
Changes in local bone mineral density can guide the treatment plan for patients with rupture of the anterior cruciate ligament
Introduction
Anterior cruciate ligament (ACL) rupture is a common injury in sports medicine. With the development of minimally invasive concepts and continuous advancements in arthroscopic technology, arthroscopic ACL reconstruction has become the main treatment for this traumatic injury. Although the overall clinical results as well as patient reported outcome measurements (PROMs) after ACL reconstruction are generally good (1-3), some patients fail to achieve satisfactory results and may require a second revision surgery (4-6). Thus, increasing the success rate of ACL reconstruction surgery is a hot topic in sports medicine at home and abroad. At present, it is recognized that the factors that affect the outcomes of ACL reconstruction include the choice of graft (7-9), the choice of fixation mode (10-13), and the location of the bone tunnel (14-16). However, there have been few studies examining the effect of local bone conditions on the reconstruction of the ACL (17,18). Most of the relevant literature focuses on the changes in local BMD after the reconstruction of the ACL, rather than the influence of the rupture of ACL on the local BMD of the knee joint. Some patients with abnormal bone mass around the knee joint will experience screw splitting and pull-out during the surgery (19). Stener et al. (17) followed bone mineral density (BMD) changes in the calcaneus, hips, and lumbar spine after ACL reconstruction and found that both female and male patients had a significant decrease in BMD in both calcaneus and both hips during the 5-year study period. However, this latter study did not investigate the changes in BMD of the affected limbs before ACL reconstruction. Lee et al. (20) examined the bone density around the fixation area during the knee ligament reconstruction and showed that the anterior medial of the proximal tibia was most acceptable in the interference screw fixation and the posterior central area had the lowest bone density in the proximal tibia. Mariani et al. (18) showed a similar result by comparing the BMD of the proximal tibia in the area adjacent to the fixation of the posterior cruciate ligament (PCL) with the BMD in a similar area at the ideal site for ACL fixation. However, Järvinen and colleagues (21) reported that BMD did not provide a sufficiently accurate prediction of the fixation strength of an individual soft tissue ACL graft. Therefore, the changes in the local bone density of the affected knee after the ACL rupture are still controversial. At present, there are few reports on the treatment plan for ACL rupture according to the local bone condition of the knee joint. Since January 2017, patients in our hospital department with ACL ruptures have routinely received local BMD measurements in the affected knee to guide treatment planning. The observations of this study demonstrated that when fixation methods were selected according to the bone condition of the patients, satisfactory outcomes could be achieved. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/apm-21-741).
Methods
General information
From January 2017 to April 2019, 80 patients with ACL rupture who were treated surgically in our department were included in the study according to the inclusion criteria and exclusion criteria. The following inclusion criteria were applied (22): (I) patients with ACL rupture only (including meniscus tear), excluding posterior cruciate ligament and collateral ligament rupture; (II) patients with no history of knee joint trauma or surgery; and (III) patients with joint instability and a positive Lachman test or anterior drawer test. The following cases were excluded: (I) cases of primary osteoporosis (postmenopausal osteoporosis and senile osteoporosis); (II) cases where the contralateral calf had a previous fracture or ligament or severe meniscus injury; and (III) cases with bilateral knee joint injury. A total of 64 males and 16 females were enrolled in this study, with an average age of 27.68±6.13 years (range, 19–40 years). The time of injury ranged from 3 days to 12 months. There were 56 patients with an ACL rupture history of less than 3 months, of which 45 were males and 11 were females, and the average age was 27.70±7.47 years. There were 24 patients with an ACL rupture history of more than 3 months, including 19 males and 5 females, with an average age of 27.63±6.46 years. All patients presented with unilateral knee injury, with 27 cases on the left knee and 53 cases on the right knee. X-ray film, magnetic resonance imaging, and BMD were routinely measured in the bilateral knees prior to surgery. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committees of Wuxi Ninth People’s Hospital (No.: LW2020031) and informed consent was taken from all the patients.
