Methods of reducing pain during bone marrow biopsy: a narrative review
Introduction
Bone marrow biopsy (BMBx) and aspiration is a fundamental part of the diagnostic workup of various benign and malignant hematological disorders. Improved via several variations and technical modifications ever since its advent in the early nineteenth century, the procedure plays a central role in establishing diagnosis in various hematological and systemic diseases (1,2). The standard methods of bone marrow sampling and BMBx have remained unchanged ever since its standardization in the early 1970s (1,3-5). Despite several breakthroughs in medicine, limited work has been done to develop methods/measures that would better control pain in patients undergoing the procedure. To date, BMBx remains a considerably painful procedure, with about half of the patients reporting severe and unbearable pain and discomfort during the procedure (1,6).
As modern medicine becomes patient-oriented and tailored to ensure each patient derives maximum benefit from the healthcare system, importance is given to reduce pain associated with medical procedures/interventions (1). Since there is paucity of data concerning the treatment and prevention of pain during BMBx, strategies to combat this problem have not been systematized (1,2). There is no formal consensus on the optimal approach to reduce pain associated with BMBx. This review discusses the current literature available regarding this subject to summarize various methods that can be adopted to minimize pain experienced by patients undergoing bone marrow sampling.
Literature search
The PubMed database was searched for articles published in the English-language literature. Medical subject headings (MeSH) including ‘bone marrow biopsy’, ‘bone marrow aspiration’, ‘bone marrow trephine biopsy’, ‘bone marrow sampling’, ‘pain control’, ‘pain relief’, ‘discomfort’, ‘analgesia’ were cross-referenced in the search, which was supplemented with a secondary manual search of PubMed, Ovid Medline, Google Scholar and Cochrane databases. Further manual searching was carried out by reviewing the articles listed in the references of the articles obtained from the primary search.
Bone marrow aspiration and biopsy
A BMBx is typically performed by a trained physician in a hospital, usually in an out-patient setting. The most common sampling site is the posterior superior iliac spine, followed by the anterior superior iliac crest. In the past, the sternum has also been used as a biopsy site, however, due to the risks of mediastinal injury and complications such as cardiac tamponade, this option is commonly kept as a last resort when sampling is not possible from other sites (7,8). Sternal puncture is also commonly used for patients who only require bone marrow aspiration with no need for trephine biopsy (8). A local anesthetic agent is administered to reduce sensations and minimize pain at the biopsy site. Some patients may also be given systemic analgesics and anxiolytics/sedatives before the procedure to reduce anxiety (9). A needle is inserted through the skin and into the periosteum. With twisting motion and pressure applied, the needle is driven through the bony cortex and into the marrow cavity. Most of the pain and discomfort associated with the procedure comes from the needle piercing through the periosteum. A solid, cylindrical sample of the marrow is removed as a trephine biopsy, followed by attachment of a syringe and aspiration of marrow fluid. The aspiration may be performed before the biopsy in some cases, depending on the physician practices and institutional policies (1). The needle is then withdrawn and pressure is applied to stop excessive blood loss from the sampling site.
The posterior superior iliac spine is the preferred site of BMBx due to its surface prominence, safety and convenience. A BMBx procedure from the posterior superior iliac spine usually takes 10 minutes, but the procedure may take up to 30 minutes depending on other sites of biopsy (and hence their respective convenience), experience of the physician and co-operation of the patient (1,10). The patient is discharged after a brief period of observation following the procedure to ensure no immediate complications follow. Additional observation time and post-procedural care is needed for patients who received systemic sedation prior to the biopsy (11). Despite its highly invasive and painful nature, complications are exceptionally rare and BMBx is generally considered a safe and low risk procedure (12).
Factors contributing to pain
Several factors have been studied to assess likelihood of pain and discomfort during BMBx. These include basic demographic factors such as age, gender, body-mass index (BMI) and ethnicity of the patient. There are no definitive correlations between the age, gender and ethnicity of the patient and pain during the BMBx (1). When concerning BMI, some studies have concluded that it plays a minimal role in association with pain (13,14), whereas others have demonstrated it to be an important factor influencing pain (15). Patients with a high BMI may have a thick layer of skin and subcutaneous tissue, making it difficult to feel the surface prominences of the posterior and anterior superior iliac crests, making the biopsy a difficult and possibly prolonged procedure requiring multiple punctures to gain access to the appropriate site. In obese patients, these sites may be inaccessible for a biopsy (16). Consequently, these patients undergo sternal puncture, which is reported to be the most painful site for marrow sampling and also holds a greater likelihood of complications (17). This may be one plausible explanation how BMI plays a role in determining pain associated with BMBx.
