Editor’s note:
“Surgical Palliative Care Column” features articles relating to incorporating the precepts and techniques of palliative care into surgical clinical practice, education, research, and advocacy. Serving as chairs to the column, Dr. Geoffrey P. Dunn (University of Pittsburgh Hamot Medical Center, USA) and Dr. Anne C. Mosenthal (Rutgers New Jersey Medical School, USA) gather surgeons interested in the field of palliative care to make the column more informative and educated. Original articles, timely review articles, perspectives, editorials and commentaries on recently published trials and studies, etc. are welcomed in the column.
Utilization of palliative care consultation service by surgical services
Introduction
Palliative medicine is specialized medical care for patients with serious and advanced illness. The primary aim of palliative care is to improve the quality of life of both patients and their families through the appropriate relief of symptoms and the stress that serious illness entails (1). Palliative care is commonly equated with end-of-life care; however, palliative care is appropriate for patients at any stage of serious illness and can be provided along with curative-intent treatment. Defined in this way, palliative care is appropriate for many patients with surgical disease.
Although the American College of Surgeons has worked to improve knowledge and integration of palliative care among surgeons since 1998 (2), there remain significant knowledge gaps and lack of referral to palliative care by surgeons (3,4). Bradley et al. sought to increase palliative care consultations in a surgical intensive care unit (ICU) through the use of triggers to prompt palliative care consultation (5). They found that palliative care consultations were rare, both before and after the institution of triggers for consultations. A recent study of trauma surgeons found that approximately half of those surveyed felt that palliative care was underutilized (4). It is unclear if this finding is true among the broader range of surgical services.
A preliminary review of our palliative care consultation database revealed that consultations from surgical services comprise only 15% of the total consultations received by our multidisciplinary palliative medicine team. The goal of the current study was to examine the characteristics of surgical patients who received palliative care consultations and compare them to medical patients who received palliative care consultations during the same period of time. Based upon the results of the current study, we hoped to identify potential barriers to consultation and opportunities to improve utilization of palliative care consultation services (PCCS) among surgical services.
Materials and methods
The Palliative Medicine Division at the University of New Mexico was created in 2009 and consists of an interdisciplinary team of physicians board-certified in Hospice & Palliative Medicine as well as nurse practitioners, a social worker, a chaplain, and Arts-in-Medicine providers. A prospectively maintained database of patients who received inpatient PCCS from 2009-2013 was queried. Stratified random sampling methodology was utilized to derive the study population (6). This methodology involves dividing the overall study population (all patients referred for palliative care consultation) into two strata: those referred from surgical services or from medical services. Once it was determined that 15% of all referrals came from surgical services between 2009 and 2013, the final study population was chosen at random to ensure that the final population was proportional to the size of these two strata. After removal of duplicates and randomization of cases, a total of 521 charts where included for review. The study was approved by the University of New Mexico Institutional Review Board.
The following data were collected on all subjects: general demographic variables, date of hospital admission, date of palliative care consultation, referring service (medical vs. surgical), hospital location of patient at the time of palliative care consultation, reason for palliative care consultation, number of days under palliative consultation, do-not-resuscitate (DNR) status before and after palliative care consultation, date of hospital discharge, and disposition of patient upon hospital discharge. Patients were stratified according to referring service.
Descriptive statistics was used to calculate frequencies, percentages and means of study variables. Continuous variables were analyzed with independent sample t-test. Categorical variables were analyzed with Fischer’s exact test or chi-square test, as appropriate. To evaluate the influence of palliative care consultation on code status, McNemar’s test for paired data was used. All P values recorded were for two-tailed tests, P value ≤0.05 was considered statistically significant. Data analysis was performed with SPSS™ Version 21.0 (IMB Corp., Armonk, NY, USA).
Results
Demographic characteristics
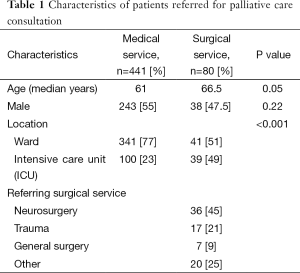
A total of 521 patients referred for PCCS were analyzed: 441 patients referred by medical services, 80 patients referred by surgical services.
