin (PCT) and triggering receptor expressed on myeloid cells 1 (TREM-1) for the early detection of pulmonary infection following laparoscopic general anesthesia for cervical cancer treatment
Introduction
Cervical cancer is a common malignant tumor in women with high incidence and mortality. At present, the clinical treatment of cervical cancer mainly involves radical resection (1). However, this is sometimes complicated by pulmonary infection which not only increases patient discomfort and lengthens the hospital stay but can also easily lead to acute respiratory insufficiency, damage the function of other organs, and even lead to death (2). The timely diagnosis of pulmonary infection after laparoscopic general anesthesia for cervical cancer treatment and effective intervention is of great significance to improving the prognosis of patients. Studies have shown that (3) inflammatory factors can play a key role during the development of pulmonary infection after cervical cancer surgery, which can lead to significant changes to serological indicators. Triggering receptor expressed on myeloid cells 1 (TREM-1) is a key mediator of inflammatory responses after trauma and infection, while C-reactive protein (CRP) and procalcitonin (PCT) are also important inflammatory factors (4,5). In this study we analyzed the predictive value of the early detection of postoperative CRP, PCT, and TREM-1 for pulmonary infection after laparoscopic general anesthesia for cervical cancer treatment and aimed to provide a scientific reference for clinical treatment. We present the following article in accordance with the STARD reporting checklist (available at http://dx.doi.org/10.21037/apm-21-554).
Methods
General information
Eighty patients who underwent radical cervical cancer surgery in our hospital from March 2018 to March 2020 were selected as research subjects. All patients agreed to participate in this study and signed an informed consent form. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Sichuan Provincial People’s Hospital, University of Electronic Science and Technology of China (No. 20180203). The inclusion criteria were all of the following: (I) pulmonary infection based on Dilworth’s scoring criteria for a lung infection after abdominal surgery and the diagnostic criteria for hospital-acquired bronchopulmonary infection established by the Respiratory Society of the Chinese Medical Association. Specifically, this was determined on the basis that (i) the number of coughs or original coughs increased after operation; (ii) an oral temperature >38 °C which lasted more than 24 h; (iii) new invasive changes in the chest were detected; (iv) thickened and increased sputum were present; (v) the white blood cell count >11×109/L; and (vi) rales were present in the lungs. Among these criteria, item (iv) was allocated 3 points, and the other items were each allocated 1 point, and a diagnosis of pulmonary infection was established when the cumulative score was ≥4 points (6). (II) Patients who did not have serious complications. (III) Patients who met the diagnostic criteria for cervical cancer; and (IV) the clinical data of the patient was complete. The exclusion criteria were any of the following: (I) patients who received relevant treatment before enrollment; (II) patients who were complicated with severe infection symptoms; (III) patients with coagulation disorders or previous malignant tumors; and (IV) patients who failed to tolerate the treatment plan or withdrew from treatment. According to whether the patients were complicated by postoperative pulmonary infection, they were divided into an infected group (n=34) and non-infected group (n=46). The infection group comprised of 18 males and 16 females with an age range between 28 and 72 years, and an average age of 41.60±5.73 years. There were 25 males and 21 females in the uninfected group, with an age range of between 28 and 70 years, and an average age of 41.58±5.71 years. As the general information of the two groups was not statistically different, the results were comparable (P>0.05).
Detection method
We collected 5 mL of fasting blood before the operation and 24 h after operation from each group. After centrifugation (3,500 r/min, 5 min, r=8 cm), the separated serum was collected and placed in a Roche E411 automatic electrochemiluminescence analyzer to detect the PCT level. The concentration of CRP and TREM-1 in the two groups was determined by the Enzyme-Linked Immune Sorbent Assay (ELISA) method (7). The reagents used in the test were provided by the Beijing Meikang Biotechnology Research Center Co., Ltd. and the measurement was carried out following the instructions of the ELISA kit.
