
Efficacy and safety of acupuncture in treating acute low back pain: a systematic review and bayesian network meta-analysis
Introduction
Low back pain is now recognized as a major public health problem worldwide, with nearly 80% of the population experiencing low back pain in their lifetime (1). Evidence suggests that low back pain has a mean point prevalence of 20%, and a lifetime prevalence of 40% (2). Acute low back pain (ALBP) refers to pain that lasts between 24 hours and 12 weeks (3). ALBP is often nonspecific, hence it cannot be attributed to a specific cause (4). Nevertheless, the possible causes of ALBP include tumor, infection, trauma, osteoporosis, and inflammatory arthritis (5-7). While intense pain and physical disability resulting from ALBP have seriously affected the life quality of patients and posed a significant economic burden, there is a need to figure out the efficacy of interventions in treating ALBP (6-8).
Many pharmacologic and non-pharmacologic treatments are available for ALBP, but the jury is still out on the comparative efficacy among them. Treatments include nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, physical therapy modalities, superficial heat, spinal manipulative therapy, acupuncture, exercise therapy, and others (4-7,9,10).
Acupuncture, an important component of Traditional Chinese Medicine (TCM), has shown its striking utility of pain alleviation in clinical practice and experimental evidence (11,12). Several systematic reviews have also confirmed the effectiveness of acupuncture therapies in treating ALBP (13-15). With regards to various types of acupuncture therapies for managing ALBP, researchers have expressed their attentions on manual acupuncture (MA), electroacupuncture (EA), motion style acupuncture (MSA), and so on. However, previous systematic reviews usually considered all the acupuncture therapies as a whole to evaluate its effectiveness. Thus, it remains unclear which acupuncture therapies are the most effective for ALBP.
Network meta-analysis (NMA) has been increasingly prevalent in medical research (16). Through a combination of direct and indirect comparisons, NMA allows the comparison of multiple interventions and ranking of different interventions (17). In this study, we conducted a Bayesian NMA to compare the efficacy and safety of different acupuncture therapies adopted in ALBP treatment. It is hoped that this work will serve as an acupuncture treatment selection guideline for ALBP. We present the following article in accordance with the PRISMA reporting checklist (available at http://dx.doi.org/10.21037/apm-21-551).
Methods
The study was registered at INPLASY under the code INPLASY2020120025, available at: https://inplasy.com/inplasy-2020-12-0025/.
Data sources and searches
We systematically searched PubMed, Cochrane Library, Embase, Web of Science, China National Knowledge Infrastructure (CNKI), VIP Database, Wanfang Database, and Chinese Biomedical Database (CBM) for randomized controlled trials (RCTs) from the date of their inception to 17 December 2020. The search was limited to studies published in English and Chinese. Full search details are shown in Appendix 1.
Study selection
Titles, abstracts, and full texts were screened independently by two reviewers (B Wu, L Yang). Disagreements were resolved through discussion with the third reviewer (C Fu). Studies were included if met the following criteria: (I) types of studies: RCTs testing acupuncture for ALBP; (II) types of participants: patients were diagnosed with ALBP (<12 weeks); (III) types of interventions: comparative interventions included acupuncture therapies (including MA, EA, and MAS. Table 1), pharmacotherapy (western medicine) and placebo; (IV) types of outcomes: the studies must include at least one of the following outcomes: visual analog scale (VAS) score, lumbar range of motion (ROM) score, and adverse events. The following were excluded: (I) duplicated literature; (II) protocol, case report, reviews, meta-analyses, conference abstracts, and animal experiments; (III) studies without sufficient data; (IV) combined interventions consisting of two or more acupuncture therapies; (V) studies that evaluated the combined effect of acupuncture and other related therapies; (VI) single acupuncture technique with different acupoints.

Full table
Data extraction and quality assessment
Two reviewers (B Wu, L Yang) screened all the studies for inclusion and performed the data extraction. All the discrepancies were reconciled by discussion with a third reviewer (C Fu). For each of the selected studies, the following information was extracted: author, publication year, country, mean age, gender, interventions of treatment and control groups, sample size, and outcome. We recorded the outcomes as close to 2 weeks as possible for all analyses.