Measure methods of BMD
While there is a standardized database reference for the BMD T value of the lumbar vertebrae and hip joint, there is no database comparison for the local BMD of the knee joint. Previous studies have shown no difference in the bone mass between the dominant and non-dominant sides in the lower extremities (23-25). Analysis of the local bone density of the knee joint for 20 healthy subjects showed similar results in the bilateral legs. Therefore, the design of this study assumed no difference in the local bone density of the knee joint between the dominant leg and the non-dominant leg of a healthy person. Thus, in the present investigation, the BMD (g/cm2) of the affected knee joint was compared to that of the healthy knee joint (26) and the results were statistically analyzed using paired T-tests.
BMD was measured using the American Norland XR-36 dual energy X-ray absorptiometry (DEXA) and a custom-made knee-scanner. DEXA has been shown to record BMD changes caused by different treatments, and to confirm the diagnosis of osteoporosis (27). The scanner has a built-in software facility that can automatically adjust the scanning speed according to the source decay to ensure reproducible counting statistics. During the scan, the knees were extended, and the feet remained upright. The imaging resolution of the bone densitometer is 0.4 mm, the bone mineral density repetition accuracy is less than 1%, the pixel matrix is 512×512, and the scanning time is 5 min. The scanning range was from suprapatellar 5 cm to subtibial plateau 5 cm. All BMD measurements were performed by an expert nurse in the hospital osteoporosis clinic. The specific measurement methods and parameter settings have been detailed in Petersen et al. (28). BMD is expressed in grams per centimeter square (g/cm2) and calculated with the software.
Surgical methods
Selection of operative methods
Several studies have confirmed good consistency between the BMD values of the left and right limbs. Oh et al. (29) enrolled 65 patients with a unilateral rotator cuff tear and computed tomography scans of the bilateral proximal humerus were performed. Region-specific BMD was measured in the proximal humerus. The results showed that the volumetric BMD values in the region of the center sphere block of the humeral head decreased to 70% of that in the asymptomatic contralateral shoulder (41.2±44.2 vs. 58.4±60.1 mg/cm3). Similarly, in Krappinger’s study (30), the local BMD of patients with proximal humerus fractures was assessed. Patients from the fracture group had a 70% lower BMD compared to patient in the control group (95.9±28.6 vs. 132.8±34.7 mg/cm3).
In keeping with the literature, patients in this current study were divided into the following groups according to the degree of decrease in local BMD pre-surgery: the density of the affected knee was not significantly lower than that of the healthy side (“normal” BMD group); the local BMD of the affected knee was lower than 70% of the healthy side (“low” BMD group); and the local BMD of the affected knee decreased but not below 70% of the healthy side (“decreased” BMD group). For patients with normal BMD, extrusion fixation should be selected. In patients whose local BMD is lower than 70% of the healthy side, suspension fixation should be applied. For patients whose local BMD of the affected knee is decreased but not lower than 70% of the healthy side, extrusion fixation is preferred. If tunnel cutting or screw splitting and tunnel enlargement or screw pull-out occurred during the surgery, the fixation mode was adjusted in real-time according to the situation (Figure 1).

Extrusion fixation method
After successful anesthesia, the patient was placed in the supine position, and the affected limb was placed in the 90° flexion position. Routine disinfection and towel laying were performed. An anterior medial L-shaped incision was made under the tibial tubercle of the knee, the semitendinosus tendon and the gracilis tendon were cut, the muscle was removed, and the tendon line was woven at both ends. At the level of the knee joint space, an opening of 8 mm was made on both sides of the patellar ligament to the articular cavity, which was disposed into the arthroscope from the lateral entrance. Additionally, the intercondylar fossa was cleared, and the scar tissue and residual ACL were removed. The tibial end of the ACL was located with a guide needle, and the tibia of the corresponding diameter was drilled to open the tibial tunnel. The femoral footprint of the ACL was then located using a guide needle, and the femur drill was used to open the femoral tunnel by approximately 35 mm. The braided tendon was introduced with the guide needle, and the knee was flexed by 20°. Reverse traction was implemented at both ends of the femur and tibia to maintain a certain tension, and passive movement of the affected knee was carried out to provide appropriate tension of the tendon. The femoral tunnel was fixed with a 25-mm long polylactic acid hydroxyapatite screw. The tibial tunnel was fixed with a tibial fixation wing and a 25-mm long polyetheretherketone screw (Smith & Nephew Inc.). The knee was moved passively, and the anterior drawer test was performed. If the knee joint was stable and the autologous tendon tension was moderate, then suturing and pressure bandaging were performed. If screw splitting or tendon cutting occurred during the surgery, the mode of fixation was adjusted to suspension fixation. If the tunnel was enlarged or screws were pulled out due to osteoporosis during the surgery, adjustment to suspension fixation would be carried out. Alternatively, on the basis of extrusion fixation, a loop steel plate was added to the outer entrance of the tunnel to carry out suspension fixation. If the tunnel was obviously enlarged, artificial bone grafting may be required (31,32).