Some pain-influencing factors are associated with the procedure itself. Reports have demonstrated a correlation of pain with the duration of BMBx and the difficulty of obtaining an adequate sample. Patients have generally reported lower levels of pain and discomfort when the BMBx is performed by an experienced physician and the procedure lasts for around or less than 10 minutes. Experienced physicians take less time to conduct a BMBx (14,15). Experienced physicians are also easily able to overcome technical difficulties encountered during the procedure and are able to obtain a satisfactory sample in the first attempt, eliminating the need for multiple attempts and hence reducing overall pain (14,15). However, there are studies which question this notion and advocate that the effect of physician experience and physician technique on pain intensity in BMBx is minimal (13,18).
Past experience with marrow sampling is another important factor. Patients undergoing a difficult BMBx, and hence more pain, develop anticipatory anxiety which leads to fear and emotional distress, making future biopsies equally or even more painful. These patients are likely to report higher scores of pain in subsequent biopsies (18,19); hence it is important for the physician to make every effort to make the procedure as least painful as possible. This is especially important for patients with hematological malignancies who require repeated marrow sampling for assessing treatment response and prognostication (6). Patient knowledge and anticipation is also a noteworthy factor, as some studies have demonstrated that patients who are given incomplete information regarding BMBx, expected pain and adverse effects reported higher scores of pain (13,20).
Pharmacological agents
Before the procedure, a local anesthetic agent is infiltrated into the overlying skin and the periosteum of the biopsy site. Lidocaine, a neuronal voltage-gated sodium channel blocking amide, is the most commonly used agent. Other agents such as novocaine, ropivacaine, bupivacaine etc. can also be used when lidocaine is not an appropriate option, such as in patients with porphyrias, in which case bupivacaine is a safe alternative (21). Another situation in which lidocaine may not be appropriate would be hypersensitivity, though caution should be taken in regards to cross-reactivity with other amino-amides (9,22). The effectiveness of these agents, however, is limited to the skin and soft tissue overlying the biopsy site (6,23,24). Periosteal and bone anesthesia is relatively incomplete because of which BMBx remains a painful procedure for most patients with local anesthesia (LA) alone. There is lack of literature comparing the efficacy of one local anesthetic to another, and the limited data that is available shows inconsistent findings, not favoring the use of one agent over the other. For example, in a randomized trial by Kuivalainen et al. (23), articaine, another sodium channel blocker, with better bone penetration, showed no significant difference in the pain scores of patients in comparison to those who were administered lidocaine prior to BMBx.
Local anesthetic preparations are acidic solutions, hence buffering them with alkaline agents is another method of administering LA. In a randomized trial (25), lidocaine buffered with sodium bicarbonate was found to be associated with lower pain scores than unbuffered lidocaine solutions, indicating it to be a superior local anesthetic for BMBx. However, the results of this study are questionable as the participating patients served as their own controls, undergoing bilateral BMBx with buffered lidocaine infiltration on one side and unbuffered on the other. This methodology could have had possible confounding effects on the results. Another randomized control trial (26) showed buffering lidocaine solution lessened pain and burning during infiltration but did not make BMBx less painful than unbuffered preparations. These findings indicate that buffering local anesthetic solutions reduces local irritation and pain during infiltration, but may or may not provide better analgesia during BMBx than unbuffered preparations.
Intravenous sedation is sometimes used in conjunction with LA. In addition to reducing the sensation of pain, sedation has shown the added advantage of decreasing anticipatory anxiety and is frequently requested by patients who experienced an unbearably painful and difficult preceding BMBx (27). Benzodiazepines such as diazepam, lorazepam, midazolam etc. are the most commonly used sedatives (28,29). In fact, sedation with intravenous midazolam is routinely offered during BMBx in some Western countries, especially the United Kingdom (6,29). Randomized control trials have demonstrated better pain control with sedation given in conjunction with LA. Park et al. (30) reported that patients receiving intravenous lorazepam in addition to LA during BMBx reported lower pain scores, were more co-operative during and willing to undergo subsequent biopsies when needed. In another randomized trial (28), pediatric leukemia patients were assigned to receive either intravenous midazolam or placebo. Although both groups did not differ significantly as far as biopsy associated pain was concerned, it was observed that children receiving midazolam were less distressed and anxious during and after the procedure. Children in the midazolam group also reported markedly reduced post-procedural pain than the controls. Other studies have reported significantly lower pain scores during (31) and after (6,32) the BMBx when sedation was used in addition to LA. Sedation also brings about a short-term amnesia in a proportion of patients, eliminating the anxiety and emotional distress associated with the procedure altogether. This was demonstrated by Dunlop et al. (33) in a study using the combination a benzodiazepine with an opioid-narcotic and in another study using intravenous midazolam (29). Another similar study (34) using intravenous midazolam and opiates showed the same effect. However, the ability of different regimens to induce this effect depends on several factors, such as pharmacological properties, biological effects and efficacy of the combinations of drugs (27).
