
Comparison of therapeutic efficacy of three methods to prevent re-adhesion after hysteroscopic intrauterine adhesion separation: a parallel, randomized and single-center trial
Introduction
Background
Intrauterine adhesions (IUA) are also known as Asherman syndrome, stemming from Asherman’s systematic description of a series of symptoms of in 1948. IUA usually begins with endometrial damage which may be caused by various factors, and may result in fibrosis, leading to IUA occlusion and clinical symptoms, in which menstrual reduction and secondary infertility are the most common symptoms. Other symptoms include amenorrhea, periodical lower abdominal pain in women of childbearing age, and postmenopausal lower abdominal pain (1,2). Factors that induce IUA include uterine procedures (such as uterine curettage, cesarean section, and myomectomy), genital tract infections (such as bacterial vaginitis and mycoplasma infection), and genital tract malformations (including uterine mediastinum) (3). Sanders (4) studies on patients with IUA showed that intrauterine manipulation is a major factor in their pathogenesis, and the increased numbers of induced abortions in recent times has contributed to a rise in IUA cases. In a word, intrauterine adhesions are mostly caused by the fibrotic regeneration of the endometrium after severe damage.
The focus of current research is on determining measures to restore the structure and volume of the uterine cavity, prevent uterine wall adhesions, and relieve the clinical symptoms of patients, as measures to improve the reproductive function of women of childbearing age. With the development of minimally invasive technology, hysteroscopy has become the latest instrument for the accurate diagnosis of IUA, although other auxiliary examination methods, such as B-ultrasound and MRI, can improve the detection rate of IUA bands (5). However, the lack of clear vision of hysteroscopy contributes little to the comprehensive AFS score and further treatment after the detection of IUA. According to Dean et al., research on current therapies for IUA focuses on five areas: (I) surgical treatments, such as TCRA under hysteroscopy; (II) prevention of re-adhesion, involving physical interventions such as intrauterine balloon, intrauterine device (IUD), and biological interventions including sodium hyaluronate and amniotic membrane; (III) promotion of endometrial regeneration, including estrogen and progesterone therapy, stem cells and Chinese traditional medicine to induce endometrial regeneration; (IV) anti-inflammatory treatment; (V) postoperative reassessment of TCRA, including non-invasive methods such as MRI and B-ultrasound examination and intrusive methods such as hysteroscopy.
The current preferred treatment for IUA in China is TCRA, which has revolutionized the field. The separation of adhesions can be realized by electrotomy separation and scissors separation (6), and to prevent uterine perforation and improve the chance of successful surgery, B-ultrasound or laparoscopy can be used for monitoring (7). The specific surgical method involves intraoperative layer by layer separation, which begins with the separation of loose tissue, the uterine cavity is then enlarged, and dense tissue such as scars are removed. This provides the opportunity to repair the region from the fundus to the midline of the uterus and then to the lateral wall of the adhered uterine cavity. TCRA has the contradictory characteristics of a high success rate and high recurrence rate. It has even been reported that the recurrence rate of severe adhesions can be as high as 48–62.5%, while the pregnancy rate is as low as 22.5–33.3% (8). Therefore, it is crucial to prevent re-adhesion and increase the chance of pregnancy after surgery. Chinese government has promoted the use of IUDs since 1959. According to the statistics in 2002, almost 50% married women of childbearing age in China choose IUD to prevent pregnancy. The use rate of IUD has been declining in the past decade, but it is still widely used (9). We conducted a systematic review of the available literature, found no current accurate use rate of IUD. While at present, IUDs and intrauterine balloons are widely used, these come in many forms, and their use is still controversial, with no clear consensus on which is best (10,11). General opinion supports a balloon indwelling time of 5–7 days, while endometrial recovery after TCRA takes at least one month (12), and the mean time to fertilization after TCRA is 9.7±3.7 months. Further, as the severity of IUA increases, the fertilization rate decreases (13).
Foreign research on IUA has largely focused on the following aspects: (I) searching for a new classification system for IUA (14,15); (II) stem cell transplantation, where scholars expect to isolate endometrial stem cells to promote endometrial regeneration by extracting menstrual blood and umbilical cord blood stem cells (16); (III) new adjuvant methods combined with balloon therapy. Cai et al. investigated the effectiveness of an oxidative regenerative cellulose adhesion barrier plus an IUD (17); (IV) new intrauterine stents. Huang et al. established a new type of intrauterine stent with the expectation of finding a replacement for previous versions (18); (V) studies on the mechanism of IUA. Wu studied the signaling pathway of related factors in IUA (19).
Clinically, IUA is the type of disease which has great influence on the quality of life and reproduction of patients. The recurrence rate after surgery was as high as 62.5% (20), and while there are many factors affecting re-adhesion, the mechanism is still unclear. Present, research on the prevention of IUA is mainly retrospective, there are relatively few experimental studies, and due to the lack of an effective classification system for the evaluation of IUA, the evaluation of its efficacy is inconsistent. As new effective measures to prevent re-adhesion are mainly studied in animal experiments for ethical reasons (21), the prevention and treatment of IUA and re-adhesions is still a problem that scientists need to solve together.
Objectives
In attempt to evaluate the efficacy of an integrated approach to prevent and treat the recurrence of intrauterine adhesions (IUA) after hysteroscopic adhesiolysis, we conducted a parallel, randomized and single-center clinical trial. It was also expected to investigate the infection status and pregnancy rate of infertile women with intrauterine adhesions.
In the present study, 96 patients with moderate and severe IUA were evaluated in the Nantong Maternal and Child Health Hospital. Patients with different degrees of adhesion were divided into 3 groups, and the efficacy and safety of three different methods to prevent re-adhesion were discussed, focusing on the following: (I) Evaluation of the effect of intrauterine balloons combined with IUD and IUD alone in preventing re-adhesion. (II) Whether prolongation of intrauterine Foley balloon placement could improve postoperative intrauterine re-adhesion in patients with moderate and severe IUA, and its effect on menstruation and pregnancy rates. Our hypothesis is that intrauterine balloon plus IUD may be better in preventing IUA recurrence, and that the prolongation of balloon may achieve better therapeutic effect.