Suspension fixation method
In the suspension fixation method, harvesting the transplanted tendon and cleaning the joint cavity were performed as described for the extrusion fixation method. After the joint cavity was cleaned, the guide needle was used to locate the tibial attachment of the ACL, and the tibia was drilled to expand the tibial tunnel. The femoral footprint of the ACL was then located, and the femur was drilled and enlarged by approximately 35 mm in a long tunnel. The guide needle was introduced into the autologous tendon, which was pulled at both ends of the tunnel to provide a certain tension, passive movement of the affected knee was carried out, providing the autologous tendon with the appropriate tension. A plate with a loop (Smith & Nephew Inc.) was used, the loop was cut, the tendon traction line was passed through both plate holes outside the thigh, and the plate was pushed forward to ensure the plate was adhered to the femoral cortex. Multiple knots were made on the surface of the plate to ensure the plate was firmly stuck at the outer entrance of the femoral tunnel to achieve suspension fixation. The outer entrance of the tibial tunnel was also suspended and fixed with a plate with a loop. The affected knee was moved passively again, and the anterior drawer test was performed. If the knee was stable and the tension of the transplanted tendon was moderate, the knee was sutured and bandaged under pressure.
Postoperative management
Post-surgery, the patients were transferred to the rehabilitation department for rehabilitation treatment. Treatments aimed at complete passive extension and quadriceps function started on the first day after ACL reconstruction. Active and passive range-of-motion exercises (including quadricep sets, prone hangs, active straight leg raises, and heel slides), and effusion management by adjustment of loading were supported. Cryotherapy was used to relieve pain. As a supplement to active exercise, high-intensity neuromuscular electrical stimulation (NMES) was efficacious in improving quadricep strength. After surgery, weight-bearing and non-weight-bearing exercises were recommended according to evidence-based guidelines (33).
Postoperative follow- up and evaluation of the curative effect
Patients were followed up at 1, 2, 3, 6, and 12 months post-surgery. Two sports medicine physicians who did not participate in this study were responsible for the follow-up. All patients were examined by the anterior drawer test, Lachman test, and pivot-shift test. The range of motion of the knee joint was measured. Patients with suspension fixation were re-examined by X-ray. Patients with extrusion fixation did not require X-rays as the screw was not visible. The function of the knee joint was evaluated by the IKDC (International Knee Documentation Committee) scale score (34) and the Lysholm knee joint scale score (35).
Statistical analysis
All data were analyzed using IBM SPSS 19.0 software (IBM Corp., Armonk, NY, USA). Measurement data are expressed as the mean ± standard deviation. Paired t-tests were used to compare the BMD of the bilateral knee joints and the functional score of the affected knee before and after the surgery. Group t-tests were used to compare the decreasing degree of BMD in patients with an ACL history less than 3 months and patients with an ACL history greater than 3 months. P<0.05 was considered statistically significant.