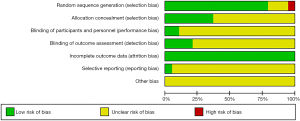
Study quality was assessed using the Cochrane risk-of-bias tool (18). This tool examined six major domains of bias: selection bias, performance bias, detection bias, attrition bias, reporting bias, and other bias. Each domain was categorized as low risk, high risk, and unclear risk. Critical appraisal of studies was carried out independently by two reviewers (G Jian, Y Zhuo). All the differences were resolved through discussion with a third reviewer (M Yao).
Statistical analysis
First of all, the pairwise meta-analysis was performed using RevMan 5.3. Cochran’s I-square (I2) statistic was used to assess the heterogeneity of the results (19). A fixed-effects model was selected when I2 value <50%, otherwise a random-effects model was used. For continuous outcomes, mean difference (MD) or standard mean difference (SMD) with 95% confidence interval (CI) was used. Then, the NMA was performed in a Bayesian framework using Markov Chain Monte Carlo (MCMC) methods by WinBUGS 1.4. A random-effects model was employed because of anticipated heterogeneity. SMD with 95% CI was presented for continuous outcomes. Furthermore, the surface under the cumulative ranking curve (SUCRA) was applied to rank the size effect of treatments (20). In this study, the higher the SUCRA value is, the better the rank of the treatment, and vice versa (21). The node-splitting method was used to assess the inconsistency between direct and indirect evidence. We assessed the publication bias by funnel plots. Sensitivity analyses were used to evaluate the robustness of the results. The generation of result figures was performed using RevMan 5.3 and STATA 14 software.
Results
Study selection
Based on the search strategy, a total of 1,883 studies were identified from these databases. After eliminating duplicates, the titles and abstracts of 996 articles were screened. In the end, 95 articles were selected for full-text screening, and 19 studies (22-40) were included in the data synthesis. Full details of the selection process are shown in Figure 1.
Study characteristics
A total of 19 studies were used for the final Bayesian NMA. All eligible studies were published between 2008 and 2020. Four of these studies were written in English, while fifteen studies were in Chinese. The participant sample size ranged from 13 to 113, and 779 (54.59%) of the 1,427 total participants were males. Participants’ mean ages ranged from 25.30 to 47.00 years. Interventions of 19 RCTs included MSA, EA, MA, pharmacotherapy, and placebo. Besides, all 19 studies reported the VAS score, and 8 of 19 studies reported the ROM score and adverse events. The characteristics of the included studies are shown in Table 2. Furthermore, the network plot of comparisons are shown in Figure 2.
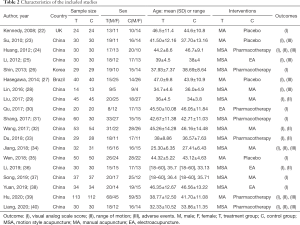
Full table

Methodological quality assessment
The risk of bias assessment of the 19 RCTs is presented in Figures 3 and 4. Fifteen studies were judged as low risk for random sequence generation, and one was judged as high risk because it was allocated in numerical order. Seven studies described the method of allocation concealment, which were judged as low risk. Four studies described double or single blinding, and these studies had low risk. All studies had a low risk of bias for incomplete outcome data for the missing data was few. Selective outcome reporting was unclear in all included studies, except for one study, which provided published protocols. Additionally, for the judgment of other risks, there was insufficient information to make correct assessments.