We present the following article in accordance with the CONSORT reporting checklist (available at https://dx.doi.org/10.21037/apm-21-1296).
Methods
Experimental design and ethics
This is a parallel, randomized and single-center clinical trial with 1:1:1 allocation ratio of three therapies (trial protocol at https://dx.doi.org/10.21037/apm-21-1296). From January 2016 to December 2019, IUA patients in the Nantong Maternal and Child Health Hospital were evaluated. Patients with moderate and severe IUA (48 cases in each degree) were selected and admitted for TCRA treatment, then randomly divided into three groups, respectively (Figure 1). The sequence of simple randomization was generated through a computer random number generation and maintained by a doctor who was not involved in patient registry. No investigator had access to the sequence. Opaque sealed envelopes were used to store the documents and were opened before the surgery by gynecologists. Group A (IUD, n=16) received IUD implantation immediately post TCRA and the IUD was removed 3 months after operation. In Group B, (Foley1w+IUD, n=16) a Foley intrauterine balloon was placed immediately after TCRA and removed after 1 week when it was replaced with an IUD. After 3 months, the IUD was removed. In Group C, (Foley1M+IUD, n=16), a Foley intrauterine balloon was placed immediately after TCRA. After 1 month, this was removed and replaced by an IUD, which was removed after 3 months. All patients received sequential treatment of estrogen and progesterone on the day of operation, and the range and degree of adhesion were observed by hysteroscopy at 1 and 3 months after operation. Doctors who performed the second-look and third-look hysteroscopy were blinded to the allocation. B-ultrasound examination was performed to detect endometrial thickness, telephone follow-up was performed to record menstruation and pregnancy. The severity of IUA was rated according to the American Fertility Society (AFS), as shown in the table below (Box 1).
Full table

Full table
The project was approved by the ethical committee of the Nantong Maternal and Child Health Hospital (No. Y2015095) and was in accordance with the Declaration of Helsinki (as revised in 2013). The trial protocol was explained to the patients with detail and informed consent were obtained from all the patients.
Participating women
The inclusion criteria were as follows: healthy women aged 20 to 35 years, with reduced menstrual volume or amenorrhea symptoms, diagnosed with moderate to severe adhesions, according to the AFS score, infertile women with a future fertility desire and IUA were the only infertile factor, without contraindications for the use of hormone drugs or antibiotics; with great treatment compliance. Patients were excluded if they (I) were diagnosed with serious medical or surgical disease which may impact analysis results; (II) had decreased ovarian function according to sex hormone levels; (III) genital tract inflammation, tuberculosis, tumor, or malformation.
Sample size
Based on our preliminary experiment, a sample size of 75 participants (25 per group) was calculated to achieve 90% power. To allow for a 20% lost rate of follow-up, we planned to enroll 96 participants.
Interventions
Preoperative preparation
Patients with clinical symptoms and IUA confirmed by hysteroscopy were selected by outpatient doctors. IUA patients meeting the inclusion criteria were recruited by investigators and divided into moderate IUA and severe IUA groups according to AFS score. Patients in the two groups were numbered according to the order of admission [1–48], and a computer random generator was used to divide the patients into three groups, with 16 in each group. We use Yuan Gong medicated Cu-IUDs which were provided by Yantai Family Planning Medical Device Company Limited. Foley balloon catheters with external drainage bag were provided by Malaysia Youle Technology Company Limited (Model No. 2111430).
All participants were informed of the operation and the need for follow up,and were admitted to the day care ward. Non-amenorrhea patients were considered suitable for surgery 3–7 days after menstruation and amenorrhea patients at any time. After admission, a detailed medical history was recorded, and examinations were completed including blood leukocyte determination, leucorrhea analysis, and B-ultrasound (measurement of endometrial thickness). Preoperative vaginal cleaning was performed, and after screening for drug contraindications, a 0.5 mg carboprost methylate suppository (Kayunshuan, specification: 0.5 mg, Manufacturer: Northeast pharmaceutical group Shenyang No. 1 Pharmaceutical Co. LTD.) was placed in the posterior vaginal fornix to promote cervical softening. Perioperative antibiotics (Cefazolin sodium pentahydrate, 1.0 g) were used to prevent infection.
Surgical procedures
All surgeries were performed by experienced gynecologists with titles of deputy senior, or above and qualifications in hysteroscopy. The surgical area was again disinfected before surgery to prevent infection, the position and depth of the uterus were probed, and the cervix was dilated with a dilatation stick to size 9. Using turgor medium normal saline, the normal shape of the patient’s uterine cavity was restored after operation of the plasma electric cutting needle under B-ultrasound monitoring. The blockage of the bilateral oviduct openings were removed. Normal endometrial tissue should be protected as much as possible throughout the entire surgical procedure. After confirming no active bleeding, a sodium hyaluronate (Xinkeling, Specification: 3 mL, Manufacturer: Hangzhou Singclean Medical Products Co., Ltd.) was used, and after surgery, either IUD or Foley intrauterine balloon was placed according to the groups. Different doses of normal saline were injected into the balloon according to the volume of the uterine cavity, with the routine dose being 3–5 mL. However, during the actual operation, the fluid volume of the syringe was reduced by 0.5 mL after resistance was felt in the process of injecting water. After the operation was complete, an external drainage bag was used to fully drain the blood in the uterine cavity. During the postoperative hysteroscopy review, patients of three groups could not be blinded. Postsurgical assessors who were blinded to the randomization performed the second and the third hysteroscopy and evaluated the adhesion score. IUDs were removed at the second hysteroscopy.