Results
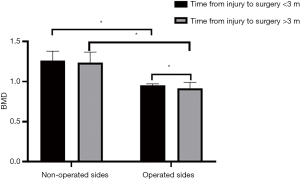
There was no significant difference in age or gender between patients with a history of less than 3 months and those with a history of more than 3 months. The local BMD measurements of the knee joints in 80 patients showed that 68 patients had varying degrees of bone mass loss relative to the healthy side. The average BMD of the affected knee was significantly less than that of the contralateral knee joint (0.927±0.283 vs. 1.256±0.153 g/cm2; P<0.01; Table 1). The decrease in local BMD of the affected knee was less than 70% of the contralateral value in 28 patients and greater than 70% of the contralateral value in 40 patients. The BMD of the affected knee in patients with a history of more than 3 months was significantly lower than that observed in patients with a history of less than 3 months (0.914±0.076 vs. 0.956±0.017 g/cm2; P<0.01; Table 2), suggesting that the longer the time after injury, the more significant the decrease in BMD (Figure 2).

Full table
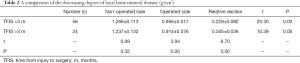
Full table
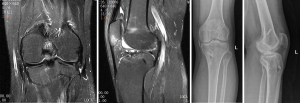
All patients were followed up for 12 to 30 months (mean follow-up period of 20.65±5.12 months). During the last follow-up, symptoms of knee instability were not detected in any of the patients and only 5 patients complained of mild knee pain. Physical examination showed that the anterior drawer tests, Lachman tests, and pivot-shift tests were all negative. All patients displayed a normal range of motion of the knee joint. At the last follow-up, the IKDC score and the Lysholm knee score of the affected knee were 89.17±3.28 and 89.67±2.97, respectively. Both scores were significantly higher than that observed pre-surgery (P<0.01; Table 3). In all patients, the muscle function of the knee joints returned to normal. In the “normal” BMD group, tunnel enlargement and screw pull-out occurred in 2 patients, and screw splitting occurred in 1 patient. Among them, the patients with screw splitting and tunnel enlargement were adjusted to suspension fixation in real-time during the surgery, and the other patient with tunnel enlargement was fixed by suspension with a plate with a loop on the basis of extrusion fixation (Figure 3). All 3 patients recovered well after follow up.

Full table
Discussion
The ACL is a statically stable structure that plays an important role in the stability of the knee joint. Once injured, it is difficult to heal and can even lead to progressive meniscus and articular cartilage wear, and thus it is usually necessary to reconstruct the ligament under arthroscopy. However, even with the high success rate of surgery, there are still thousands of patients undergoing revision surgery every year in China. The common causes of graft failure include poor location of bone tunnel, graft re-injury and biological factors. There are many biological factors that can affect graft healing, and local bone condition is one of them. The severe symptoms caused by the rupture of the ACL often lead to the loss of motor function of the affected limbs. It leads to severe atrophy of the muscles around the knee joint, especially of the quadriceps femoris, and at the same time, the local BMD decreases accordingly. ACL attachment fixation is the most important link in reconstruction surgery (36), and most reconstruction failures are caused by unstable attachment fixation (20). Vopat et al. (37) suggested that the failure of ACL reconstruction often occurs on the fixed side, not on the transplanted tendon itself. It was suggested that reliable postoperative immediate stability could be obtained by interface screw extrusion. Additionally, the operation of interface screw fixation is relatively simple, provided it is screwed into the tunnel along the guide needle. Therefore, in the past, when dealing with this kind of injury, our department would proceed with the method of extrusion fixation with good results. However, with the increase in the number of surgical cases, we observed that very few patients had symptoms of ligament relaxation and joint instability after surgery, especially in elderly women and patients with old injuries. Therefore, we inferred that the local bone mass of the affected knee decreased due to postmenopausal osteoporosis and disuse bone atrophy, thus reducing the holding force of the screw (38,39). And it has been reported that local BMD will further decrease due to external fixation after ACL reconstruction, and some BMD declines are even permanent. Coupled with the decrease of BMD before operation, it should be inferred that the total BMD can drop by more than 30%. Therefore, starting from January 2017, we routinely measured the local BMD of the bilateral knees and performed X-rays of the affected knee in patients with ACL rupture before surgery. The bone mass of the affected knee would be evaluated and the ACL attachment fixation method would be selected according to the decreasing degree of BMD. This method has achieved good results.