Deep sedation with multiple agents is another strategy used by some physicians. The combination of ketamine and propofol (ketofol) has been tested for pain relief and sedation in pediatric patients. Due to its complimentary effects, ketamine has been shown to reduce the dose of propofol required to achieve adequate sedation during painful procedures (35). Since ketamine and propofol have opposing effects on the cardiopulmonary systems, this combination is also associated with fewer overall side effects than when each agent is used individually (35,36). Ketofol can produce effective procedural analgesia and sedation in children undergoing BMBx (37), although there is limited literature since it is a relatively newer agent in medical practice. While there are several preparations with varying relative concentrations of both component drugs, formulations with larger concentrations of ketamine are associated with increased the incidence of adverse effects such as nausea, increased recovery time and psychotomimetic effects (hallucinations, nightmares, etc.). On the other hand, combinations with lowers doses of ketamine relative to propofol provide equally adequate sedation and analgesia with shorter recovery time and decreased psychotomimetic side effects, and may be a more appropriate choice, especially in pediatric patients (35,38-40). The advantages of reducing required dose, decreased side effects and shorter recovery time with equally effective pain relief have also been demonstrated by adding fentanyl to propofol (41).
In a retrospective report by Burkle et al. (42), the safety of deep sedation with midazolam, propofol and fentanyl was studied. No differences were observed between the two groups, other than the deep sedation group being less likely to require blood transfusions. Although the benefits of sedation are evident in several studies, the drawbacks and risks associated with it need to be kept in mind. There is an increased risk of adverse events with patients receiving sedatives. There is a substantial risk of respiratory depression, aspiration and aspiration pneumonia associated with sedation, as well as other complications such as hemodynamic instability, arrhythmias and even cardiac arrest (43,44). This not only prolongs the post-procedural hospital stay but also necessitates the use of additional monitoring equipment and hospital staff to keep adverse events to a minimum (6,42). For example, in one study, up to 19% of patients receiving intravenous midazolam required flumazenil to reverse sedation due to respiratory depression (29). As current medical practice becomes progressively individualized, physicians need to balance the advantages of using sedatives against the risk of adverse effects for each patient to ensure the least painful BMBx with the lowest possible risk of complications.
Although most of the pain and discomfort of BMBx arises from the puncture to gain entry into the marrow cavity, a considerable amount comes from the suction and aspiration of marrow fluid, one which is not affected by LA (1). In a prospective study by Vanhelleputte et al. (15), when compared with the placebo group, patients receiving tramadol prior to the procedure reported less intensity in pain during the aspiration phase of the BMBx, indicating that the pain associated with vacuum aspiration of marrow is responsive to opioids. In this study, tramadol given as a 50 mg dose one hour before the procedure proved beneficial, with mild sedation and transient dizziness being the only reported side effects to the medication. Since tramadol lacks unwanted inhibitory effects on the cardiopulmonary systems, it is considered to be the safest and well tolerated amongst all opioid analgesics (45,46). Fentanyl is another opioid narcotic that has been tested for reducing pain during BMBx, showing benefit when used in combination with propofol (41). However, in a study using sublingual single-agent fentanyl, the pain scores of the fentanyl and placebo groups were similar, with side effects occurring frequently in the fentanyl group (47).
The mixture of nitrous oxide and oxygen, commonly referred to as Entonox, is a potent analgesic gas ordinarily used in dental procedures (48). Studies have demonstrated that Entonox can be self-administered by the patient prior to and/or during the procedure and is efficacious in reducing pain and discomfort during BMBx (18,49,50). A study by Gudgin et al. (49) showed Entonox to be equally as effective or better than sedation with midazolam in patients who had previously received the latter during past BMBx. Similarly, in a study by Kanagasundaram et al. (48), Entonox was shown to be effective in reducing pain in pediatric patients undergoing painful procedures (including BMBx), with 65% of patients having no recollection of undergoing the procedure. Adverse effects were reported in only up to 7.8% patients. While oxygen desaturation was observed in some patients, none of the patients developed hypoxia. In a comparative study (50) with lidocaine, Entonox used as an adjuvant to LA showed better pain control than LA alone. Entonox has the added benefits of being less costly, easy to administer and requiring minimal supervision. Vomiting, dysphoria, diffusion hypoxia are known adverse effects of Entonox, however, studies involving the agent as a method of analgesia report little to no adverse effects, reflecting on its safety (48-50). One study has reported the mean time to recovery from the effects of the agent being as short as 3 minutes (48). A vast majority of patients show satisfaction with Entonox, with up to 84% patients admitting to consider this method of analgesia during future biopsies. These findings indicate that Entonox is a short-acting analgesic which is a reasonable adjuvant to LA to minimize pain during BMBx. Chakupurakal et al. compared the pain relieving effects of Entonox with intravenous midazolam (29). Although both agents produced pain relieving effects in their respective group of patients, midazolam proved to be superior in terms of relieving anxiety during BMBx, pain relief during and after the procedure, as well as post-procedural amnesia. It is, however, noteworthy that up to 19% of patients in the midazolam arm experienced respiratory depression, necessitating the use of flumazenil to reverse the sedation. On the other hand, the prominent side effect associated with Entonox use was mild, transient dizziness. Although Entonox may not be as potent as midazolam, its relatively low cost, patients not requiring medical observation, prolonged hospital stay or antidotes to reverse its effects make it an attractive choice to provide patients pain relief and comfort during BMBx (50).
