Editor’s note: “Palliative Radiotherapy Column” features articles emphasizing the critical role of radiotherapy in palliative care. Chairs to the columns are Dr. Edward L.W. Chow from Odette Cancer Centre, Sunnybrook Health Sciences Centre in Toronto and Dr. Stephen Lutz from Blanchard Valley Regional Cancer Center in Findlay, gathering a group of promising researchers in the field to make it an excellent column. The column includes original research manuscripts and timely review articles and perspectives relating to palliative radiotherapy, editorials and commentaries on recently published trials and studies.
Stereotactic body radiation therapy for non-spine bone metastases—a review of the literature
Introduction
Bone metastases are common in advanced cancer, with 70−85% of patients diagnosed with bone metastases at the time of autopsy (1). Conventional palliative radiation therapy has been proven to decrease pain and improve quality of life; however, no increase in overall survival has been reported (2-4). New advances in radiation treatment, however, may be able to improve overall survival and local control rates.
Stereotactic body radiation therapy (SBRT) for bone metastases is a recent technological advance for the treatment of oligometastatic disease. SBRT is able to deliver significantly higher biologically equivalent doses (BED) as compared to conventional radiation. As defined by the Canadian Association of Radiation Oncologists (CARO), SBRT is “the precise delivery of highly conformal and image-guided hypofractionated external beam radiotherapy, delivered in a single or few fraction(s), to an extra-cranial body target with doses at least biologically equivalent to a radical course when given over a protracted conventionally fractionated (1.8−3.0 Gy/fraction) schedule” (5). Thus, SBRT is able to shift the goal of therapy to maximizing both local tumour control and pain reduction, as opposed to pain and symptom relief alone. As SBRT is still a relatively new field, information on the toxicities, and outcomes associated with such treatment are still to be learned.
In bone metastases, there are three main potential indications for utilizing SBRT as a treatment. The first indication is retreatment to a site that has previously been irradiated with conventional external beam radiation (5,6). The next indication is in oligometastases with five or less metastatic sites (7). The third indication is oligometastatic progression in patients with widespread metastases; however, one or two areas may be significantly worse. SBRT is able to target these few areas that are either causing pain or have progressed on radiography. The purpose of this literature review was to determine the outcomes as well as toxicities associated with SBRT treatment of non-spine bone metastases.
Methods
A literature search was conducted to find studies that pertained to SBRT in patients with non-spine bone metastases. Articles were examined independently by Bedard G and Chow E to determine eligibility for the review. Articles that involved bones of the skull base were excluded. Due to the relatively small number of studies investigating SBRT treatment of non-spine bone metastases, studies that included other sites of metastases as well as bone metastases were included.
Studies were then examined for their inclusion and exclusion criteria. Data was extracted under the headings of: sample size, age, primary cancer site, SBRT dose, areas of treatment, concurrent treatment, endpoints, local control, survival, and toxicity. As the dosing regimens varied between studies, we calculated the BED for each study (8). A α/β of 7 was used for renal cell carcinoma as it is relatively radioresistant, while a α/β of 10 was used for all other tumors (8).
Results
Fourteen studies were found that fit the search criteria. Only two studies by Jhaveri et al. (8) and Owen et al. (9) specifically reported outcomes and toxicities of SBRT for non-spine bone metastases. All other studies included other sites of metastases in their analysis of outcomes and toxicities. Sample size of the studies ranged from 8 to 206 patients. There was also a large variance in primary cancer site, SBRT dose and areas of treatment (Table 1). Inclusion and exclusion criteria for each individual study were extracted (Table 2). The majority of studies required patients to be over the age of 18 with a pathologically confirmed metastatic cancer. Most studies included patients with oligometastatic disease (five or less metastases), a relatively good performance status, and a life expectancy greater than 3 months.