For ACL rupture, the common attachment fixation methods in our department include extrusion fixation and suspension fixation (40). For suspension fixation with plates, it was previously believed that because it was far away from the normal ACL anatomical attachment, the longitudinal movement between the autogenous tendon and the bone canal could produce a “bungee jump” effect, and the transverse movement could produce a “wiper” effect, which can lead to enlargement of the bone tunnel, and synovial fluid immersion would also affect the tendon-bone healing process. However, through interface screw extrusion fixation, we can operate under direct vision, according to hand feel and mirror observation, and this method is more solid and reliable. The polylactide hydroxyapatite screw does not need to be removed for the second time and does not affect the magnetic resonance examination. Therefore, in general, the extrusion fixation method was preferred. However, extrusion fixation is not an omnipotent fixation method, and its indication and curative effects are closely related to the local bone mass of the affected knee. Since we must drill holes in the femur and tibia to form a tunnel in the extrusion fixation method, and then fix the graft in the tunnel at both ends of the femur and tibia, obviously, the bone density of the femur and tibia will affect the fixation quality of the graft. Decreased bone density will delay the tendon-bone healing. If this factor is not considered, and the time of external fixation is not extended accordingly, the graft may fall off or loosen during the movement of the knee joint, which will affect the outcomes of the surgery. Through previous surgical observations, we noted that some patients suffered from screw splitting and that the transplanted tendon was cut by the edge of the bone tunnel when squeezing the screw. In addition, some patients experienced screw loosening or even pull-out and bone tunnel enlargement when the knee was passively moved during the surgery (41). Therefore, there are still some limitations in extrusion fixation. During the surgery, if an adverse event occurs during extrusion fixation, immediate adjustment to the suspension fixation mode should be performed. When the plate with a loop is used for suspension fixation, the attachment crosses the outer entrance of the bone tunnel, and there is no need to consider the effect of bone mass, and therefore, it can be used for patients with osteoporosis and osteosclerosis. The force provided by suspension fixation and the contractile force of the transplanted tendon belong to a pair of acting forces and reaction forces, which are kept in a straight line in the opposite direction and have a strong anti-pull-out ability. The stress is concentrated between the plate and the outer entrance of the tunnel, and the suspension force is positively correlated with the contact area between them.
The rupture of ACL can lead to the decrease in local BMD around it, and the degree of decrease is highly correlated with gender, age, location and time after injury. The bone density of the expected ACL femoral canal and tibial canal is uniformly decreased. Especially after ACL reconstruction, the bone density around the knee decreased more obviously. The decrease of BMD is not conducive to the healing of the graft and the bone tunnel, which directly affects the effect of the operation. For some patients, especially those with old ACL rupture (course of disease >3 months), firm fixation with screws is usually difficult due to localized osteoporosis. Flexion and extension of the affected knee several times during the surgery can lead to screw loosening and tendon relaxation and as a result, suspension fixation must be used for replacement. Thus, it is imperative that the preoperative equipment is fully prepared such that the fixation mode can be adjusted in a timely manner.
Preoperative BMD examination, combined with X-ray images, can assist doctors to understand the bone mass around the knee joint and guide the preoperative preparation and selection of the type of graft fixation. If the local BMD of the patient is different, the appropriate individual fixation method can be adopted accordingly. For patients with old injuries, it is common to see severe osteoporosis in the affected knee due to long-term lack of exercise. Preoperative preparation for these patients may include functional exercises in the outpatient clinic and anti-osteoporosis treatment with drugs prior to reconstructive surgery, thereby reducing the risk of extrusion fixation failure. If the preoperative preparations do not improve the osteoporosis of the patient and the local BMD of the affected knee remains less than 70% of the contralateral value, ACL reconstruction can still be performed by suspension fixation. However, the time of external fixation must be extended appropriately to ensure a curative effect.