Methoxyflurane is another inhalation anesthetic that can be used to provide pain relief in this context. In a recent randomized control trial by Spruyt et al. (51), its efficacy and safety regarding pain control during BMBx was tested. In comparison to LA alone, adjuvant use of methoxyflurane provided markedly better pain control, reducing overall pain during BMBx and also the pain during bone marrow aspiration phase. However, in a subsequent study by Kliman et al. (52) methoxyflurane was found to be similar to lidocaine and nitrous oxide in relieving pain during BMBx. However, it is noteworthy that this study had a very low response rate of 16% amongst approached patients, which may account for the inconsistent results. While methoxyflurane proves to be a potent, rapidly acting analgesic, it has an extensive side effect profile, including inhibitory effects on the cardiopulmonary systems and nephrotoxicity. In above mentioned studies, patients receiving the inhalant were more likely to suffer from side effects, with up to 20.4% patients suffering from adverse effects, albeit mild to moderate in nature (51,52). Carefully designed, prospective studies need to be conducted to gauge the efficacy and safety of methoxyflurane for analgesic use in this context.
Non-pharmacological strategies
As mentioned earlier, patient anxiety and distress are important determinants influencing pain. In a prospective survey by Degen et al. (13), information provided prior to the biopsy had a significant effect on the level of pain experienced by the patient. Patients who reported severe and unbearable pain reported to be given inadequate or incomplete information by the physician performing the biopsy. Building a good rapport with the patient, providing accurate and comprehensible information and ensuring privacy and maximum possible comfort are fundamental aspects of the physician-patient relationship that can lower patient anxiety and apprehension prior to the procedure. This represents an effortless approach to reducing pain during BMBx, as incomplete information provided at any point has been correlated with the likelihood of severe pain. Patients who have adequate knowledge about what the experience is going to be like, either from the information provided by the physician or from a previous BMBx, are able to better anticipate what the procedure entails in order to distract themselves from the pain as much as possible and as a result, reduce the associated pain through mental strategies and psychological coping mechanisms (13).
Another method to reduce pain is to use different kinds of biopsy needles and devices, ones that inflict less pain without compromising specimen retrieval and quality. A notable example of this approach is the Goldenberg snare-coil BMBx needle. This device incorporates a spiral-shaped snare within the needle that allows for capturing of the bone marrow with a simple twist of a lever in the handle. The needle can then be withdrawn with the sample, without the need for manipulating the needle within the bone of the patient to obtain an adequate specimen, as is needed in case of a conventional BMBx, effectively eliminating the pain and discomfort associated with this step (53). The snare-coil needle was tested in a study published in 2001 (54). Of the fifty biopsies done in this study, the specimens retrieved demonstrated intact bone marrow tissue and architecture which were adequate to establish pathological diagnosis in all cases. This reflects on the snare-coil needle’s reliability to retrieve intact and adequate specimens to assist in the diagnosis of patients. However, studies comparing this device with the conventional BMBx needle are lacking. The superiority of the snare-coil needle needs to be objectively established through prospective studies of randomized trial design.
The OnControl Bone Marrow (OBM) Biopsy System represents another potential alternative to the traditional, manual technique of BMBx for reducing pain and discomfort. A battery-powered drill is used to insert the biopsy needle into the anterior superior iliac crest for extraction of bone marrow (55). One of the earliest studies investigating the OBM technique reported it to be a quick and convenient method of bone marrow sampling associated with low pain scores and no complications (56). Several subsequent studies have also demonstrated the OBM technique to be easier and faster in comparison to the manual technique of BMBx (57-59). Not only this, but these studies also showed that OBM was associated with substantially reduced pain scores from patients. Samples obtained via OBM technique were larger and of superior quality, providing more tissue for diagnosis, increasing diagnostic yield and accuracy and eliminating the need for repeat procedures, making it an attractive method of bone marrow sampling not only for producing less pain and discomfort but also for yielding adequate tissue samples to increase the accuracy of diagnostics in patients.