Pairwise meta-analyses
The results of pairwise meta-analyses are presented in Table 3. We generated 6 pairwise meta-analyses to compare the VAS score of different interventions. The VAS score of MA was significantly lower than that of placebo (SMD: −1.10; 95% CI, −1.59 to −0.61). VAS scores were significantly lower in MSA (MD: −1.21; 95% CI, −2.31 to −0.11) and MA (MD: −2.89; 95% CI, −3.35 to −2.43) than those in pharmacotherapy. Moreover, the VAS score of MSA was significantly lower than those of MA (SMD: −1.34; 95% CI, −2.11 to −0.56) and EA (MD: −1.07; 95% CI, −1.51 to −0.63). No significant difference between EA and pharmacotherapy were noted. In terms of ROM score, we performed 4 pairwise meta-analyses to compare different interventions. The ROM score of MSA was significantly lower than those of pharmacotherapy (SMD: −0.81; 95% CI, −1.12 to −0.50) and MA (MD: −0.58; 95% CI, −0.84 to −0.32). Furthermore, the ROM score of MA was significantly lower than that of pharmacotherapy (MD: −0.94; 95% CI, −1.20 to −0.68).
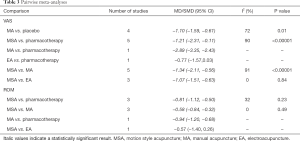
Full table
NMA
The results of NMA are presented in Figure 5. Data on VAS score were available from 19 RCTs, and the five reported arms were (I) MSA, (II) MA, (III) EA, (IV) pharmacotherapy, and (V) placebo. The MSA (SMD: −2.21; 95% CI, −3.33 to −1.08), MA (SMD: −1.14; 95% CI, −2.01 to −0.27) and EA (SMD: −1.57; 95% CI, −2.98 to −0.15) showed significantly better effects in reducing VAS score compared to placebo. Furthermore, the MSA was significantly more effective than MA (SMD: −1.06; 95% CI, −1.78 to −0.35) and pharmacotherapy (SMD: −1.17; 95% CI, −1.85 to −0.49) in reducing VAS score. Data on ROM score were available from 8 RCTs, and the four reported arms were (I) MSA, (II) MA, (III) EA, and (IV) pharmacotherapy. The MSA (SMD: −1.00; 95% CI, −1.47 to −0.54) and MA (SMD: −0.60; 95% CI, −1.15 to −0.05) showed significantly better effects in reducing ROM score compared to pharmacotherapy.
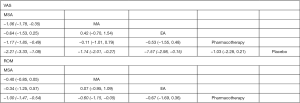
Ranking probability
The SUCRA-based rankings of all interventions are displayed in Figure 6. For the VAS score, MSA (98.0%) was the optimal intervention method, followed by EA (67.2%), MA (45.4%), pharmacotherapy (37.5%), and placebo (1.8%) which was ranked as the worst. For the ROM score, MSA (92.2%) was the best intervention, followed by EA (55.9%), MA (48.3%), and pharmacotherapy (3.6%) which was ranked as the worst. Based on the SUCRA values of intervention methods for VAS and ROM score, MSA appeared to be the best intervention method.

Safety
Eight studies reported adverse events, while no serious complications were observed in all included studies. Generally speaking, the major adverse effects of acupuncture therapy include fainting and haematoma formation. As most studies did not report the adverse events in a standard way, it was difficult to perform a quantitative analysis of adverse events in this review.
Inconsistency analyse
For the inconsistency test outcome of VAS score, it showed inconsistency between MSA and MA (P=0.02), and MA and pharmacotherapy (P=0.02). For the inconsistency test outcome of ROM score, it showed inconsistency between MSA and MA (P=0.006), MSA and pharmacotherapy (P=0.006), and MA and pharmacotherapy (P=0.006).
Publication bias and sensitivity analysis
Funnel plots revealed no evidence of publication bias (Appendix 2). Sensitivity analysis showed the result was robust (Appendix 3).
Discussion
ALBP is a common musculoskeletal disorder that seriously affects patients’ quality of life and imposes a substantial social and economic burden (6-8). Acupuncture is a widely used non-pharmacological therapy in China because of its advantages of easy operation, safety, and reliability, etc. (13-15). Many studies have proved the effectiveness and safety of Acupuncture in treating ALBP (13). However, no previous studies have clarified which type of acupuncture technique shows the most efficacy in ALBP treatment. Thus, this study systematically analyzed the results of previous studies with Bayesian NMA to compare the efficacy and safety of different acupuncture techniques in the treatment of ALBP.