Intravenous antibiotics were used to prevent infection during the perioperative period (1 day total), except those with allergies. Estrogen and progesterone were administered from the day of surgery and estrogen was administered orally from the day of surgery for 21 days. Dydrogesterone tablets (Dafutong, Specification: 10 mg, Manufacturer: Abbott Biologicals B.V.) were taken orally from the 12th day of operation for 10 days. The estrogen (Bujiale, Specification: 2 mg), Manufacturer: Abbott Biologicals B.V.) dose was 4–6 mg daily and the progesterone dose was 20 mg daily.
Main outcomes and measures
Hysteroscopy was performed in all three groups at 1 month and 3 months after operation. The primary outcome was AFS score, which contains the adhesion type, adhesion range and menstrual volume. The secondary outcomes included leucorrhea, white blood cell count, pregnancy and endometrial thickness. Type and range of intrauterine adhesion were recorded by surgeons immediately after hysteroscopy. Transvaginal ultrasound (TVU) was performed to measure endometrial thickness before menstruation preoperatively and postoperatively.
Statistical methods
All data were collected in Nantong Maternal and Child Health Hospital from January 2016 to December 2019 and were statistically processed by SPSS 23.0 software. Measurement data were expressed as mean ± standard deviation, and the three groups were compared by ANOVA. LSD analysis was used when variances were homogeneous, and Welch test was used when variances were not homogeneous. If P<0.05, it was considered statistically significant and post hoc test multiple comparisons were conducted. The t-test was used to compare the two groups, and P<0.05 was considered statistically significant. Enumeration data was expressed by rate (%), and the Chi-square test or Fisher’s precision probability test were used for comparison. P<0.05 was considered statistically significant.
Results
Comparison of preoperative clinical data
A total of 96 patients were included in the final analysis. In this study, there were no cases of shedding during the follow-up. In each group of moderate and severe IUA patients, there were 16 cases included in the final analysis. Results were analyzed by original assigned groups.
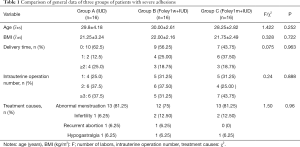
Comparison of general data of three groups of patients with severe adhesions
The mean age of patients in group A (IUD) was 29.8±4.18 years, the mean BMI was 21.25±3.24 kg/m2, and the mean delivery time was 0.68±1.01. The mean age of patients in group B (Foley1w+IUD) was 30.00±2.61 years old, the mean BMI was 22.00±2.16 kg/m2, and the mean delivery time was 0.75±0.93; and the mean age of patients in group C (Foley1m+IUD) was 28.25±2.82 years old, the mean BMI was 21.75±2.49 kg/m2, and the mean delivery time was 0.81±0.91. The common causes in the three groups were abnormal menstruation, infertility, recurrent abortion, and hypogastralgia, among which menstrual abnormality was the most common cause. The patients with abnormal menstruation in group A (IUD) accounted for 81.25%, while in group B (Foley1w+IUD) this was 75%, and in group C (Foley1m+IUD) 81.25%. There were no statistically significant differences in age, BMI, times of delivery, intrauterine operation number, and treatment causes among the three groups (P>0.05) (Table 1).
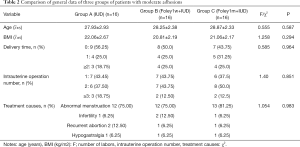
Comparison of general data of three groups of patients with moderate adhesions
The mean age of patients in group A (IUD) was 27.93±2.93 years, the mean BMI was 22.06±2.67 kg/m2, and the mean delivery time was 0.68±0.94. The mean age of patients in group B (Foley1w+IUD) was 28.25±2.38 years old, the mean BMI was 20.81±2.19 kg/m2, and the mean delivery time was 0.75±0.85; and the mean age of patients in group C (Foley1m+IUD) was 28.87±2.33 years old, the mean BMI was 21.06±2.17 kg/m2, and the mean delivery time was 0.85±0.95. The common causes of moderate adhesions in the three groups were abnormal menstruation, infertility, recurrent abortion and hypogastralgia, among which abnormal menstruation was the most common cause. The patients with abnormal menstruation in group A (IUD) accounted for 75%, group B (Foley1w+IUD) 75%, and group C (Foley1m+IUD) 81.25%. There were no statistically significant differences in age, BMI, times of delivery, intrauterine operation number, and treatment causes among the three groups (P>0.05) (Table 2).
Full table
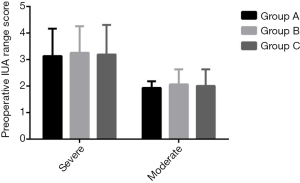
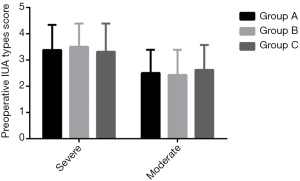
Comparison of preoperative AFS scores in patients with moderate and severe adhesions
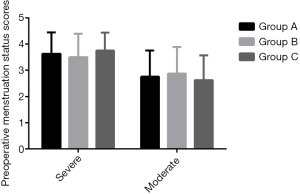
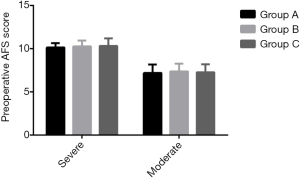
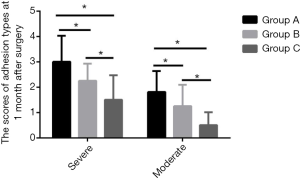
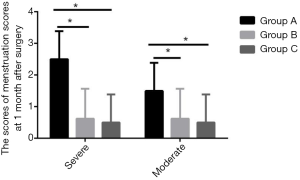
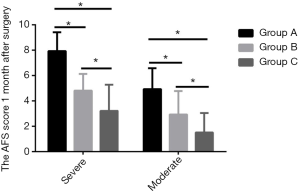
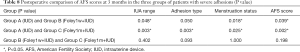
To study preoperative AFS scores, ANOVA and chi-square test were used to compare patients with severe adhesions and moderate adhesions in the groups, and the differences were statistically significant (P<0.05) (Table 3). In severe and moderate patients, there was no statistical significance in adhesion type score, adhesion range score, menstrual status score, and AFS score among the three groups (P>0.05) (Figures 2-5).