Other non-pharmacological strategies have also been explored in their ability to reduce pain during BMBx. Hypnosis and cognitive behavioral therapy (CBT) are examples of such alternative methods. In a randomized control trial involving pediatric patients undergoing BMBx (60), CBT and hypnosis were compared with controls. Patients receiving either CBT or hypnosis reported significantly less pain and discomfort than did the controls. Although CBT and hypnosis were equally as effective, patients in the CBT group showed more behavioral distress and anxiety than those in the hypnosis group. Accardi and Milling (61) conducted a methodological literature review, demonstrating the superiority of hypnosis in controlling pain and discomfort when used in conjunction with LA than other ways such as distracting techniques and LA alone. Hypnosis was also found to be efficacious in alleviating pain during other invasive procedures such as lumbar punctures and post-surgical pain. The aforementioned studies examined the utility of these methods in pediatric and adolescent age groups, indicating that CBT and hypnosis were reasonable strategies in preparing pediatric and adolescent patients for BMBx to reduce pain and discomfort. A randomized control trial (62) testing the effectiveness of hypnosis in adults undergoing BMBx showed reduce anxiety in patients during the procedure, although the pain scores did not differ significantly between the hypnosis and standard of care groups, indicating hypnosis is not as effective in adult patients as it is in younger age groups. This highlights that hypnosis, as a method of pain control during BMBx can be more effective for pediatric patients, as children can be more suggestible and have raised susceptibility to hypnosis in comparison to adults (63).
Other approaches, such as music therapy, have also been tested. In a randomized trial by Shabanloei et al. (64), music therapy was shown to be associated with lower levels of pain and anxiety during the procedure when combined with LA during BMBx. Other ways, such as providing nature screens coupled with nature sounds, provide distraction and consequently reduce pain and anxiety associated with BMBx.
Another tested modality is transcutaneous electric nerve stimulation (TENS). In a recent randomized control trial, Tucker et al. (65), investigated the utility of TENS during BMBx as an adjunctive method of pain relief in addition to standard techniques. Patients in the intervention group stated satisfaction with TENS and would recommend others to use the same modality during BMBx. However, these reports were purely subjective and objective comparison using the numerical pain rating scales failed to show any benefit. This indicates that TENS provides a subjective benefit to patients; whether it can provide objectively superior pain relief needs to be explored through further studies.
Magnetic acupressure has also been tried as a non-pharmacological method of pain relief during BMBx (66). Although not shown to bring about a substantial decrease in median pain scores of the patients, it did reduce the proportion of patients who reported severe pain during the biopsy. Since this is an inexpensive and well tolerated modality that requires minimal training, its applicability in this patient population needs to be confirmed through prospective studies involving a large sample sizes.
Conclusions
Despite several modifications and different protocols, BMBx remains an extremely painful and uncomfortable procedure for most patients. LA by infiltration with sodium channel blockers, such as lidocaine is the most basic and widely used means of providing analgesia, however, pain relief is limited and does not affect the severe pain associated with bone puncture and marrow aspiration. Buffered local anesthetic solutions are associated with reduced pain and discomfort during infiltration but may or may not provide better analgesia during the actual biopsy. Sedation during the procedure significantly reduces anticipatory anxiety, provides better pain control and even produces short term amnesia regarding the BMBx. Benzodiazepines are most commonly used for sedation, although hypnotics, such as propofol, have also been used. However, side effects are significant with sedation, including cardiopulmonary depression, requiring prolonged hospital stay and additional healthcare staff and medical equipment for monitoring. Combining other analgesic drugs like ketamine and fentanyl with sedatives such as propofol reduces the dose required to produce adequate sedation and pain control while minimizing the significant side effects. Tramadol is also effective in relieving pain during the procedure with the added benefit of significantly reducing pain caused specifically by marrow aspiration and minimal adverse effects. Methoxyflurane is another agent able to reduce aspiration-related pain but has a higher incidence of adverse effects. Entonox is a potent analgesic gas that can be self-administered before and during the biopsy and is efficacious in minimizing pain during the procedure with minimal side effects. These methods provide pain control to varying degrees during the procedure. Pain control after BMBx is an under-explored area that may be a topic of future research interest. Evidence suggests that benzodiazepines and Entonox do provide pain relief not only during but also in the post-procedural period.