In this study, 19 RCTs recruiting 1,427 participants were included in the analysis. The SUCRA-based rankings of the primary outcome shown that the MSA was the most effective in reducing VAS and ROM score. EA was better than MA in reducing VAS scores, but both acupuncture techniques showed comparable efficacy in reducing ROM score. Overall, we found that all acupuncture treatments (MSA, MA, and EA) are more effective in both alleviating pain and improving lumbar activity of ALBP patients compared with pharmacotherapy or placebo. This was consistent with the results of the previous systematic review (13-15). Concurring with previous systematic reviews on acupuncture safety (13-15,41), no severe adverse events associated with acupuncture therapy were reported among the included studies. Moreover, the inconsistency was assessed by the node-splitting method, which showed inconsistency between the direct and the indirect comparisons. The possible causes of the variation were as follows: Firstly, only one or two RCTs comparing the related interventions, small effect size of the trials, and the results of indirect comparison are stronger. Secondly, it is difficult to rule out heterogeneity among studies due to the differences in acupoints, clinicians’ experience, treatment frequency, and follow-up time used across studies. We speculate that the inconsistency might be attributed to heterogeneity among studies. In general, patients who did not respond well to conventional pharmacotherapy may consider acupuncture as an alternative. Nevertheless, it is difficult to determine which acupuncture therapy is the best considering the low quality of the original study. As a result, clinicians must consider the clinical conditions and patient's willingness when they make treatment decisions.
This study identified that MSA is the most effective treatment for ALBP, although its safety remained unclear. The MSA is a traditional acupuncture technique that has been recorded as a therapeutic modality for soft tissue injuries and musculoskeletal disorders in several ancient traditional Chinese medicine classics (26,28). MSA therapy requires active or passive movement of patients’ body in company with needling (26,28,42). It can maximize the synergistic therapeutic efficacy of acupuncture and exercise therapy. The mechanisms underlying the effects in pain relief and recovery of lumbar mobility in MSA therapy are not yet clear. However, according to previous studies, it may be related to acupuncture analgesia and cognitive shifts in pain perception. The mechanisms that MSA therapy enhances the effects of pain relief may be as follows. Firstly, acupuncture can increase the secretion of β-endorphin by stimulating the internal activity of the central nervous system (43,44). The increase in β-endorphin levels correlated with an increase in the pain threshold (44). Secondly, another possible mechanism is that acupuncture activates the diffuse noxious inhibitory control (DNIC), a descending system that modulates nociceptive neurons at the spinal cord level from top to bottom, resulting in pain alleviation (45,46). After acupuncture treatment, if patients feel less pain, then more mobility can be obtained. In the meantime, there is evidence that exercise therapy should be prescribed for the treatment of adults with ALBP to expedite recovery (47). Thus, MSA therapy could form a positive cycle leading to enhanced therapeutic efficacy.
However, this study has several limitations. First, due to poor reporting, most of the included RCTs were judged as having an unclear risk of bias in terms of allocation concealment, blinding, and selective outcome reporting. Methodologic limitations of the included RCTs may reduce the credibility of our conclusions to some extent. To improve the quality of evidence, future trials should follow the Consolidated Standards of Reporting Trials (CONSORT) guidelines (48) and Standards for Reporting Interventions in Controlled Trials of Acupuncture (STRICTA) checklists (49). Second, heterogeneity was difficult to rule out because of the differences in acupoints, clinicians’ experience, treatment frequency, and follow-up time used across studies. Third, Most of the included RCTs were implemented in China among Chinese populations, which may limit the generalization of our conclusions. Fourth, we failed to assess the safety of each acupuncture therapy due to a lack of standardization in the reporting of adverse events. Close monitoring and adequate reporting of adverse events need to be considered by future researchers in this field. The limitations above notwithstanding, this study comprehensively analyzed the efficacy of each acupuncture therapy for treating ALBP, which was quite fresh in a related study. To date, no studies have evaluated the efficacy of acupuncture therapy on ALBP based on NMA. The results of this study may provide a reference for the treatment of ALBP.