Statistical analysis
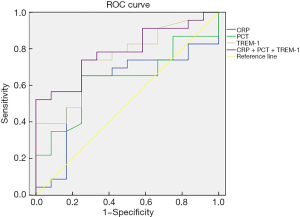
SPSS22.0 software was used to analyze the data. The measurement data were expressed as mean ± standard deviation (), and the comparison between the two groups was tested by t-test. The count data was expressed as a percentage (%), and the χ2 test was used for comparison. Logistic regression analysis was used to analyze the risk factors of pulmonary infection in patients who underwent laparoscopic general anesthesia for cervical cancer treatment. The ROC curve was used to analyze the predictive value of CRP, PCT, and TREM-1 individually and combined for the occurrence of pulmonary infection, and the cut off value for α was set to 0.05.
Results
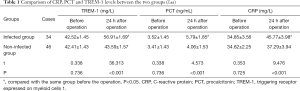
Comparison of CRP, PCT, and TREM-1 levels between the two groups
While the before operation levels of CRP, PCT, and TREM-1 were not statistically significant between the two groups, the levels of CRP, PCT, and TREM-1 in the non-infected group were higher than those in the infected group (P<0.05), as shown in Table 1.
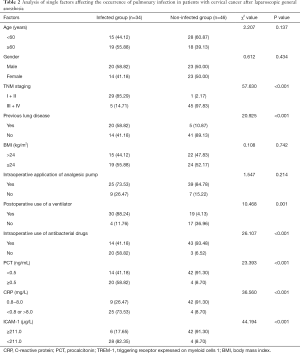
Single-factor analysis of pulmonary infection in patients after laparoscopic general anesthesia for cervical cancer treatment
There was no significant correlation between age, gender, BMI, or the intraoperative application of analgesic pumps, and pulmonary infection in patients after surgery. However, tumor TNM staging (III + IV), previous lung disease (yes), postoperative use of a ventilator (yes), intraoperative use of antibacterial drugs (yes), PCT (≥0.5 ng/mL), CRP (<0.8 or 8.0 mg/L), and ICAM-1 (<211.0 µg/L) were significantly correlated with pulmonary infection (P<0.05), as shown in Table 2.
Full table
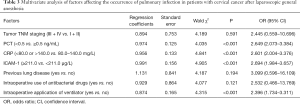
Analysis of multiple factors affecting the occurrence of pulmonary infection in patients after laparoscopic general anesthesia for cervical cancer treatment
The postoperative application of a ventilator (yes), PCT (≥0.5 ng/mL), CRP (<0.8 or >8.0 mg/L), and ICAM-1 (<211.0 µg/L) were all independent factors that can affect the occurrence of pulmonary infection (P<0.05) as shown in Table 3.
Full table
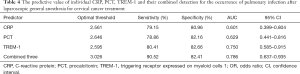
The predictive value of individual CRP, PCT, TREM-1 and their combined detection for the occurrence of pulmonary infection after laparoscopic general anesthesia for cervical cancer treatment
The ROC curve was used to analyze the predictive value of individual CRP, PCT, TREM-1 levels, and their combined detection. The AUC for individual CRP, PCT, TREM-1 and combined detection of the three for the prediction of the occurrence of pulmonary infection was 0.601, 0.629, 0.750, and 0.786, respectively, where combined detection achieved the best predictive performance, as shown in Table 4 and Figure 1.
Full table
Discussion
General anesthesia is a commonly used method of anesthesia for large-scale clinical operations (8). Several factors have been identified as contributing to the likelihood of post-operative infection following general anesthesia. The low immune function of patients with cervical cancer, and fluid and blood loss during laparoscopic surgery increase the likelihood of post-operative infection and invasion of multiple pathogens (9).