Demographic characteristics of medical vs. surgical patients are summarized in Table 1. Medical patients tended to be younger compared to patients referred from surgical services. Although the majority of patients referred to PCCS were located outside of an ICU (73%), patients referred from surgical services were more likely to be in an ICU at the time of consultation compared to patients referred from medical services. Almost half of all patients referred by a surgical service were referred from the neurosurgery service.
Full table
Characteristics of palliative care consultations
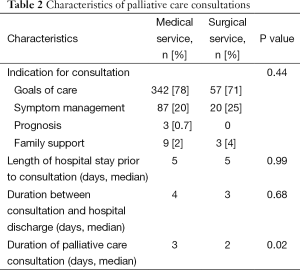
Characteristics of PCCS by referring service are shown in Table 2. More than 70% of referrals from both medical and surgical services were to establish goals of patient care. Patients from both services were referred to PCCS after a median of 5 days of in-hospital stay. There was no difference between the two groups in time from PCCS to hospital discharge. Patients referred by medical services were followed by the PCCS longer than patients referred by surgical services.
Full table
Patient disposition
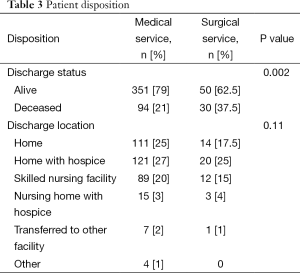
Table 3 summarizes patient outcome following PCCS. There was no difference between the groups in terms of patient disposition following hospital discharge. However, a larger proportion of patients referred to PCCS by surgical services died in-hospital compared to patients referred by medical services. There was no difference between the two groups in the percentage who were discharged with hospice services (medical: 31%, surgical: 29%).
Full table
Impact of palliative care consultation on code status
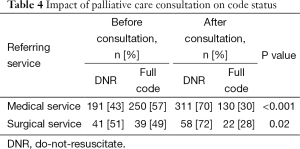
The impact of PCCS on code status among patients referred by medical versus surgical services is shown in Table 4. Forty-four percent of all patients had a DNR order in place before PCCS. The percentage of patients with DNR orders prior to PCCS did not vary between referring services (P=0.19). After PCCS, the percentage of patients with DNR orders increased significantly in both referring services.
Full table
Discussion
Palliative care is medical care focused on improving the quality of life in patients with serious and advanced illness. Since its recognition as a defined medical subspecialty in 2006, palliative medicine has seen a rapid expansion of palliative care services available to a wide variety of patients (7). The increased integration of palliative care services has not been seen across all medical disciplines, however. Despite the American College of Surgeons Statement of Principles Guiding Care at the End-of-Life originally published in 1998 and later revised to support the provision of palliative care services to a broader range of surgical patients, surgical patients often do not receive palliative care services (2,8). The disparity in utilization of PCCS between medical and surgical services was identified in our own institution; surgical services constitute only 15% of all referrals to the PCCS. The current study sought to compare utilization of PCCS among surgical vs. medical services.
Compared to patients referred by medical services, patients referred from surgical services tended to be older and more likely to be in an ICU. The fact that surgical patients were older may reflect a bias on the part of surgeons to consult palliative care for patients with a perceived reduced chance for recovery and/or increased perceived risk for dying. This hypothesis is supported by the fact that surgical patients referred for PCCS were more likely to be in an ICU at the time of consultation and, therefore, more critically ill than those referred by medical services. Over half of surgical patients had a DNR order in place at the time of PCCS compared to 43% of patients from medical services. Furthermore, surgical patients had a higher in-hospital mortality (37.5%) compared to medical patients (21%) (P=0.002). Taken together, these results suggest a (mis)perception that palliative care is reserved for patients at end-of-life.