Conclusions
The findings of this comprehensive review indicate that acupuncture therapy achieved good therapeutic effects in the treatment of ALBP. Furthermore, MSA may be considered as an optimal treatment for ALBP. However, the low quality of the included studies limited the trustworthiness of the conclusion. Therefore, well-designed RCTs with high quality and large samples are still required to evaluate the efficacy and safety of acupuncture therapy for ALBP.
Acknowledgments
Funding: This work was supported by the National Natural Science Foundation of China (No. 81874478), the Hunan Provincial Natural Science Foundation of China (No. 2019JJ40224), and the Hunan Traditional Chinese Medicine Scientific Research Program (No. 2021002).
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at http://dx.doi.org/10.21037/apm-21-551
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-21-551). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Andersson GB. Epidemiological features of chronic low-back pain. Lancet 1999;354:581-85. [Crossref] [PubMed]
- Hoy D, Bain C, Williams G, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum 2012;64:2028-37. [Crossref] [PubMed]
- van Tulder M, Becker A, Bekkering T, et al. Chapter 3. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J 2006;15:S169-91. [Crossref] [PubMed]
- Chou R, Huffman LHAmerican Pain Society. American College of Physicians. Medications for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med 2007;147:505-14. [Crossref] [PubMed]
- Atlas SJ, Deyo RA. Evaluating and managing acute low back pain in the primary care setting. J Gen Intern Med 2001;16:120-31. [Crossref] [PubMed]
- Qaseem A, Wilt TJ, McLean RM, et al. Clinical Guidelines Committee of the American College of Physicians. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med 2017;166:514-30. [Crossref] [PubMed]
- Casazza BA. Diagnosis and treatment of acute low back pain. Am Fam Physician 2012;85:343-50. [PubMed]
- Martin BI, Turner JA, Mirza SK, et al. Trends in health care expenditures, utilization, and health status among US adults with spine problems, 1997-2006. Spine (Phila Pa 1976) 2009;34:2077-84. [Crossref] [PubMed]
- Chou R, Atlas SJ, Stanos SP, et al. Nonsurgical interventional therapies for low back pain: a review of the evidence for an American Pain Society clinical practice guideline. Spine (Phila Pa 1976) 2009;34:1078-93. [Crossref] [PubMed]
- Chou R, Huffman LHAmerican Pain Society. American College of Physicians. Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med 2007;147:492-504. [Crossref] [PubMed]
- Fan Y, Wu Y. Effect of electroacupuncture on muscle state and infrared thermogram changes in patients with acute lumbar muscle sprain. J Tradit Chin Med 2015;35:499-506. [Crossref] [PubMed]
- Kelly RB, Willis J. Acupuncture for Pain. Am Fam Physician 2019;100:89-96. [PubMed]
- Lee JH, Choi TY, Lee MS, et al. Acupuncture for acute low back pain: a systematic review. Clin J Pain 2013;29:172-85. [Crossref] [PubMed]
- Hu XJ. Systematic review of exercise acupuncture in the treatment of acute lumbar sprain. Chengdu University of Chinese Medicine 2015. Available online: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CMFD&dbname=CMFD201601&filename=1016042695.nh&v=4eYJgDomecVQQ5bqo1Wnm7Q%25mmd2BwAfRkkMymn6Ma6I5ABJ1hq%25mmd2Fy%25mmd2FKgIiAD8KhCrm%25mmd2FvS
- Li JL. Systematic review and META analysis of acupuncture treatment of acute lumbar sprain in recent 10 years. Beijing University of Chinese Medicine 2016. Available online: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CMFD&dbname=CMFD201602&filename=1016069055.nh&v=uUP2pp80ssi3JP%25mmd2F30m4oq6dVRasvexoq8idhlmJBf01RwHVdiWCU5qJ7m%25mmd2Biy8ryG