The likelihood of pulmonary infection may also increase when the tracheal intubation airbag is over-inflated and compresses the tracheal mucosa, resulting in ischemia which can promote lung infection (10). Restricted post-operative thoracic movement resulting from a painful incision, chest drainage tube irritation, or tight chest strap, and the general reduction in airflow velocity and cough force seen in some cancer patients can lead to difficulty discharging sputum, further increasing the probability of infection (11,12). Most patients after surgery also have a limited amount of body fluids and an increased flow of inhaled oxygen, which can easily lead to thick sputum which is difficult to cough up (13). For these reasons, the early diagnosis of pulmonary infection is both important and the focus of the current research. Studies have pointed out that the detection of serum-related inflammatory factors can significantly improve the sensitivity and specificity of diagnosis which is particularly important in cases where a typical clinical and chest imaging manifestations are present (14).
PCT is an intermediate product in the production of calcitonin, which is normally produced and secreted by C cells in the thyroid. Once the body is infected, PCT can be detected in all organs, and its serum level can be significantly increased (15). Therefore, PCT has always been used as an important indicator reflecting the severity of infectious bacterial inflammation. Furthermore, studies (16) have shown that PCT has a short half-life (approximately 25–30 h), which can quickly reflect the effect of treatment and provide effective support for the clinical assessment of patient prognosis. The results of this study show that PCT was abnormally elevated in patients with pulmonary infection after laparoscopic general anesthesia for cervical cancer treatment 24 h after surgery, and was also one of the independent risk factors affecting patients with pulmonary infection. This suggests PCT can be used as an important indicator for the early judgment and evaluation of pulmonary infection.
CRP is an acute-phase reactive protein which can rise sharply when the body is infected or damaged. In this study, CRP levels were detected in 80 patients with cervical cancer after general anesthesia. After 24 h, CRP levels were abnormally increased in patients with pulmonary infection which is consistent with the results of previous studies (17), and suggests that CRP was involved in the occurrence of the disease. One possible explanation is that the massive production and aggregation of CRP and other cytokines can cause neuronal cell damage and apoptosis of astrocytes, inducing a cascade reaction of cytokines which can promote the occurrence of pulmonary inflammation (18).
TREM-1 belongs to the TREM family. Early studies have shown that the expression of TREM-1 on the surface of neutrophils was significantly increased in conditions including bacterial peritonitis, septic shock, bacterial pneumonia, and skin damage, while there was no significant increase in inflammation seen in non-microbial infections. Studies have also proposed that changes in the level of TREM-1 in plasma may be one of the body’s self-protection mechanisms against inflammation, and the inhibition of TREM-1 may reduce the degree of inflammation (19). The results of this study show that TREM-1 was an independent risk factor for pulmonary infections, suggesting the detection of serum TREM-1 in patients can help diagnose bacterial infections and assess the prognosis of patients.
The predictive value of PCT, CRP, and TREM-1 in the early detection of pulmonary infection after laparoscopic general anesthesia for cervical cancer treatment was confirmed in this study via logistic regression. Furthermore, the results of the ROC curve showed that the highest performance was achieved in terms of AUC, sensitivity, and specificity when these three indicators were combined. This may be because when PCT, CRP, and TREM-1 are separately used to assess patient prognosis, their performance is susceptible to systemic inflammatory reactions, such as seen with tissue damage, and a synergistic effect is established when the three are combined (20).
The shortcomings of this study are that the sample size is small, the sample inclusion is restricted by region, and the time span is large. The results have certain limitations, which need to be strengthened and discussed in depth in the later period.
In summary, the level of PCT, CRP, and TREM-1 is abnormally increased in patients with pulmonary infection after laparoscopic general anesthesia for cervical cancer treatment. The combined detection of the three can be used as an effective means to predict the occurrence of pulmonary infection in the early stage and initiate timely clinical interventions to improve patient prognosis.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STARD reporting checklist. Available at http://dx.doi.org/10.21037/apm-21-554
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-21-554
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-21-554). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Sichuan Provincial People’s Hospital, University of Electronic Science and Technology of China (No. 20180203). All patients agreed to participate in this study and signed an informed consent form.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Branche A, Neeser O, Mueller B, et al. Procalcitonin to guide antibiotic decision making. Curr Opin Infect Dis 2019;32:130-5. [Crossref] [PubMed]
- Cervical Cancer Analysis Reveals New Mutations. Cancer Discov 2017;7:344.
