
The effects of the 45° semi-recumbent position on the clinical outcomes of mechanically ventilated patients: a systematic review and meta-analysis study
Introduction
Invasive mechanical ventilation (MV) has become a common adjuvant treatment modality in the intensive care unit (ICU). However, this technique requires tracheotomy or direct access to the trachea, which can increase the incidence of ventilator-associated pneumonia (VAP) (1). The occurrence of VAP prolongs the ventilation time required and greatly increases the risk of mortality (2), which can be as high as 13.0–25.2% (3). In the 1990s, it was demonstrated that body position is closely related to the occurrence of VAP, and bed head elevation at a certain angle can significantly reduce the incidence of VAP. A multi-centered observational study showed that the majority of mechanically ventilated patients are positioned with their head-of-bed angle at less than 30° (4). However, study (5) revealed that with the position less than 30 it was very likely to increase the risk of VAP and mortality during the primary treatment of ventilation. Another randomized controlled trial (RCT) research (6) revealed that ventilated patients with a semi-recumbent position can reduce reflux of contaminated gastric contents and aspiration. A meta-analysis study by Wang et al. (7) was conducted to compare semi-recumbent position (45°) with 25° to 30° position in the outcomes of VAP, mortality, length of ICU stay, the results show not significant between the two, but there is only two trials included in the study and the GRADE showed very low quality evidence. In this study, more trials were included in the meta-analysis to provide more strong evidence for the 45° semi-recumbent position of mechanically ventilated patients.
We present the following article in accordance with the PRISMA reporting checklist (available at https://dx.doi.org/10.21037/apm-21-2359).
Methods
Database and search strategy
This study refers to PRISMA 2020 standard. The medical databases PubMed, Embase, and the Cochrane library were searched using the following keywords alone or in combination: “45°”, “head-of-bed elevation”, “semi-recumbent”, “backrest”, “head elevation”, “ICU”, “ventilation”, and “ventilator”. The filter was set by using the filtering function of the database. Reports of RCTs with full text articles published between 2005 and 2021 were included.
Inclusion and exclusion criteria of the selected literature
Inclusion criteria
The following inclusion criteria were applied to the included literature: (I) all patients were aged 18 years and older and were treated in the ICU with MV to support respiration; (II) the intervention must include a group of patients given MV in the 45° bed head elevation angle, with adjustments not greater than 5°, and a control group treated at the 30° bed head elevation angle (other control groups might be included, such as a 0° group, but would not included in the final analysis); (III) the duration of bed head elevation must be identical for both the intervention group and the control group; (IV) the outcome indicators included VAP incidence rate, gastric reflux incidence rate, pressure sores incidence rate, ventilation indicators, ventilation time, mortality, length of hospital stay, and other indicators.
Exclusion criteria
The following articles were excluded: (I) non-randomized studies, studies or observational studies, investigations, case analysis, reviews, guidelines, systematic reviews, etc; (II) literatures with repeated study contents with others; and (III) literatures with missing data, or data that could not be transformed and/or used.
Literature quality evaluation
The Jadad scoring criteria were used to evaluate the quality of the included randomized controlled studies. The quality of the literatures were scored, and the evaluation process was independently completed by two researchers, If there was any disagreement during the process, a third researcher was resorted. A score of less than 3 presented a low-quality literature, and a score greater than 3 presented a high-quality literature.
Literature screening
Two researchers independently searched the database for the studies. The retrieval results were combined with replicative check, preliminary screening was performed by reading the title and the abstracts. Studies were further screened by reviewing the full-text articles applying the inclusion and exclusion criteria. Quality evaluations were performed on the remaining studies and those with scores of less than 3 were excluded.
Bias assessment
The Cochrane review handbook was used to assess the bias of the studies, including the following six aspects: (I) the random sequence generation; (II) the allocation concealment; (III) the blinding method; (VI) the outcome assessment; (V) the incomplete outcome data; and (IV) other bias. Any disagreement between the two researchers were resolved via discussion and consultation with a third investigator.
Data extraction
Studies that met the inclusion and exclusion criteria were summarized and the basic characteristics were collated, including authors, publication year and month, sample size, characteristics of the study subjects, intervention methods, outcome measures.
Statistical methods
All data were analyzed using the RevMan 5.3.5 software. The enumeration data such as VAP incidence rate, gastric reflux incidence rate, and pressure sores incidence rate, were reported using an odds ratio (OR) value and 95% confidence interval (CI). P value <0.05 was considered statistically significant. The heterogeneity of the studies was examined by I2 analysis and Q check. Analyses with I2>25% or P<0.1 suggested significant heterogeneity and the random-effects model would be used, otherwise, the fixed effects model was used. If heterogeneity was suggested among the studies, sensitivity analysis was performed using a case-by-case elimination method. Funnel plots were used to present publication bias.
Results
Literature screening results
Initially, 128 literatures were identified from the database searches. Following a review of the titles and the abstracts, non-randomized controlled studies, repeated studies, and studies with missing intervention methods and incomplete data were excluded. Finally, 7 literatures, with a total of 740 patients, were included in this meta-analysis, the selection process was shown in (Figure 1), and the characteristics of included literatures were shown in (Table 1).