- Lee AW. Use of network meta-analysis in systematic reviews: a survey of authors. Syst Rev 2016;5:8. [Crossref] [PubMed]
- Catalá-López F, Tobías A, Cameron C, et al. Network meta-analysis for comparing treatment effects of multiple interventions: an introduction. Rheumatol Int 2014;34:1489-96. [Crossref] [PubMed]
- Higgins JP, Altman DG, Gøtzsche PCCochrane Bias Methods Group, et al. Cochrane Statistical Methods Group. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [Crossref] [PubMed]
- von Hippel PT. The heterogeneity statistic I(2) can be biased in small meta-analyses. BMC Med Res Methodol 2015;15:35. [Crossref] [PubMed]
- Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol 2011;64:163-71. [Crossref] [PubMed]
- Mbuagbaw L, Rochwerg B, Jaeschke R, et al. Approaches to interpreting and choosing the best treatments in network meta-analyses. Syst Rev 2017;6:79. [Crossref] [PubMed]
- Kennedy S, Baxter GD, Kerr DP, et al. Acupuncture for acute non-specific low back pain: a pilot randomised non-penetrating sham controlled trial. Complement Ther Med 2008;16:139-46. [Crossref] [PubMed]
- Su JT, Zhou QH, Li R, et al. Immediate analgesic effect of wrist-ankle acupuncture for acute lumbago: a randomized controlled trial. Zhongguo Zhen Jiu 2010;30:617-22. [PubMed]
- Huang JZ. Study on the clinical efficacy of Yao Tong Point acupuncture combined with exercise in treating acute lumbar sprain. Guangzhou University of Chinese Medicine 2012. Available online: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CMFD&dbname=CMFD2012&filename=1012396486.nh&v=JcefA1k%25mmd2Fng2pWRd%25mmd2BnfIm38WFnX8KdivOgUCN%25mmd2FnkRXQOIF%25mmd2FwBOb7DLbqC2zchtkAE
- Li B. Clinical Study of acute lumbar sprain treated with Balance acupuncture and exercise therapy. Guangzhou University of Chinese Medicine 2012. Available online: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CMFD&dbname=CMFD2012&filename=1012396427.nh&v=JcefA1k%25mmd2Fng21Oe53l7bYG1Sb7ifw1EJ6n8ImicrRHjpdGT%25mmd2B6pB%25mmd2FEMWtfgpM612H%25mmd2F
- Shin JS, Ha IH, Lee J, et al. Effects of motion style acupuncture treatment in acute low back pain patients with severe disability: a multicenter, randomized, controlled, comparative effectiveness trial. Pain 2013;154:1030-7. [Crossref] [PubMed]
- Hasegawa TM, Baptista AS, de Souza MC, et al. Acupuncture for acute non-specific low back pain: a randomised, controlled, double-blind, placebo trial. Acupunct Med 2014;32:109-15. [Crossref] [PubMed]
- Lin R, Zhu N, Liu J, et al. Acupuncture-movement therapy for acute lumbar sprain: a randomized controlled clinical trial. J Tradit Chin Med 2016;36:19-25. [Crossref] [PubMed]
- Liu Q, Li MX, Li DX, et al. Clinical Observations on the Effect of Acupuncture at Yingtang and Houxi Acupoint Combined with Exercise Therapy in Treating Acute Lumbar Sprain. Clinical Journal of Traditional Chinese Medicine 2017;29:127-9.
- Qu F, Guan HL, Luo YJ, et al. Clinical observation on treating acute lumbar muscle sprain by electropuncture. Clinical Journal of Chinese Medicine 2017;9:39-40.
- Shang LL, Liu K, Sun H, et al. Clinical Study on Distal-points Acupuncture Combined with Exercise for Acute Lumbar Sprain: Experiences from Professor SUN Yuan-zheng. Journal of Clinical Acupuncture and moxibustion 2017;33:38-40.
- Wang JH. Clinical observation of acupuncture combined with local exercise therapy in the treatment of acute lumbar sprain. Chinese Medicine Emergency 2017;26:1673-5.