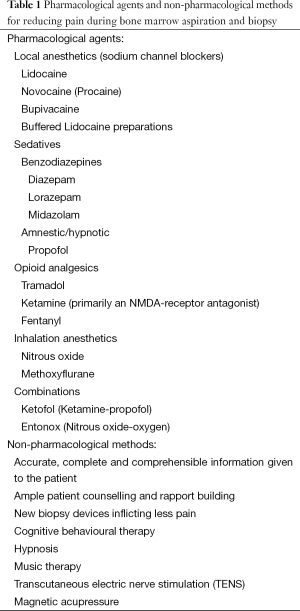
Non-pharmacological factors also play an important role in influencing pain during BMBx and are potential opportunities that can be used to minimize pain. Providing a patient with complete and comprehensible information can allow them to better anticipate what the entire process involves and better cope with and handle the pain associated with the procedure. Using devices that allow for specimen collection with minimal manipulation of the needle when inside the marrow cavity reduces pain associated with this specific step of the BMBx. The Goldenberg snare-coil needle is an example of such a device. Other techniques, such as hypnosis, CBT, music therapy etc. that provide distractions to patients can help them focus off the pain during the procedure and hence lead to better pain control. However, the effectiveness of these techniques greatly varies according to the kind of patient they are employed on. TENS and magnetic acupressure have also proven to be effective adjuvants to LA in providing pain relief during BMBx. All strategies for reducing pain during BMBx that have been tested are grouped together in Table 1.
Full table
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Hjortholm N, Jaddini E, Hałaburda K, et al. Strategies of pain reduction during the bone marrow biopsy. Ann Hematol 2013;92:145-9. [PubMed]
- Talamo G, Liao J, Bayerl MG, et al. Oral administration of analgesia and anxiolysis for pain associated with bone marrow biopsy. Support Care Cancer 2010;18:301-5. [PubMed]
- Birch CD, Fischer S, Zibell A, et al. Diagnostic bone-marrow studies extended routinely by iliac crest biopsy, using the method of Schaadt-Fischer. Acta Pathol Microbiol Immunol Scand A 1982;90:229-34. [PubMed]
- Ellis LD, Jensen WN, Westerman MP. Needle biopsy of bone and marrow; an experience with 1,445 biopsies. Arch Intern Med 1964;114:213-21. [PubMed]
- Jamshidi K, Windschitl HE, Swaim WR. A new biopsy needle for bone marrow. Scand J Haematol 1971;8:69-71. [PubMed]
- Watmough S, Flynn M. A review of pain management interventions in bone marrow biopsy. J Clin Nurs 2011;20:615-23. [PubMed]
- Bichel J. Serious complications of sternal puncture. Ugeskr Laeger 1989;151:442-4. [PubMed]
- Pascali VL, Lazzaro P, Fiori A. Is sternal bone marrow needle biopsy still a hazardous technique? Report of three further fatal cases. Am J Forensic Med Pathol 1987;8:42-4. [PubMed]
- Riley RS, Hogan TF, Pavot DR, et al. A pathologist’s perspective on bone marrow aspiration and biopsy: I. Performing a bone marrow examination. J Clin Lab Anal 2004;18:70-90. [PubMed]
- Hernández-García MT, Hernández-Nieto L, Pérez-González E, et al. Bone marrow trephine biopsy: anterior superior iliac spine versus posterior superior iliac spine. Clin Lab Haematol 1993;15:15-9. [PubMed]
- Bain BJ. Bone marrow trephine biopsy. J Clin Pathol 2001;54:737-42. [PubMed]
- Steinke B. Complications after bone marrow biopsy. Dtsch Med Wochenschr 1992;117:1003-4. [PubMed]
- Degen C, Christen S, Rovo A, et al. Bone marrow examination: a prospective survey on factors associated with pain. Ann Hematol 2010;89:619-24. [PubMed]
- Kuball J, Schuz J, Gamm H, et al. Bone marrow punctures and pain. Acute Pain 2004;6:9-14.
- Vanhelleputte P, Nijs K, Delforge M, et al. Pain during bone marrow aspiration: prevalence and prevention. J Pain Symptom Manage 2003;26:860-6. [PubMed]
- Bain BJ. Bone marrow biopsy morbidity and mortality. Br J Haematol 2003;121:949-51. [PubMed]
- Knowles S, Hoffbrand AV. Bone-marrow aspiration and trephine biopsy (1). Br Med J 1980;281:204-5. [PubMed]
- Johnson H, Burke D, Plews C, et al. Improving the patient’s experience of a bone marrow biopsy - an RCT. J Clin Nurs 2008;17:717-25. [PubMed]
- Brunetti GA, Tendas A, Meloni E, et al. Pain and anxiety associated with bone marrow aspiration and biopsy: a prospective study on 152 Italian patients with hematological malignancies. Ann Hematol 2011;90:1233-5. [PubMed]
- Audran M, Maury E, Bouvard B, et al. Is transiliac bone biopsy a painful procedure? Clin Nephrol 2012;77:97-104. [PubMed]
- Jensen NF, Fiddler DS, Striepe V. Anesthetic considerations in porphyrias. Anesth Analg 1995;80:591-9. [PubMed]
- Gall H, Kaufmann R, Kalveram CM. Adverse reactions to local anesthetics: analysis of 197 cases. J Allergy Clin Immunol 1996;97:933-7. [PubMed]
- Kuivalainen AM, Niemi-Murola L, Widenius T, et al. Comparison of articaine and lidocaine for infiltration anaesthesia in patients undergoing bone marrow aspiration and biopsy. Eur J Pain 2010;14:160-3. [PubMed]
- Holdsworth MT, Raisch DW, Winter SS, et al. Pain and distress from bone marrow aspirations and lumbar punctures. Ann Pharmacother 2003;37:17-22. [PubMed]
- Ruegg TA, Curran CR, Lamb T. Use of buffered lidocaine in bone marrow biopsies: a randomized, controlled trial. Oncol Nurs Forum 2009;36:52-60. [PubMed]
- Kuivalainen AM, Ebeling F, Rosenberg P. Warmed and buffered lidocaine for pain relief during bone marrow aspiration and biopsy. A randomized and controlled trial. Scand J Pain 2014;5:43-7.