Comparison of postoperative AFS scores in patients
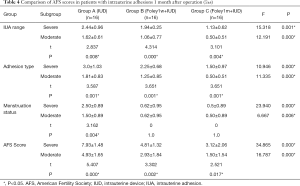
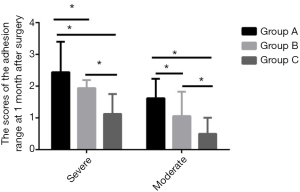
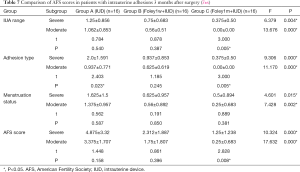
Comparison of AFS scores in patients with moderate and severe adhesions 1 month after operation
We compared the scores of patients with severe and moderate adhesions in each group 1 month following surgery and found no significant difference in menstruation in group B (Foley1w+IUD) and group C (Foley1m+IUD) (P>0.05). However, there were significant differences in other data (P<0.05). Statistically significant differences were found in IUA range, adhesion type, menstrual status, and AFS score among the three groups of severe and moderate adhesion patients (P<0.05) (Table 4). Further, the results from ANOVA and post hoc test multiple comparisons showed the following: (I) Patients with severe adhesions: comparison in adhesions range and type: there were significant differences between Group C (Foley1m+IUD) and Group A (IUD), Group C (Foley1m+IUD) and Group B (Foley1w+IUD), respectively (P<0.05), but no significant difference between group A (IUD) and group B (Foley1w+IUD) (P>0.05) (Figures 6,7). Comparison in menstrual improvement: There were significant differences between group A (IUD) and group B (Foley1w+IUD), group A (IUD) and group C (Foley1m+IUD), respectively (P<0.05). However, there was no statistically significant difference between Group B (Foley1w+IUD) and Group C (Foley1m+IUD) (Figure 8). Comparison in AFS score: Pairwise comparison among the three groups showed statistically significant differences (P<0.05) (Table 5) (Figure 9). Patients with moderate adhesions: There were statistically significant differences in IUA range, adhesion type, and AFS score (P<0.05). In terms of menstrual conditions, there were significant differences between the three groups, respectively but no significant difference between Group B (Foley1w+IUD) and Group C (Foley1m+IUD) (P>0.05) (Table 6).
Full table

Full table

Full table
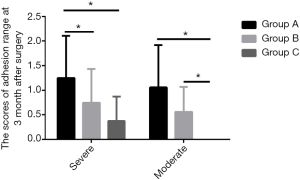
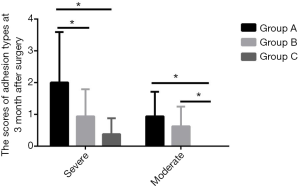
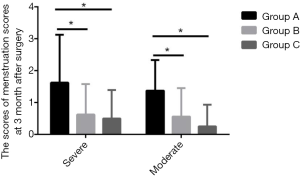
Comparison of AFS scores in patients with moderate and severe adhesions 3 months after surgery
We compared the scores of patients with severe and moderate adhesions in groups A, B, and C 3 months after surgery and found significant differences in IUA range, adhesion type, menstrual status, and AFS score between the three groups, respectively (P<0.05) (Table 7). Further, the results from ANOVA and post hoc test multiple comparisons showed the following: (I) Patients with severe adhesions: Comparison in adhesion range, adhesion type, menstrual status, and AFS score: There were significant differences between group A (IUD) and group B (Foley1w+IUD), group A (IUD) and group C (Foley1m+IUD), respectively, and the differences were statistically significant (P<0.05) and no statistically significant difference between Group B (Foley1w+IUD) and Group C (Foley1m+IUD) (Table 8) (Figures 10-13). Patients with moderate adhesions: Comparison in adhesion range: There were significant differences between the three groups and no significant difference between group A (IUD) and group B (Foley1w+IUD) (P>0.05). Comparison in menstruation status: There were significant differences between group A (IUD) and group B (Foley1w+IUD) and group C (Foley1m+IUD), respectively, and the differences were statistically significant (P<0.05). There was no significant difference between Group B (Foley1w+IUD) and Group A (IUD) (P>0.05). Comparison in adhesion type and AFS score: Pairwise comparison among the three groups showed statistically significant differences (P<0.05) (Table 9) (Figures 10-13).
Full table
Full table
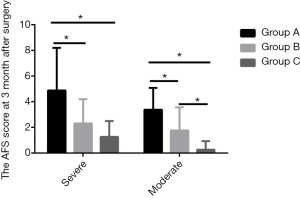
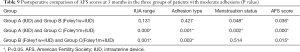
Full table
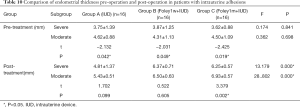
Comparison of endometrial thickness in patients with moderate and severe adhesions 3 months after surgery
We compared the endometrial thickness of patients with severe and moderate adhesions preoperatively and postoperatively in the three groups and the difference was statistically significant (P<0.05). While there was no significant difference in endometrial thickness 3 months after surgery (P>0.05) and no statistically significant difference in endometrial thickness before treatment (P>0.05), there was statistically significant difference in endometrial thickness after treatment (P<0.05) (Table 10) (Figures 14,15). Further, the results from ANOVA and post hoc test multiple comparisons showed the following: (I) In patients with severe adhesions, there were significant differences between Group A (IUD) and Group B (Foley1w+IUD) and Group C (Foley1m+IUD), respectively, and the differences were statistically significant (P<0.05). There was no statistically significant difference between Group B (Foley1w+IUD) and Group C (Foley1m+IUD) (P>0.05) (Table 11). (II) In patients with moderate adhesions, there were statistically significant differences among the three groups (P<0.05) (Table 12).