Full table
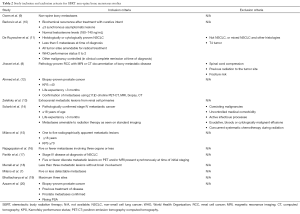
Full table
Typical outcomes included local control, overall survival and progression free survival. Local control was defined as: stable disease, partial response or complete response based on imaging (9), lack of tumor progression at the treated site (12), or using the RECIST criteria (7,21). As per the RECIST criteria: complete response is the disappearance of all lesions, partial response is a ≥30% decrease in size from baseline, progressive disease is defined as a ≥20% increase in size and stable disease is neither a partial response nor progressive disease (21). Some studies did not give a definition for local control (18).
In studies that reported local control rates, these rates were greater than 85% in all studies (7,9,10,16,18,19). Median overall survival varied and was cited as 9.3 months (9), 13.5 months (11), 31.7 months (14), and 32 months (15). Progression free survival also varied significantly between the studies. Due to the large variance in endpoints among the studies, conclusions of overall local control and progression free survival were near impossible to make.
Jhaveri et al. found that in patients who were treated with a BED greater than 85, mean time to decrease in pain score was 1 week and 83% of patients had a response to treatment, which was an improvement over those who were treated with a BED less than 85 (8). Through a review of the BED of all other studies, and evaluation of the local control and overall survival of each of the studies, it appears that patients who received a higher BED had a better outcome to treatment, echoing the findings of Jhaveri et al. There was no difference in patients who received multiple fractions as opposed to single fraction treatment.
Toxicity data are listed in Table 1. Very rarely were grade 3 and 4 toxicities observed (7,11,13,16). Toxicities that occurred most frequently included dermatitis (8,9,13), dyspnea (9,11), and fracture (9,13). There was no trend between BED and severity of toxicity. However, single fraction treatments appear to have a greater percentage of patients experiencing toxicity than multiple fraction treatments (9,12,16). For studies where greater than 50% of patients were treated with single fraction treatment, toxicity data was pooled and overall percentages of patients who experienced toxicity was calculated. Approximately 24% of patients undergoing single fraction treatment (9,12,16,18) vs. 12% of patients undergoing multiple fraction treatments (7,8,10,11,20) experienced some sort of acute or late treatment toxicity. The numbers above are estimates based on the reported toxicities of each of the studies; bearing in mind that sites treated other than bone metastases may have been included in the analysis in each of the studies as well. Due to the variance in dose between and within studies, we are unable to determine which toxicities were more likely for single and multiple fraction treatments.
Discussion
SBRT appears to be a feasible and safe treatment option for patients with non-spine bone metastases. However, due to the lack of endpoint consistency between clinical trials, it proves to be difficult to pool and analyze data. A consensus on SBRT endpoints is necessary in order to standardize the reporting of outcome assessment and allow comparison across trials.
In the conventional radiation setting, the international consensus of bone metastases has been developed for clinical endpoints (3). Response categories were based on patient reported pain scores and analgesic consumption. A complete response to treatment was defined as a pain score of 0 out of 10 at the treated site with no concomitant increase in analgesic intake, while a partial response was defined as a pain reduction of 2 or more at the treated site without analgesic increase, or an analgesic reduction of 25% with no increase in pain score or 1 point above baseline. Pain progression was defined as an increase in pain score of 2 or more above baseline with stable analgesic intake or an analgesic increase of 25% with stable pain score. Lastly an indeterminate response was any response not captured in the above definitions (3). These definitions, however, are not directly transferable to the SBRT patient population, due to the differing indications for treatment with SBRT.
The three major potential indications for SBRT differ from those of conventional treatment (5). These include: need for retreatment, oligometastatic disease and oligometastatic progression. If the treatment goal is to decrease pain; this can be evaluated by using the endpoints outlined by the international consensus. For patients with oligometastatic disease, utilizing the Response Evaluation Criteria in Solid Tumors (RECIST) criteria for asymptomatic lesions (21) is appropriate. In asymptomatic lesions, radiological imaging becomes increasingly important. When there is soft tissue involvement in the bone metastases, as per the RECIST criteria, the response rates should be defined as follows: complete response is the disappearance of all lesions, partial response is a ≥30% decrease in size from baseline, progressive disease is defined as a ≥20% increase in size and stable disease is neither a partial response or progressive disease (21). The RECIST criteria however are not feasible to use to determine response of bone metastases without soft tissue involvement.