- Milligan DW, Howard MR, Judd A. Premedication with lorazepam before bone marrow biopsy. J Clin Pathol 1987;40:696-8. [PubMed]
- Friedman AG, Mulhern RK, Fairclough D, et al. Midazolam premedication for pediatric bone marrow aspiration and lumbar puncture. Med Pediatr Oncol 1991;19:499-504. [PubMed]
- Chakupurakal G, Delgado J, Nikolousis E, et al. Midazolam in conjunction with local anaesthesia is superior to Entonox in providing pain relief during bone marrow aspirate and trephine biopsy. J Clin Pathol 2008;61:1051-4. [PubMed]
- Park SH, Bang SM, Nam E, et al. A randomized double-blind placebo-controlled study of low-dose intravenous Lorazepam to reduce procedural pain during bone marrow aspiration and biopsy. Pain Med 2008;9:249-52. [PubMed]
- Giannoutsos I, Grech H, Maboreke T, et al. Performing bone marrow biopsies with or without sedation: a comparison. Clin Lab Haematol 2004;26:201-4. [PubMed]
- Mainwaring CJ, Wong C, Lush RJ, et al. The role of midazolam-induced sedation in bone marrow aspiration/trephine biopsies. Clin Lab Haematol 1996;18:285-8. [PubMed]
- Dunlop TJ, Deen C, Lind S, et al. Use of combined oral narcotic and benzodiazepine for control of pain associated with bone marrow examination. South Med J 1999;92:477-80. [PubMed]
- Fay M, Murphy PT. Sedation with intravenous midazolam and intravenous opiate is superior to intravenous midazolam alone for bone marrow biopsy procedures. Clin Lab Haematol 2004;26:365. [PubMed]
- Chiaretti A, Ruggiero A, Barbi E, et al. Comparison of propofol versus propofol-ketamine combination in pediatric oncologic procedures performed by non-anesthesiologists. Pediatr Blood Cancer 2011;57:1163-7. [PubMed]
- Habibi MR, Hasanzadeh Kiabi F, Soleimani A, et al. Sedation and analgesia during bone marrow aspiration in children: Is ketamine and propofol combination (Ketofol) an appropriate agent? Indian J Med Paediatr Oncol 2013;34:337-9. [PubMed]
- da Silva PS, de Aguiar VE, Waisberg DR, et al. Use of ketofol for procedural sedation and analgesia in children with hematological diseases. Pediatr Int 2011;53:62-7. [PubMed]
- Daabiss M, Elsherbiny M, Alotibi R. Assessment of different concentration of Ketofol in procedural operation. BJMP 2009;2:27-31.
- Hashemi A, Ayatolahi V, Ghilian R, et al. Ketofol for bone marrow aspiration and lumbar puncture in children with ALL. Iran J Ped Hematol Oncol 2011;1:126-32.
- Ghadami Yazdi A, Ayatollahi V, Hashemi A, et al. Effect of two Different Concentrations of Propofol and Ketamine Combinations (Ketofol) in Pediatric Patients under Lumbar Puncture or Bone Marrow Aspiration. Iran J Ped Hematol Oncol 2013;3:187-92. [PubMed]
- Anghelescu DL, Burgoyne LL, Faughnan LG, et al. Prospective randomized crossover evaluation of three anesthetic regimens for painful procedures in children with cancer. J Pediatr 2013;162:137-41. [PubMed]
- Burkle CM, Harrison BA, Koenig LF, et al. Morbidity and mortality of deep sedation in outpatient bone marrow biopsy. Am J Hematol 2004;77:250-6. [PubMed]
- Becker DE, Haas DA. Management of complications during moderate and deep sedation: respiratory and cardiovascular considerations. Anesth Prog 2007;54:59-68. [PubMed]
- Mendelson WB, Thompson C, Franko T. Adverse reactions to sedative/hypnotics: three years’ experience. Sleep 1996;19:702-6. [PubMed]
- Desmeules JA. The tramadol option. Eur J Pain 2000;4 Suppl A:15-21.