Full table
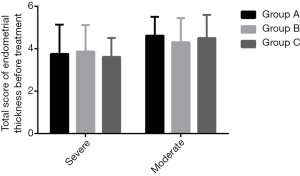


Full table

Full table
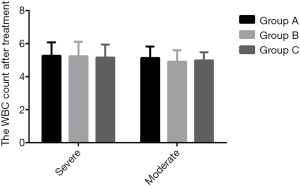
Comparison of postoperative infection in the three groups
In patients with severe adhesions, the mean white blood cell count in Group A (IUD) was (5.26±0.81)×1012/L, in Group B (Foley1w+IUD) was (5.24±0.87)×1012/L, and in Group C (Foley1m+IUD) was (5.16±0.78)×1012/L. In patients with moderate adhesions, the mean white blood cell count in Group A (IUD) was (5.13±0.69)×1012/L, in Group B (Foley1w+IUD) was (4.90±0.70)×1012/L, and in Group C (Foley1m+IUD) was (4.98±0.49)×1012/L. To study postoperative infection in the three groups, ANOVA was used to analyze the WBC count and leucorrhea routine differences of moderate and severe adhesions, and the results showed there was no statistical significance (P>0.05) (Table 13) (Figure 16).
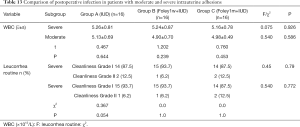
Full table
Comparison of pregnancy and conception in moderate and severe adhesion patients
Comparison of pregnancy rate in patients with moderate adhesions
Among the patients with moderate adhesions, six (37.50%) were pregnant in Group A (IUD), seven (43.75%) in Group B (Foley1w+IUD), and 14 (87.50%) in Group C (Foley1m+IUD), and there was statistical significance in the pregnancy rate among the three groups (P<0.05) (Table 14). There were significant differences between Group C (Foley1m+IUD) and Group B (Foley1w+IUD) and Group A (IUD), respectively, and the differences were statistically significant (P<0.05) but no significant difference between Group A (IUD) and Group B (Foley1w+IUD) (P>0.05) (Table 15).
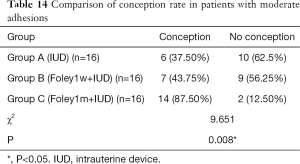
Full table

Full table
Comparison of pregnancy rate in patients with severe adhesions
Among the patients with severe adhesions, four (25.0%) were pregnant in Group A (IUD), six (37.5%) in Group B (Foley1w+IUD), and eight (50%) in Group C (Foley1m+IUD). There was no statistical significance in the pregnancy rate among the three groups (P>0.05) (Table 16).
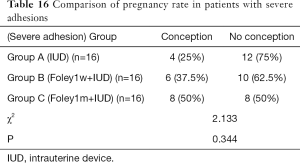
Full table
Discussion
Symptoms and risk factors of intrauterine adhesions
Mo et al. retrospectively analyzed factors influencing IUA and found age and BMI were not influencing factors, but female genital tract inflammation, an excessive number of pregnancies, history of intrauterine surgery [curettage, negative pressure suction, and cesarean section (22,23) were. Others have pointed out that more than two intrauterine operations, a curettage time of more than 15 minutes, and a history of myoma of uterus and polyps were also harmful factors (24,25). Chen et al. further conducted an in-depth study on patients with secondary infertility and found that the number of abortions and surgical methods were not risk factors for secondary infertility after induced abortion, but IUA, endometritis, chronic salpingitis, ovarian dysfunction, and endometriosis were (26). Based on the above results we believe to the most effective way of reducing IUA can be considered from four perspectives. The first of these concerns reducing the number of induced abortions through public health education on the range of contraceptive measures. Secondly, improving the skills of surgeons will reduce suction and scraping time, minimize endometrial damage, and potentially avoid the possibility of secondary or even multiple curettage caused by uterine residue; Thirdly, during uterine surgery, preoperative and postoperative infection prevention should be strengthened to reduce the occurrence of pelvic inflammation, and fourthly, regular physical examination should be carried out on patients after surgery, to monitor any changes and initiate timely treatment. There are seven evaluation criteria for the severity of IUA (27). In this study, the inclusion criteria of patients with moderate and severe adhesions were strictly controlled according to the AFS score, and there was no difference in the general data of patients in different groups, which improved the accuracy of the experimental results.
Analysis of the factors affecting the postoperative efficacy of intrauterine adhesions
Many researchers have analyzed the factors influencing the treatment effect of IUA using hysteroscopy. Yang et al. reported that a longer disease course caused IUAs to be become denser, and the larger the range of adhesions, the more likely they were to affect postoperative efficacy. In addition, the use of postoperative estrogen and progesterone was a protective factor (28). Therefore, the present study did not generally examine all types of patients with IUA, but separated patients with different severity and complexity. On this basis, differences in the efficacy of varying physical barriers to prevent re-adhesion after TCRA were obtained in patients with different degrees of disease severity. Cai et al. studied estrogen receptors after TCRA and found that estrogen can effectively improve menstrual and uterine morphology, and the expression of ER is closely related to the efficacy of estrogen (29). Haas (30) and Bu (31) confirmed through their respective studies that the combined use of estrogen and progesterone was significantly better than that of estrogen alone in maintaining endometrium stability and improving the pregnancy rate. However, the views of scholars differ on the dosage of estrogen. While Liu (32) believed that large doses of estrogen were effective, Zhou (33) held that physiological doses were safe and effective. In the present study, estrogen and progesterone were mainly used in combination. Estradiol valerate was selected for estrogen (4–6 mg/day), and dydrogesterone tablet was used for progesterone (20 mg/day). The three groups of patients received this hormone regimen simultaneously and at the same dose, facilitating the protective effect of estrogen in the prevention of adhesion.