Two recent studies provide insight as to why surgeons may delay or defer palliative care consultation for their patients. In a study of nine trauma and neurosurgeons, Tilden et al. sought to identify attitudes and practices regarding palliative care consultation in their population of patients with sudden and advanced illness (9). They found that surgeons were less likely to consult palliative medicine when they believed the patient would die early in their hospital course or if the patient would likely survive. Conversely, surgeons were more likely to consult palliative medicine when they believed the patient would eventually die from their injury or if they would progress to a chronic condition and were not showing signs of progress. A survey of 358 trauma surgeons found that the single greatest perceived benefit of palliative care consultation was assistance with end-of-life issues, again highlighting the misperception that palliative care is primarily reserved for patients at end-of-life. In the same study, nearly one-third of surgeons did not consult palliative medicine due to concern that it would indicate that the surgeon was “giving up” on the patient (4). Both of these studies reflect the “cure culture” that dominates in surgery; the tendency to initiate palliation only after all curative options have been exhausted. The drive toward cure and continuation of aggressive interventions may also be spurred on by the increasing focus on surgical 30-day mortality statistics which may encourage some surgeons to pursue quantity over quality of life and other more appropriate surgical quality metrics (10). In the ICU, in particular, there exists an apparent dichotomy between the interventions designed to support life and pain associated with these interventions (11).
An alternative explanation for the increased rate of PCCS for surgical patients in the ICU compared to consults from the medical service may be a reflection of several recent studies specifically focused on the benefits of palliative care consultation for ICU patients. The most notable of these efforts has been the Improving Palliative Care in the ICU (IPAL-ICU) Project (12). Although not yet validated in a surgical ICU population, use of triggers for palliative care consultation has been advocated (13). One retrospective study using ten previously identified potential triggers for palliative care consultation in a surgical ICU revealed that only 5% of patients met the criteria for consultation based upon the triggers and did not significantly change the number of palliative care consultations (5). Additionally, use of these triggers for consultation did not alter the time from trigger to consultation or the rate of consultation for surgical ICU patients dying in the hospital. In contrast, a more recent study by Sihra et al. found that institution of a screening protocol for patients who may benefit from PCCS resulted in an increase in palliative care consults of 113% in the medical ICU and increase of 51% in consults from the surgical ICU during an eight month screening period (14).
The tendency for surgeons to reserve palliative care consultations for their most critically ill and those with a perceived low likelihood of survival highlights the need for increased education in surgical palliative care. In 2009, Dunn provided a comprehensive overview of the core competencies of surgical palliative care (15). Unfortunately, despite increasing awareness and availability of palliative care services, a recent study by Amini et al. of surgical oncology and hepatobiliary fellows found that fellows’ training in palliative care was poor compared to the training they received in other aspects of their fellowship (16). A study of surgical residents in Japan revealed that a significant proportion of surgical trainees lacked the knowledge or ability to manage common symptoms such as management of cancerous pain, respiratory symptoms, or digestive tract symptoms (17). Efforts are currently underway to establish a palliative care curriculum for surgical trainees which will be a critical step toward remediating these educational deficiencies.
In the current study, patients (or their surrogates) were more likely to change their code status from full code to DNR following PCCS. Recent literature has shown that palliative care significantly impacts patients’ decision to elect DNR status (18). After reviewing palliative care consultations over a 5-year period, Bell and colleagues found that palliative care consultation was strongly associated with code status change. Patients who received a palliative care consultation to establish goals of care had a 3-fold increase in changing their code status to DNR. A study of older patients with end-stage cancer or advanced medical illness found that those who felt that end-of-life issues were relevant to them were 5.5 times more likely to want to discuss resuscitation with their physician (19). These results are consistent with those in the current study that indicate that palliative care consultation has a significant impact on clarifying patients’ wishes regarding cardiopulmonary resuscitation.
There are several limitations to the current study. The study is based upon on a randomized sample implying that results may not completely reflect what may be observed the population as a whole. Furthermore, while the results of the current study may apply to our particular institution, we cannot be certain that our findings can be generalizable to other hospital practices where different models of treatment and referral may exist.
Our results indicate that there appears to be an opportunity to increase PCCS among surgical patients, specifically among younger patients and those outside of an ICU setting. The current pattern of referral suggests a potential misconception that PCCS is primarily useful for those with critical illness and/or at end-of-life as evidenced by the significant percentage of surgical patients who died prior to discharge and already had a DNR order in place at the time of PCCS. Although triggers for palliative care consultation have not consistently been shown to increase palliative care consultations among surgical patients in an ICU, triggers or some other means of screening surgical patients outside of the ICU for palliative care needs may identify opportunities to improve symptom management and relieve the burden of serious illness among surgical patients. Whether the presence a surgeon with palliative care expertise leads to an increase in overall, or earlier, referral for PCCS among surgical services is the focus of a current investigation.