The degree of BMD decrease that is suitable for each fixation method still requires further evaluation with more clinical data. There are some limitations to this current investigation. First, this was not a randomized controlled study, and the intraoperative fixation method was changed according to the patient situation. Second, only 80 patients were included in the study. Future large-scale studies should be conducted to increase the statistical significance of this data. Third, this study relied on the clinical experience of the medical staff and this may have caused a degree of variability. According to the clinical experiences in our hospital department in recent years, we suggest that for patients with normal bone density, extrusion fixation should be selected. Suspension fixation should be used for patients whose local BMD is lower than 70% of the healthy side. For patients whose local BMD of the affected knee is decreased but not lower than 70% of the healthy side, extrusion fixation is preferred. We recommend that ACL reconstruction should be carried out within 3 months after injury to avoid a further decrease in the bone mass of the affected knee and to avoid affecting the outcomes of fixation. Inevitably, even with the above criteria, there will still be surgical failures in individual patients. Therefore, it is imperative to consider a holistic surgical plan for each individual patient and consider factors such as the age, gender, past history, and injury time. This will help to maximize the effectiveness of the surgery.
Conclusions
This research confirms that measurement of local BMD before surgery is of guiding significance for the selection of the type of graft fixation to be used in ACL reconstruction surgery. It is recommended that the reconstruction of the ACL should be performed within 3 months after the injury to avoid further decreases in the bone mass. When the BMD of the affected knee decreases significantly to below 70% of the healthy side, suspension fixation is more suitable. It should be noted that local BMD is just one of many factors that affect the outcomes of ACL reconstruction. Thus for each patient, it is necessary to consider the overall situation when making the surgical plan so as to achieve the most favorable outcome.
Acknowledgments
Funding: The project was supported by the Research Fundation of Wuxi Ninth People’s Hospital (No. 20184709).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist Available at http://dx.doi.org/10.21037/apm-21-741
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-21-741
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-21-741). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committees of Wuxi Ninth People’s Hospital (No.: LW2020031) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ahmad SS, Schreiner AJ, Hirschmann MT, et al. Dynamic intraligamentary stabilization for ACL repair: a systematic review. Knee Surg Sports Traumatol Arthrosc 2019;27:13-20. [Crossref] [PubMed]
- Yoo YS, Song SY, Yang CJ, et al. A Comparison between Clinical Results of Selective Bundle and Double Bundle Anterior Cruciate Ligament Reconstruction. Yonsei Med J 2016;57:1199-208. [Crossref] [PubMed]
- Ahmad SS, Schürholz K, Liechti EF, et al. Seventy percent long-term survival of the repaired ACL after dynamic intraligamentary stabilization. Knee Surg Sports Traumatol Arthrosc 2020;28:594-8. [Crossref] [PubMed]
- Cheatham SA, Johnson DL. Anatomic revision ACL reconstruction. Sports Med Arthrosc Rev 2010;18:33-9. [Crossref] [PubMed]
- Grassi A, Kim C, Marcheggiani Muccioli GM, et al. What Is the Mid-term Failure Rate of Revision ACL Reconstruction? A Systematic Review. Clin Orthop Relat Res 2017;475:2484-99. [Crossref] [PubMed]
- Magnussen RA, Meschbach NT, Kaeding CC, et al. ACL Graft and Contralateral ACL Tear Risk within Ten Years Following Reconstruction: A Systematic Review. JBJS Rev 2015;3:01874474-201501000-00002.