In bone metastases after radiation treatment, remineralization may occur. There have been two publications in conventional radiation treatment assessing the remineralization and computed tomography (CT) density changes following treatment (22,23). Koswig and Budach observed that a more fractionated schedule was more effective for the recalcification of bone most likely due to the greater biological efficacy (22). Another study also reported that remineralization of osteolytic lesions occurs after palliative radiotherapy with gradual increases in median percent density change as the dose and fractionation increases (23). There may be increased recalcification in patients undergoing SBRT due to the higher BED of this treatment. Future studies should investigate the use of CT density in order to determine response rates.
In these oligometastatic patients, the endpoints of local control and prevention of distant metastases would be useful in determining the outcomes of SBRT. Tumor markers such as prostate specific antigen (PSA) in prostate cancer, progression free and overall survival are important secondary endpoints. In patients who have widespread metastases with oligometastatic progression, differing endpoints again need to be defined. These patients may perhaps have one to two new areas that are causing increased symptoms or are increasing in size. If these lesions are symptomatic, the international consensus endpoint definitions should be followed. If they are asymptomatic, the RECIST criteria for response assessment can be used if a soft tissue component is involved. In this population the occurrence of distant metastases becomes a less significant issue as these patients already have metastases elsewhere. As there are differing indications for SBRT, there should also be different ways to assess the treatment outcomes.
The majority of the studies included in this review involved numerous sites of metastases, and some did not differentiate between bone and non-bone metastatic sites. Therefore, pooled toxicity and outcome data may not be completely accurate for the non-spine bone metastatic sites alone. This review suggests that single and multiple fraction SBRT treatment have similar outcomes in terms of local control and severity of side effects, albeit single fraction treatment may have an increased frequency of toxicity. A randomized trial of single vs. multiple fraction SBRT treatment is warranted to determine if there is a dose-response phenomenon.
Acknowledgements
We thank the generous support of Bratty Family Fund, Michael and Karyn Goldstein Cancer Research Fund, Joey and Mary Furfari Cancer Research Fund, Pulenzas Cancer Research Fund, Joseph and Silvana Melara Cancer Research Fund, and Ofelia Cancer Research Fund.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Tubiana-Hulin M. Incidence, prevalence and distribution of bone metastases. Bone 1991;12 Suppl 1:S9-10. [PubMed]
- Li KK, Chow E, Chiu H, et al. Effectiveness of Palliative Radiotherapy in the Treatment of Bone Metastases Employing the Brief Pain Inventory. Journal of Cancer Pain & Symptom Palliation 2006;2:19-29.
- Chow E, Hoskin P, Mitera G, et al. Update of the international consensus on palliative radiotherapy endpoints for future clinical trials in bone metastases. Int J Radiat Oncol Biol Phys 2012;82:1730-7. [PubMed]
- Chow E, Harris K, Fan G, et al. Palliative radiotherapy trials for bone metastases: a systematic review. J Clin Oncol 2007;25:1423-36. [PubMed]
- Sahgal A, Roberge D, Schellenberg D, et al. The Canadian Association of Radiation Oncology scope of practice guidelines for lung, liver and spine stereotactic body radiotherapy. Clin Oncol (R Coll Radiol) 2012;24:629-39. [PubMed]
- Takahashi T, Nishimura K, Yamano T, et al. Role of Palliative Radiotherapy for Bone Metastasis. J Palliat Care Med 2014;4:171.