- Tsikouras P, Zervoudis S, Manav B, et al. Cervical cancer: Screening, diagnosis, and staging. J BUON 2016;21:320-5. [PubMed]
- Marquina G, Manzano A, Casado A. Targeted Agents in Cervical Cancer: Beyond Bevacizumab. Curr Oncol Rep 2018;20:40. [Crossref] [PubMed]
- Hu Z, Ma D. The precision prevention and therapy of HPV-related cervical cancer: new concepts and clinical implications. Cancer Med 2018;7:5217-36. [Crossref] [PubMed]
- Olusola P, Banerjee HN, Philley JV, et al. Human Papilloma Virus-Associated Cervical Cancer and Health Disparities. Cells 2019;8:622-5. [Crossref] [PubMed]
- Printz C. Cervical cancer self-sampling tests could improve access. Cancer 2019;125:1583. [Crossref] [PubMed]
- Srinivasan R. Cervical cancer genomics: an initial step towards personalized approach to therapy. EBioMedicine 2019;43:11-2. [Crossref] [PubMed]
- Mruts KB, Gebremariam TB, et al. Knowledge and Perception Towards Cervical Cancer among Female Debre Berhan University Students. Asian Pac J Cancer Prev 2018;19:1771-7. [PubMed]
- Bourgin C, Estevez JP, Collinet P. Post therapeutic cervical cancer surveillance in France: Priority for examination. Gynecol Obstet Fertil Senol 2018;46:503-5. [PubMed]
- SaeiGhare Naz M. Educational Interventions for Cervical Cancer Screening Behavior of Women: A Systematic Review. Asian Pac J Cancer Prev 2018;19:875. [PubMed]
- Gibot S, Jolly L, Lemarié J, et al. Triggering Receptor Expressed on Myeloid Cells-1 Inhibitor Targeted to Endothelium Decreases Cell Activation. Front Immunol 2019;10:2314-6. [Crossref] [PubMed]
- Peng L, Zhou Y, Dong L, et al. TGF-β1 Upregulates the Expression of Triggering Receptor Expressed on Myeloid Cells 1 in Murine Lungs. Sci Rep 2016;6:18946-9. [Crossref] [PubMed]
- Gadducci A, Cosio S. Neoadjuvant Chemotherapy in Locally Advanced Cervical Cancer: Review of the Literature and Perspectives of Clinical Research. Anticancer Res 2020;40:4819-28. [Crossref] [PubMed]
- Nair S, Huynh JP, Lampropoulou V, et al. Irg1 expression in myeloid cells prevents immunopathology during M. tuberculosis infection. J Exp Med 2018;215:1035-45. [Crossref] [PubMed]
- Moutachakkir M, Lamrani HA, Baraou A, et al. Immunoanalytical characteristics of C-reactive protein and high sensitivity C-reactive protein. Ann Biol Clin (Paris) 2017;75:225-9. [Crossref] [PubMed]
- Dyer EM, Waterfield T, Baynes H. How to use C-reactive protein. Arch Dis Child Educ Pract Ed 2019;104:150-3. [Crossref] [PubMed]
- Yao Z, Zhang Y, Wu HB. Regulation of C-reactive protein conformation in inflammation. Inflamm Res 2019;68:815-23. [Crossref] [PubMed]
- Philipp S, Rebekka B, Meret M, et al. Procalcitonin-guided antibiotic therapy algorithms for different types of acute respiratory infections based on previous trials. Expert Rev Anti Infect Ther 2018;85:331-6.
- Lippi G, Plebani M. Procalcitonin in patients with severe coronavirus disease 2019 (COVID-19): A meta-analysis. Clin Chim Acta 2020;505:190-1. [Crossref] [PubMed]
(English Language Editor: B. Draper)