Necessity of measuring endometrial thickness
Intrauterine adhesions are an important cause of infertility in women, and endometrial damage is by far the most important, though not the total, cause of IUA. When the morphology and function of the intima are normal, menstruation can be formed by periodic growth and shedding, which can also provide a good endometrial environment for embryo implantation. The amount of menstruation after surgery also reflects whether the function of the endometrium is intact.
Many scholars believe that the thickness of endometrium that can promote pregnancy should be at least 8 mm. In clinical practice, endometrium thickness is usually monitored in vitro by auxiliary means such as B-ultrasound to predict the chance of pregnancy. Endometrium thickness before and after hysteroscopic repair (5,34) is helpful in assessing the possibility of conception, as endometrium thinness can directly affect conception and even lead to adverse pregnancy outcomes. When the uterine cavity volume and endometrial thickness can be recovered in time after intrauterine surgery, it can effectively protect the uterus and prevent IUA, as shown by Evans-Hoeker et al. (5). Therefore, the present study compared the efficacy of three different methods by measuring endometrial thickness before and after surgery. We concluded that the postoperative intrauterine implantation of IUA patients with an IUD or Foley balloon, regardless of the severity of adhesion, could effectively improve endometrial thickness, as could the appropriate extension of intrauterine balloon implantation time in patients with moderate adhesions. Further, these findings may provide effective guidance for clinical practice.
Pregnancy rate post TCRA
Foreign studies (35) reported that the pregnancy rate after TCRA could reach 52%, but in the case of severe adhesion, this figure would significantly decrease. However, domestic data show a significantly lower value, with one study reporting a pregnancy rate of only 22.5–33.3% (8). While the direct effect of endometrial thickness on pregnancy was described above, Zhao et al. (36) listed other influencing factors, including age, endometrial area, preoperative adhesion degree, postoperative menstrual improvement, and adhesion recurrence. Many factors have been identified as inducing infertility, including immune system dysfunction and complications of internal medicine and surgery. However, most studies have examined these factors from the perspective of determining the chances of postoperative pregnancy, while few have directly followed postoperative pregnancy for extensive durations. The appropriate time for pregnancy after TCRA is within 1 year of surgery, and when there is no need for delayed fertility treatment after surgery (37). In the present study, we recommended patients receive fertility guidance in the reproductive assisted pregnancy clinic of our hospital immediately after the second hysteroscopy, and their pregnancy status under different treatment methods was followed up one year after surgery. Our results showed that the placement of an intrauterine balloon and IUD could improve postoperative pregnancy, but for patients with moderate adhesions, the effect of prolonged implantation of an intrauterine balloon was better than that of IUD implantation and short time balloon placement. However, in patients with severe adhesions, the duration of balloon placement had no significant effect on postoperative pregnancy rate. This adds weight to the conjecture that even if the physiological structure is restored, it is difficult for patients with severe adhesions to return to normal reproductive function. Novel and effective treatments to deal with these circumstances remain to be developed.
Prevention and treatment of intrauterine re-adhesion: IUD and intrauterine balloon
Yu et al. (8) showed that the re-adhesion rate after TCRA can be as high as 62.5%, which seriously impacts postoperative menstrual improvement and fertility. At present, commonly used anti-adhesion methods include IUDs and intrauterine balloons and auxiliary measures including biological materials (hyaluronic acid and hydroxymethyl chitosan), and estrogen, while amniotic membrane (38), stem cells (39), and traditional Chinese medicine (40) have not been widely used in clinical practice. Some studies have investigated the use of a single method (41), while others have investigated a combination of multiple methods. Some researchers (42) have compared patients who used a balloon uterine stent alone with those who received an IUD combined with intrauterine balloon and found that the combined use of the stent prevents adhesion recurrence better than the use of the stent alone. Others (43) compared patients with 7, 14, and 28 days of balloon placement, and believed that the chance of re-adhesion could be reduced if the balloon placement was 28 days, but there was no further study on how this may influence pregnancy. In the present study, the IUD group [Group A (IUD)]and balloon group [Group B (Foley1w+IUD)] were set, with Group C (Foley1m+IUD, i.e., the extended balloon placement time group) added as a contrast, and differences were found among the three groups. Prolongation of balloon placement could improve adhesion type, adhesion range, AFS score, and endometrial thickness in patients with moderate adhesion, and in terms of menstrual improvement, the effect was the same as that of longer balloon placement versus shorter balloon placement. However, there was no improvement in the efficacy of prolonging balloon placement time in patients with severe adhesions. The results may be related to endometrial injury repair mechanism or intrauterine infection. Therefore, for patients with severe intrauterine adhesions, the optimal treatment is IUD combined with intrauterine balloon, and it’s unnecessary to prolong the placement of balloon. Comprehensive consideration of the above conclusions can effectively guide clinical work, as different anti-adhesion methods should be chosen according to the different degree of IUA.
Deficiency and prospect
Although prolonged balloon placement has been proven effective in moderate IUA, there is a risk of balloon shedding during clinical procedures, and some patients have reported lower abdominal pain. How much water can be injected into the balloon to achieve an anti-adhesion effect without affecting the blood supply of the endometrium and without causing lower abdominal pain remains is subject to further study.
As this study involved a small sample size and was conducted in a single center, studies with larger sample sizes and conducted across multiple centers are required to confirm the results.