Acknowledgements
The authors wish to acknowledge Venita Wolfe, MS for her assistance in maintaining the University of New Mexico Palliative Medicine Consultation database.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Sepúlveda C, Marlin A, Yoshida T, et al. Palliative Care: the World Health Organization's global perspective. J Pain Symptom Manage 2002;24:91-6. [PubMed]
- Statement on principles guiding care at the end of life. American College of Surgeons' Committee on Ethics. Bull Am Coll Surg 1998;83:46. [PubMed]
- Klaristenfeld DD, Harrington DT, Miner TJ. Teaching palliative care and end-of-life issues: a core curriculum for surgical residents. Ann Surg Oncol 2007;14:1801-6. [PubMed]
- Karlekar M, Collier B, Parish A, et al. Utilization and determinants of palliative care in the trauma intensive care unit: results of a national survey. Palliat Med 2014;28:1062-8. [PubMed]
- Bradley C, Weaver J, Brasel K. Addressing access to palliative care services in the surgical intensive care unit. Surgery 2010;147:871-7. [PubMed]
- Berenson ML, Levine DM, Krehbiel TC. Basic Business Statistics: Concepts and Applications (10th Edition). New Jersey: Prentice Hall, 2005.
- Center to Advance Palliative Care and the National Palliative Care Research Center. National Palliative Care Registry TM Annual Survey Summary. Results of the 2012 National Palliative Care Registry TM Survey, as of July 2014. Available online: https://registry.capc.org/cms/portals/1/Reports/Registry_Summary%20Report_2014.pdf, accessed on Jun 29, 2015.
- Task Force on Surgical Palliative care, Committee on Ethics. Statement of principles of palliative care. Bull Am Coll Surg 2005;90:34-5.
- Tilden LB, Williams BR, Tucker RO, et al. Surgeons' attitudes and practices in the utilization of palliative and supportive care services for patients with a sudden advanced illness. J Palliat Med 2009;12:1037-42. [PubMed]
- Schwarze ML, Brasel KJ, Mosenthal AC. Beyond 30-day mortality: aligning surgical quality with outcomes that patients value. JAMA Surg 2014;149:631-2. [PubMed]
- Mosenthal AC, Lee KF, Huffman J. Palliative care in the surgical intensive care unit. J Am Coll Surg 2002;194:75-83; discussion 83-5. [PubMed]
- Mosenthal AC, Murphy PA. Interdisciplinary model for palliative care in the trauma and surgical intensive care unit: Robert Wood Johnson Foundation Demonstration Project for Improving Palliative Care in the Intensive Care Unit. Crit Care Med 2006;34:S399-403. [PubMed]
- Bradley CT, Brasel KJ. Developing guidelines that identify patients who would benefit from palliative care services in the surgical intensive care unit. Crit Care Med 2009;37:946-50. [PubMed]
- Sihra L, Harris M, O'Reardon C. Using the improving palliative care in the intensive care unit (IPAL-ICU) project to promote palliative care consultation. J Pain Symptom Manage 2011;42:672-5. [PubMed]
- Dunn GP. Principles and core competencies of surgical palliative care: an overview. Otolaryngol Clin North Am 2009;42:1-13. vii. [PubMed]
- Amini A, Miura JT, Larrieux G, et al. Palliative care training in surgical oncology and hepatobiliary fellowships: a national survey of the fellows. Ann Surg Oncol 2015;22:1761-7. [PubMed]
- Oya H, Matoba M, Murakami S, et al. Mandatory palliative care education for surgical residents: initial focus on teaching pain management. Jpn J Clin Oncol 2013;43:170-5. [PubMed]
- Bell CL, Kuriya M, Fischberg D. Hospice referrals and code status: outcomes of inpatient palliative care consultations among Asian Americans and Pacific Islanders with cancer. J Pain Symptom Manage 2011;42:557-64. [PubMed]
- Heyland DK, Frank C, Groll D, et al. Understanding cardiopulmonary resuscitation decision making: perspectives of seriously ill hospitalized patients and family members. Chest 2006;130:419-28. [PubMed]