- Kang RW, Strauss EJ, Barker JU, et al. Effect of donor age on bone mineral density in irradiated bone-patellar tendon-bone allografts of the anterior cruciate ligament. Am J Sports Med 2011;39:380-3. [Crossref] [PubMed]
- Lansdown DA, Riff AJ, Meadows M, et al. What Factors Influence the Biomechanical Properties of Allograft Tissue for ACL Reconstruction? A Systematic Review. Clin Orthop Relat Res 2017;475:2412-26. [Crossref] [PubMed]
- Mouarbes D, Menetrey J, Marot V, et al. Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis of Outcomes for Quadriceps Tendon Autograft Versus Bone-Patellar Tendon-Bone and Hamstring-Tendon Autografts. Am J Sports Med 2019;47:3531-40. [Crossref] [PubMed]
- Ayzenberg M, Arango D, Gershkovich GE, et al. Pullout strength of a novel hybrid fixation technique (Tape Locking Screw™) in soft-tissue ACL reconstruction: A biomechanical study in human and porcine bone. Orthop Traumatol Surg Res 2017;103:591-5. [Crossref] [PubMed]
- Ettinger M, Karkosch R, Horstmann H, et al. Biomechanical properties of adjustable extracortical graft fixations in ACL reconstruction. J Exp Orthop 2018;5:41. [Crossref] [PubMed]
- Ettinger M, Werner-Lebeda T, Calliess T, et al. Femoral interference screw fixation of hamstring and quadriceps tendons for ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 2017;25:1241-8. [Crossref] [PubMed]
- Gaines EB, Lau D, Naziri Q, et al. A biomechanical analysis of tibial ACL reconstruction with graft length mismatch. J Orthop Surg (Hong Kong) 2017;25:2309499017690983 [Crossref] [PubMed]
- Okazaki K, Matsubara H, Osaki K, et al. Femoral tunnel apertures on the lateral cortex in anterior cruciate ligament reconstruction: an analysis of cortical button fixation. Arthroscopy 2014;30:841-8. [Crossref] [PubMed]
- Suomalainen P, Moisala AS, Paakkala A, et al. Comparison of tunnel placements and clinical results of single-bundle anterior cruciate ligament reconstruction before and after starting the use of double-bundle technique. Knee Surg Sports Traumatol Arthrosc 2013;21:646-53. [Crossref] [PubMed]
- Varady NH, Kernkamp WA, Li J, et al. The biomechanical effect of tunnel placement on ACL graft forces in double-bundle ACL reconstruction - A 3D computational simulation. Int J Med Robot 2017; [Crossref] [PubMed]
- Stener S, Kartus J, Ejerhed L. Anterior cruciate ligament reconstruction reduces bone mineral areal mass. Arthroscopy 2013;29:1788-95. [Crossref] [PubMed]
- Mariani PP, Margheritini F, Bellelli A. Bone mineral density of the proximal metaphysis of tibia: clinical relevance in posterior cruciate ligament reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy 2005;13:263-7. [Crossref] [PubMed]
- Balci A, Gezer NS, Tatari MH, et al. Measurement of regional trabecular bone attenuation of the knee following anterior cruciate ligament rupture. Arch Orthop Trauma Surg 2016;136:1453-7. [Crossref] [PubMed]
- Lee YS, Nam SW, Hwang CH, et al. Computed tomography based evaluation of the bone mineral density around the fixation area during knee ligament reconstructions: clinical relevance in the choice of fixation method. Knee 2012;19:793-6. [Crossref] [PubMed]
- Järvinen TL, Nurmi JT, Sievänen H. Bone density and insertion torque as predictors of anterior cruciate ligament graft fixation strength. Am J Sports Med 2004;32:1421-9. [Crossref] [PubMed]
- Månsson O, Sernert N, Ejerhed L, et al. Long-Term Examination of Bone Mineral Density in the Calcanei After Anterior Cruciate Ligament Reconstruction in Adolescents and Matched Adult Controls. Arthroscopy 2016;32:615-23. [Crossref] [PubMed]
- Gomez-Bruton A, Gonzalez-Aguero A, Matute-Llorente A, et al. The muscle-bone unit in adolescent swimmers. Osteoporos Int 2019;30:1079-88. [Crossref] [PubMed]
- Lekamwasam S, Rodrigo M, de Silva KI, et al. Comparison of phalangeal bone mineral content and density between the dominant and non-dominant sides. Ceylon Med J 2005;50:149-51. [Crossref] [PubMed]