The follow-up time of pregnancy in this study was short, and there was a lack of further tracking of long-term pregnancy, pregnancy outcomes, and fetal conditions.
Use of the term “infertility” as a chief complaint and as an indication for hysteroscopy is still controversial. Determining the specific plan for repeated hysteroscopy after TCRA, especially for patients with fertility requirements, is still to be resolved.
At present, there are not enough effective anti-adhesion materials used in the clinical setting, and the efficacy of various methods is not uniform. We expect the emergence of new materials may go towards resolving this.
Conclusions
In this study, 96 patients with moderate and severe intrauterine adhesions were studied and the prevention of intrauterine re-adhesion and improvement of pregnancy rate were analyzed in depth. The main conclusions were as follows:
- The effect of an intrauterine balloon combined with IUD in preventing re-adhesion was better than that of IUD alone. In clinical practice, combined treatment can have a better therapeutic effect.
- Appropriate prolongation of intrauterine Foley balloon placement has no significant advantage for patients with severe adhesions, but for patients with moderate adhesions, it can safely significantly improve adhesion prevention and the pregnancy rate.
- Patients with severe adhesions need further exploration to find appropriate treatment methods.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at https://dx.doi.org/10.21037/apm-21-1296
Trial Protocol: Available at https://dx.doi.org/10.21037/apm-21-1296
Data Sharing Statement: Available at https://dx.doi.org/10.21037/apm-21-1296
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/apm-21-1296). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The project was approved by the ethical committee of the Nantong Maternal and Child Health Hospital (No. Y2015095) and was in accordance with the Declaration of Helsinki (as revised in 2013). All patients signed informed consent prior to participation.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Abiodun OM, Balogun OR, Fawole AA. Aetiology, clinical features and treatment outcome of intrauterine adhesion in Ilorin, Central Nigeria. West Afr J Med 2007;26:298-301. [PubMed]
- Al-Inany H. Intrauterine adhesions. An update. Acta Obstet Gynecol Scand 2001;80:986-93. [PubMed]
- Deans R, Abbott J. Review of intrauterine adhesions. J Minim Invasive Gynecol 2010;17:555-69. [Crossref] [PubMed]
- Sanders B. Uterine factors and infertility. J Reprod Med 2006;51:169-76. [PubMed]
- Evans-Hoeker EA, Young SL. Endometrial receptivity and intrauterine adhesive disease. Semin Reprod Med 2014;32:392-401. [Crossref] [PubMed]
- Huang H, Cheng C, Johnson G, et al. Hysteroscopic Intrauterine Adhesiolysis Using a Blunt Spreading Dissection Technique With Double-action Forceps. J Minim Invasive Gynecol 2018;25:583-4. [Crossref] [PubMed]
- Tiras MB, Oktem M, Noyan V. Laparoscopic intracorporeal ultrasound guidance during hysteroscopic adhesiolysis. Eur J Obstet Gynecol Reprod Biol 2003;108:80-4. [Crossref] [PubMed]
- Yu D, Wong YM, Cheong Y, et al. Asherman syndrome--one century later. Fertil Steril 2008;89:759-79. [Crossref] [PubMed]
- Wu XF, Li L. Influencing factors and research progress of women intrauterine device placement. Maternal and Child Health Care of China 2016;32:2237-9.
- Lin XN, Zhou F, Wei ML, et al. Randomized, controlled trial comparing the efficacy of intrauterine balloon and intrauterine contraceptive device in the prevention of adhesion reformation after hysteroscopic adhesiolysis. Fertil Steril 2015;104:235-40. [Crossref] [PubMed]
- . Expert consensus on the diagnosis and management of intrauterine adhesions in China. Zhonghua Fu Chan Ke Za Zhi 2015;50:881-7. [PubMed]
- Yang JH, Chen MJ, Chen CD, et al. Optimal waiting period for subsequent fertility treatment after various hysteroscopic surgeries. Fertil Steril 2013;99:2092-6.e3. [Crossref] [PubMed]
- Chen L, Zhang H, Wang Q, et al. Reproductive Outcomes in Patients With Intrauterine Adhesions Following Hysteroscopic Adhesiolysis: Experience From the Largest Women's Hospital in China. J Minim Invasive Gynecol 2017;24:299-304. [Crossref] [PubMed]
- Manchanda R, Rathore A, Carugno J, et al. Classification systems of Asherman's syndrome. An old problem with new directions. Minim Invasive Ther Allied Technol 2021;1-16. [Crossref] [PubMed]
- Cao M, Pan Y, Zhang Q, et al. Predictive value of live birth rate based on different intrauterine adhesion evaluation systems following TCRA. Reprod Biol Endocrinol 2021;19:13. [Crossref] [PubMed]
- Zheng SX, Wang J, Wang XL, et al. Feasibility analysis of treating severe intrauterine adhesions by transplanting menstrual blood-derived stem cells. Int J Mol Med 2018;41:2201-12. [Crossref] [PubMed]
- Cai H, Qiao L, Song K, et al. Oxidized, Regenerated Cellulose Adhesion Barrier Plus Intrauterine Device Prevents Recurrence After Adhesiolysis for Moderate to Severe Intrauterine Adhesions. J Minim Invasive Gynecol 2017;24:80-8. [Crossref] [PubMed]
- Huang H, Xu B, Cheng C, et al. A novel intrauterine stent for prevention of intrauterine adhesions. Ann Transl Med 2020;8:61. [Crossref] [PubMed]
- Wu J, Jin L, Zhang Y, et al. LncRNA HOTAIR promotes endometrial fibrosis by activating TGF-β1/Smad pathway. Acta Biochim Biophys Sin (Shanghai) 2020;52:1337-47. [Crossref] [PubMed]
- Bosteels J, Weyers S, D'Hooghe TM, et al. Anti-adhesion therapy following operative hysteroscopy for treatment of female subfertility. Cochrane Database Syst Rev 2017;11:CD011110 [Crossref] [PubMed]
- Cao J, Liu D, Zhao S, et al. Estrogen attenuates TGF-β1-induced EMT in intrauterine adhesion by activating Wnt/β-catenin signaling pathway. Braz J Med Biol Res 2020;53:e9794 [Crossref] [PubMed]
- Salazar CA, Isaacson K, Morris S. A comprehensive review of Asherman's syndrome: causes, symptoms and treatment options. Curr Opin Obstet Gynecol 2017;29:249-56. [Crossref] [PubMed]
- Ad Esiyun AG, Zayyan MS, Ojabo A. Aetiology of involuntary infertility following caesarean birth in last pregnancy. Pakistan Journal of Medical ences Online 2011;27:1005-8.