- Milano MT, Katz AW, Zhang H, et al. Oligometastases treated with stereotactic body radiotherapy: long-term follow-up of prospective study. Int J Radiat Oncol Biol Phys 2012;83:878-86. [PubMed]
- Jhaveri PM, Teh BS, Paulino AC, et al. A dose-response relationship for time to bone pain resolution after stereotactic body radiotherapy (SBRT) for renal cell carcinoma (RCC) bony metastases. Acta Oncol 2012;51:584-8. [PubMed]
- Owen D, Laack NN, Mayo CS, et al. Outcomes and toxicities of stereotactic body radiation therapy for non-spine bone oligometastases. Pract Radiat Oncol 2014;4:e143-9. [PubMed]
- Berkovic P, De Meerleer G, Delrue L, et al. Salvage stereotactic body radiotherapy for patients with limited prostate cancer metastases: deferring androgen deprivation therapy. Clin Genitourin Cancer 2013;11:27-32. [PubMed]
- De Ruysscher D, Wanders R, van Baardwijk A, et al. Radical treatment of non-small-cell lung cancer patients with synchronous oligometastases: long-term results of a prospective phase II trial (Nct01282450). J Thorac Oncol 2012;7:1547-55. [PubMed]
- Ahmed KA, Barney BM, Davis BJ, et al. Stereotactic body radiation therapy in the treatment of oligometastatic prostate cancer. Front Oncol 2013;2:215. [PubMed]
- Zelefsky MJ, Greco C, Motzer R, et al. Tumor control outcomes after hypofractionated and single-dose stereotactic image-guided intensity-modulated radiotherapy for extracranial metastases from renal cell carcinoma. Int J Radiat Oncol Biol Phys 2012;82:1744-8. [PubMed]
- Solanki AA, Weichselbaum RR, Appelbaum D, et al. The utility of FDG-PET for assessing outcomes in oligometastatic cancer patients treated with stereotactic body radiotherapy: a cohort study. Radiat Oncol 2012;7:216. [PubMed]
- Milano MT, Philip A, Okunieff P. Analysis of patients with oligometastases undergoing two or more curative-intent stereotactic radiotherapy courses. Int J Radiat Oncol Biol Phys 2009;73:832-7. [PubMed]
- Rajagopalan MS, Clump DA, Heron DE, et al. Initial Report of a Prospective Phase 2 Study Including Patient-Reported Quality of Life Data of Stereotactic Body Radiation Therapy (SBRT) for Patients With Oligometastatic Disease. Int J Radiat Oncol Biol Phys 2013;87:S570.
- Parikh RB, Cronin A, Kozono DE, et al. Factors Associated With Survival in Patients With Oligometastatic Non-Small Cell Lung Cancer (NSCLC). Int J Radiat Oncol Biol Phys 2013;87:S202.
- Merrell KW, Barney BM, Yan E, et al. A Comparison of Standard Fractionation and Stereotactic Body Radiation Therapy in the Treatment of Metastatic Breast Cancer. Int J Radiat Oncol Biol Phys 2013;87:S232-3.
- Bhattacharya IS, Woolf DK, Hughes RJ, et al. Stereotactic body radiotherapy (SBRT) in the management of extracranial oligometastatic (OM) disease. Br J Radiol 2015;88:20140712. [PubMed]
- Azzam G, Lanciano R, Arrigo S, et al. SBRT: An Opportunity to Improve Quality of Life for Oligometastatic Prostate Cancer. Front Oncol 2015;5:101. [PubMed]
- van Persijn van Meerten EL, Gelderblom H, Bloem JL. RECIST revised: implications for the radiologist. A review article on the modified RECIST guideline. Eur Radiol 2010;20:1456-67. [PubMed]
- Koswig S, Budach V. Remineralization and pain relief in bone metastases after after different radiotherapy fractions (10 times 3 Gy vs. 1 time 8 Gy). A prospective study. Strahlenther Onkol 1999;175:500-8. [PubMed]
- Chow E, Holden L, Rubenstein J, et al. Computed tomography (CT) evaluation of breast cancer patients with osteolytic bone metastases undergoing palliative radiotherapy--a feasibility study. Radiother Oncol 2004;70:291-4. [PubMed]