- Du L. AnaIgesiatime-effects study of acupuncture at YaoTong Point combined with exercise therapy for acute lumbar sprain. Guangzhou University of Chinese Medicine 2018. Available online: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CMFD&dbname=CMFD202001&filename=1019097231.nh&v=PCxD3ISX6aUTS0lMvDd2DxYZOaFl8LiVvdsmguySlwBXMGQyHVxXmt9zDym9sAil
- Jiang LH. Clinical study of local shallow acupuncture combined with active exercise in the treatment of acute lumbar sprain. Nanjing University of Chinese Medicine 2018. Available online: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CDFD&dbname=CDFDLAST2018&filename=1018124582.nh&v=K8HEh4rzBBzSxQqJ%25mmd2FMUC67QAIw76Ib9z14ma3rjQ2hPJnOxBiloEAuN1%25mmd2FigTuwOc
- Wen X, Chen XJ, Liang JH, et al. Study on the immediate analgesic effect of the wrist and ankle acupuncture in treating acute lumbago. Journal of Electrocardiography (Electronic Edition) 2018;7:128-9.
- Li J. Clinical observation of balance needle combined with exercise therapy in the treatment of acute lumbar sprain. Modern Distance Education of Chinese Medicine 2019;17:79-81.
- Song JC. Clinical observation on the treatment of acute lumbar sprain with distal acupoint acupuncture. Chinese Modern Distance Education of Traditional Chinese Medicine 2019;17:91-2.
- Yuan J, Dou YX, Li MH.Clinical observation of the second metacarpal side holographic therapy combined with exercise therapy for acute low back pain. Massage and Rehabilitation Medicine 2019;10:16-17, 20.
- Hu ZP, Yang ZQ, Yong Wu, et al. Clinical randomized controlled study on the immediate effect of long needle penetration in the treatment of acute lumbar sprain. Chinese Medicine Emergency 2020;29:1788-90.
- Liang HS, Sheng D, Jiang RJ, et al. Effect analysis of acupuncture at Dong Shiqi point in the treatment of acute lumbar sprain. Chinese Medicine Emergency 2020;29:1944-6.
- Chan MWC, Wu XY, Wu JCY, et al. Safety of Acupuncture: Overview of Systematic Reviews. Sci Rep 2017;7:3369. [Crossref] [PubMed]
- He GX. Effect of movement on acupuncture analgesia and its clinical significance. Zhen Ci Yan Jiu 1982;10:1-8.
- Clement-Jones V, McLoughlin L, Tomlin S, et al. Increased beta-endorphin but not met-enkephalin levels in human cerebrospinal fluid after acupuncture for recurrent pain. Lancet 1980;2:946-9. [Crossref] [PubMed]
- Bodnar RJ, Nilaver G, Wallace MM, et al. Pain threshold changes in rats following central injection of beta-endorphin, met-enkephalin, vasopressin or oxytocin antisera. Int J Neurosci 1984;24:149-60. [Crossref] [PubMed]
- Le Bars D, Dickenson AH, Besson JM. Diffuse noxious inhibitory controls (DNIC). II. Lack of effect on non-convergent neurones, supraspinal involvement and theoretical implications. Pain 1979;6:305-27. [Crossref] [PubMed]
- Bing Z, Villanueva L, Le Bars D. Acupuncture and diffuse noxious inhibitory controls: naloxone-reversible depression of activities of trigeminal convergent neurons. Neuroscience 1990;37:809-18. [Crossref] [PubMed]
- McLain K, Powers C, Thayer P, et al. Effectiveness of exercise versus normal activity on acute low back pain: an integrative synthesis and meta-analysis. Online J Knowl Synth Nurs 1999;6:7. [Crossref] [PubMed]
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. J Pharmacol Pharmacother 2010;1:100-7. [Crossref] [PubMed]
- MacPherson H, Altman DG, Hammerschlag R, et al. Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): extending the CONSORT statement. Acupunct Med 2010;28:83-93. [Crossref] [PubMed]