- Mo X, Qin G, Zhou Z, et al. Assessment of Risk Factors of Intrauterine Adhesions in Patients With Induced Abortion and the Curative Effect of Hysteroscopic Surgery. J Invest Surg 2019;32:85-9. [Crossref] [PubMed]
- Di Spiezio Sardo A, Di Guardo F, Santangelo F, et al. Commentary on "Assessment of Risk Factors of Intrauterine Adhesions in Patients with Induced Abortion and the Curative Effect of Hysteroscopic Surgery". J Invest Surg 2019;32:90-2. [Crossref] [PubMed]
- Chen Y, Liu L, Luo Y, et al. Prevalence and Impact of Chronic Endometritis in Patients With Intrauterine Adhesions: A Prospective Cohort Study. J Minim Invasive Gynecol 2017;24:74-9. [Crossref] [PubMed]
- Nasr AL, Al-Inany HG, Thabet SM, et al. A clinicohysteroscopic scoring system of intrauterine adhesions. Gynecol Obstet Invest 2000;50:178-81. [Crossref] [PubMed]
- Yang JH, Chen CD, Chen SU, et al. The influence of the location and extent of intrauterine adhesions on recurrence after hysteroscopic adhesiolysis. BJOG 2016;123:618-23. [Crossref] [PubMed]
- Cai H, Li H, He Y. Interceed and Estrogen Reduce Uterine Adhesions and Fibrosis and Improve Endometrial Receptivity in a Rabbit Model of Intrauterine Adhesions. Reprod Sci 2016;23:1208-16. [Crossref] [PubMed]
- Haas J, Smith R, Zilberberg E, et al. Endometrial compaction (decreased thickness) in response to progesterone results in optimal pregnancy outcome in frozen-thawed embryo transfers. Fertil Steril 2019;112:503-509.e1. [Crossref] [PubMed]
- Bu Z, Yang X, Song L, et al. The impact of endometrial thickness change after progesterone administration on pregnancy outcome in patients transferred with single frozen-thawed blastocyst. Reprod Biol Endocrinol 2019;17:99. [Crossref] [PubMed]
- Liu AZ, Zhao HG, Gao Y, et al. Effectiveness of estrogen treatment before transcervical resection of adhesions on moderate and severe uterine adhesion patients. Gynecol Endocrinol 2016;32:737-40. [Crossref] [PubMed]
- Zhou Q, Wu X, Dai X, et al. The different dosages of estrogen affect endometrial fibrosis and receptivity, but not SDF-1/CXCR4 axis in the treatment of intrauterine adhesions. Gynecol Endocrinol 2018;34:49-55. [Crossref] [PubMed]
- Schlaff WD, Hurst BS. Preoperative sonographic measurement of endometrial pattern predicts outcome of surgical repair in patients with severe Asherman's syndrome. Fertil Steril 1995;63:410-3. [Crossref] [PubMed]
- Capmas P, Mihalache A, Duminil L, et al. Intrauterine adhesions: What is the pregnancy rate after hysteroscopic management? J Gynecol Obstet Hum Reprod 2020;49:101797 [Crossref] [PubMed]
- Zhao X, Liu Y, Zhang A, et al. Logistic regression analyses of factors affecting fertility of intrauterine adhesions patients. Ann Transl Med 2020;8:49. [Crossref] [PubMed]
- Aharon D, Sekhon L, Lee JA, et al. Optimal Interval of Time from Operative Hysteroscopy to Embryo Transfer in an In Vitro Fertilization Cycle. J Minim Invasive Gynecol 2019;26:1083-1087.e1. [Crossref] [PubMed]
- Li C, Cai A, Sun C, et al. The study on the safety and efficacy of amnion graft for preventing the recurrence of moderate to severe intrauterine adhesions. Genes Dis 2020;7:266-71. [Crossref] [PubMed]
- Zhang J, Li N, Chen S, et al. Transplantation induced pluripotent stem cells in situ improves fertility outcome impaired by intrauterine adhesions in mice. 2016
- Ya-Li T, Jia XU, Dong J, et al. Mechanism of Fuke Qianjin Capsules in treating intrauterine adhesion in rats through TGF-β1-PI3K/Akt signaling pathway. Zhongguo Zhong Yao Za Zhi 2020;45:4705-11. [PubMed]
- Gupta S, Talaulikar VS, Onwude J, et al. A pilot study of Foley's catheter balloon for prevention of intrauterine adhesions following breach of uterine cavity in complex myoma surgery. Arch Gynecol Obstet 2013;288:829-32. [Crossref] [PubMed]
- Huang XW, Lin MM, Zhao HQ, et al. A prospective randomized controlled trial comparing two different treatments of intrauterine adhesions. Reprod Biomed Online 2020;40:835-41. [Crossref] [PubMed]
- Yang X, Liu Y, Li TC, et al. Durations of intrauterine balloon therapy and adhesion reformation after hysteroscopic adhesiolysis: a randomized controlled trial. Reprod Biomed Online 2020;40:539-46. [Crossref] [PubMed]
(English Language Editor: B. Draper)