- Scott LJ, Perry CM. Tramadol: a review of its use in perioperative pain. Drugs 2000;60:139-76. [PubMed]
- Kuivalainen AM, Ebeling F, Rosenberg PH. Pre-medication with sublingual fentanyl did not relieve pain associated with bone marrow aspiration and biopsy: a randomized feasibility trial. Eur J Pain 2013;17:1357-64. [PubMed]
- Kanagasundaram SA, Lane LJ, Cavalletto BP, et al. Efficacy and safety of nitrous oxide in alleviating pain and anxiety during painful procedures. Arch Dis Child 2001;84:492-5. [PubMed]
- Gudgin EJ, Besser MW, Craig JI. Entonox as a sedative for bone marrow aspiration and biopsy. Int J Lab Hematol 2008;30:65-7. [PubMed]
- Steedman B, Watson J, Ali S, et al. Inhaled nitrous oxide (Entonox) as a short acting sedative during bone marrow examination. Clin Lab Haematol 2006;28:321-4. [PubMed]
- Spruyt O, Westerman D, Milner A, et al. A randomised, double-blind, placebo-controlled study to assess the safety and efficacy of methoxyflurane for procedural pain of a bone marrow biopsy. BMJ Support Palliat Care 2014;4:342-8. [PubMed]
- Kliman D, Rugg L, Bailey S, et al. A prospective assessment of Methoxyflurane and other analgesic agents during bone marrow biopsy. Pathology-Journal of the RCPA 2014;46:S94. Available online: http://journals.lww.com/pathologyrcpa/Abstract/2014/02001/A_PROSPECTIVE_ASSESSMENT_OF_METHOXYFLURANE_AND.260.aspx
- Goldenberg AS, Rishton M. Bone-marrow biopsy needle incorporating a snare-coil specimen-capturing device: description and preclinical studies. Biomed Instrum Technol 1999;33:522-9. [PubMed]
- Goldenberg AS, Tiesinga JJ. Clinical experience with a new specimen capturing bone marrow biopsy needle. Am J Hematol 2001;68:189-93. [PubMed]
- Reed LJ, Raghupathy R, Strakhan M, et al. The OnControl bone marrow biopsy technique is superior to the standard manual technique for hematologists-in-training: a prospective, randomized comparison. Hematol Rep 2011;3:e21. [PubMed]
- Cohen SC, Gore JM. Evaluation of a powered intraosseous device for bone marrow sampling. Anticancer Res 2008;28:3843-6. [PubMed]
- Berenson JR, Yellin O, Blumenstein B, et al. Using a powered bone marrow biopsy system results in shorter procedures, causes less residual pain to adult patients, and yields larger specimens. Diagn Pathol 2011;6:23. [PubMed]
- Miller LJ, Philbeck TE, Montez DF, et al. Powered bone marrow biopsy procedures produce larger core specimens, with less pain, in less time than with standard manual devices. Hematol Rep 2011;3:e8. [PubMed]
- Swords RT, Anguita J, Higgins RA, et al. A prospective randomised study of a rotary powered device (OnControl) for bone marrow aspiration and biopsy. J Clin Pathol 2011;64:809-13. [PubMed]
- Liossi C, Hatira P. Clinical hypnosis versus cognitive behavioral training for pain management with pediatric cancer patients undergoing bone marrow aspirations. Int J Clin Exp Hypn 1999;47:104-16. [PubMed]
- Accardi MC, Milling LS. The effectiveness of hypnosis for reducing procedure-related pain in children and adolescents: a comprehensive methodological review. J Behav Med 2009;32:328-39. [PubMed]
- Snow A, Dorfman D, Warbet R, et al. A randomized trial of hypnosis for relief of pain and anxiety in adult cancer patients undergoing bone marrow procedures. J Psychosoc Oncol 2012;30:281-93. [PubMed]
- Morgan AH, Hilgard ER. Age differences in susceptibility to hypnosis. Int J Clin Exp Hypn 1973;21:78-85.
- Shabanloei R, Golchin M, Esfahani A, et al. Effects of music therapy on pain and anxiety in patients undergoing bone marrow biopsy and aspiration. AORN J 2010;91:746-51. [PubMed]
- Tucker DL, Rockett M, Hasan M, et al. Does transcutaneous electrical nerve stimulation (TENS) alleviate the pain experienced during bone marrow sampling in addition to standard techniques? A randomised, double-blinded, controlled trial. J Clin Pathol 2015;68:479-83. [PubMed]
- Bao T, Ye X, Skinner J, et al. The analgesic effect of magnetic acupressure in cancer patients undergoing bone marrow aspiration and biopsy: a randomized, blinded, controlled trial. J Pain Symptom Manage 2011;41:995-1002. [PubMed]