- van Santen JA, Pereira C, Sanchez-Santos MT, et al. Dominant vs. non-dominant hip comparison in bone mineral density in young sporting athletes. Arch Osteoporos 2019;14:54. [Crossref] [PubMed]
- van Meer BL, Waarsing JH, van Eijsden WA, et al. Bone mineral density changes in the knee following anterior cruciate ligament rupture. Osteoarthritis Cartilage 2014;22:154-61. [Crossref] [PubMed]
- Morgan SL, Prater GL. Quality in dual-energy X-ray absorptiometry scans. Bone 2017;104:13-28. [Crossref] [PubMed]
- Petersen MM, Olsen C, Lauritzen JB, et al. Late changes in bone mineral density of the proximal tibia following total or partial medial meniscectomy. A randomized study. J Orthop Res 1996;14:16-21. [Crossref] [PubMed]
- Oh JH, Song BW, Lee YS. Measurement of volumetric bone mineral density in proximal humerus using quantitative computed tomography in patients with unilateral rotator cuff tear. J Shoulder Elbow Surg 2014;23:993-1002. [Crossref] [PubMed]
- Krappinger D, Roth T, Gschwentner M, et al. Preoperative assessment of the cancellous bone mineral density of the proximal humerus using CT data. Skeletal Radiol 2012;41:299-304. [Crossref] [PubMed]
- Uchida R, Toritsuka Y, Mae T, et al. Healing of tibial bone tunnels after bone grafting for staged revision anterior cruciate ligament surgery: A prospective computed tomography analysis. Knee 2016;23:830-6. [Crossref] [PubMed]
- Zong JC, Ma R, Wang H, et al. The Effect of Graft Pretensioning on Bone Tunnel Diameter and Bone Formation After Anterior Cruciate Ligament Reconstruction in a Rat Model: Evaluation With Micro-Computed Tomography. Am J Sports Med 2017;45:1349-58. [Crossref] [PubMed]
- Filbay SR, Grindem H. Evidence-based recommendations for the management of anterior cruciate ligament (ACL) rupture. Best Pract Res Clin Rheumatol 2019;33:33-47. [Crossref] [PubMed]
- Collins NJ, Misra D, Felson DT, et al. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res (Hoboken) 2011;63:S208-28. [Crossref] [PubMed]
- Celik D, Coşkunsu D, Kiliçoğlu O. Translation and cultural adaptation of the Turkish Lysholm knee scale: ease of use, validity, and reliability. Clin Orthop Relat Res 2013;471:2602-10. [Crossref] [PubMed]
- Tie K, Wang H, Wang X, et al. Measurement of bone mineral density in the tunnel regions for anterior cruciate ligament reconstruction by dual-energy X-ray absorptiometry, computed tomography scan, and the immersion technique based on Archimedes' principle. Arthroscopy 2012;28:1464-71. [Crossref] [PubMed]
- Vopat B, Paller D, Machan JT, et al. Effectiveness of low-profile supplemental fixation in anterior cruciate ligament reconstructions with decreased bone mineral density. Arthroscopy 2013;29:1540-5. [Crossref] [PubMed]
- Domnick C, Herbort M, Raschke MJ, et al. Anterior Cruciate Ligament Soft Tissue Graft Fixation in the Elderly: Is There a Reason to Use Interference Screws? A Human Cadaver Study. Arthroscopy 2017;33:1694-700. [Crossref] [PubMed]
- Mündermann A, Payer N, Felmet G, et al. Comparison of volumetric bone mineral density in the operated and contralateral knee after anterior cruciate ligament and reconstruction: A 1-year follow-up study using peripheral quantitative computed tomography. J Orthop Res 2015;33:1804-10. [Crossref] [PubMed]
- Meller R, Neddermann A, Willbold E, et al. The relation between tunnel widening and bone mineral density after anterior cruciate ligament reconstruction: an experimental study in sheep. Arthroscopy 2010;26:481-7. [Crossref] [PubMed]
- Germann M, Snedeker JG, Stalder M, et al. Incorporating BMP-2 and skeletal muscle to a semitendinosus autograft in an oversized tunnel yields robust bone tunnel ossification in rabbits: Toward single-step revision of failed anterior cruciate ligament reconstruction. Knee 2018;25:765-73. [Crossref] [PubMed]
(English Language Editor: J. Teoh)