Table 1
| Author | Year | Region | Study subjects | Total samples (T/C) | Age (years) (T/C) | Intervention mode (T/C) | Outcome measures | Jadad score |
|---|---|---|---|---|---|---|---|---|
| Ghezeljeh et al. (8) | 2017 | Iran | ICU mechanically ventilated patients | 80 (40/40) | 64.7/65.7 | T: head of bed elevation angle 45° (lasting for 3 d); C: head of bed elevation angle 30° (lasting for 3 d) | VAP incidence rate, pressure sores incidence rate | 4 |
| Schallom et al. (9) | 2015 | NA | ICU mechanically ventilated patients | 15 (8/7) | NA | T: head of bed elevation angle 45° (lasting for 2 d); C: head of bed elevation angle 30° (lasting for 2 d) | VAP incidence rate, gastric reflux incidence rate, pressure sores incidence rate | 5 |
| Güner et al. (10) | 2021 | NA | ICU mechanically ventilated patients | 40 (20/20) | NA | T: head of bed elevation angle 45° (lasting for 5 d); C: head of bed elevation angle 30° (lasting for 5 d) | VAP incidence rate | 4 |
| Göcze et al. (11) | 2013 | Germany | Hemodynamically stable ICU MV | 100 (50/50) | 60.0/60.5 | T: head of bed elevation angle 45° (lasting for 1 d); C: head of bed elevation angle 30° (lasting for 1 d) | MAP, ScvO2, incidence of hypotension | 4 |
| van Nieuwenhoven et al. (12) | 2006 | The Netherlands | Mechanically ventilated patients | 221 (112/109) | 64.8/63.0 | T: head of bed elevation angle 45° (lasting for 7 d); C: head of bed elevation angle 30° (lasting for 7 d) | VAP incidence rate, gastric reflux incidence rate, length of hospital stay, mortality | 5 |
| Li et al. (13) | 2015 | China | Mechanically ventilated patients | 238 (119/119) | NA | T: head of bed elevation angle 45°; C: head of bed elevation angle 30° | VAP incidence rate, gastric reflux incidence rate, pressure sores incidence rate | 5 |
| Jiang et al. (14) | 2016 | China | Mechanically ventilated patients | 46 (23/23) | 68.0/70.6 | T: head of bed elevation angle 45° (lasting for 7 d); C: head of bed elevation angle 30° (lasting for 7 d) | VAP incidence rate, pressure sores incidence rate, arterial oxygen index | 5 |
T, intervention group; C, control group; NA, not available; ICU, intensive care unit; MV, mechanical ventilation; VAP, ventilator-associated pneumonia; MAP, mean arterial pressure; ScvO2, central venous oxygen saturation.
Quality evaluation of the included literature
Quality assessment and bias analysis were performed using the Cochrane System for Randomized Intervention Evaluation criteria (Figures 2,3). There were two publications in which the description of random sequence generation was unclear and there might result in selective bias. One literature had unclear concealment method and there might be selective bias. Three articles had unclear blinding method and there might be operational bias.
Meta-analysis results
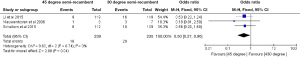
The incidence of VAP
There were six articles that included the incidence of VAP as an outcome indicator. Meta-analysis revealed that these literatures showed statistical homogeneity (I2=0%; P=0.88). The fixed effects model demonstrated a significant difference between the 45° group and the 30° control group in terms of the incidence of VAP (OR =0.48; 95% CI: 0.28 to 0.84; Z=2.59; P=0.009; Figure 4).

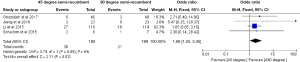
The incidence of gastric reflux
The three studies that documented the incidence of gastric reflux in the outcome measures showed statistical homogeneity (I2=0%; P=0.74). The fixed effects model revealed statistically significant differences between the 45° group and the 30° control group in terms of the incidence of gastric reflux (OR =0.50; 95% CI: 0.27 to 0.96; Z=2.09; P=0.04; Figure 5).
The incidence of pressure sores
The four studies that reported the incidence of pressure sores showed statistical homogeneity (I2=0%; P=0.85). The fixed effects model showed a statistically significant difference between the 45° group and the 30° control group in terms of the incidence of pressure sores (OR =1.88; 95% CI: 1.05 to 3.36; Z=2.11; P=0.03; Figure 6).
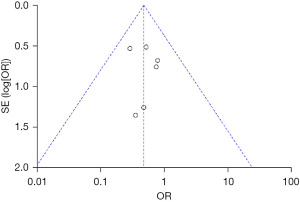
Analysis of sensitivity and publication bias
Some literatures contained unclear descriptions regarding the random sequence generation and the blinding method, and this may have contributed to bias in the synthesis results. However, all synthesis results showed statistical homogeneity, and thus, sensitivity analysis were not conducted. The funnel plot in Figure 7 shows an uneven distribution in the two groups, suggesting that there may be publication bias.
Discussion
Although the Center for Disease Control and Prevention recommends that mechanically ventilated patients remain in the 45° position to reduce the risk of VAP, there is still a lack of strong evidence supporting this position in the practical clinical setting (15). Our meta-analysis examined a total of 740 patients across 7 qualified publications and found that the incidence of VAP in patients with a 45° angle supine position was significantly lower than that observed in patients with a 30° angle supine position, suggesting that the 45° angle semi-recumbent position was sufficient to reduce the incidence of VAP. Furthermore, the incidence of gastric reflux was significantly reduced in patients with a 45° semi-recumbent position compared to patients with a 30° supine position. Reflux of gastric contents and subsequent microaspiration of bacterial contaminate the oropharyngeal fluids and lead to the development of VAP, but a combination of nasogastric feeding tube and the supine position prevents gastroesophageal reflux and increases the volume of oropharyngeal fluids significantly (16). With the 45° recumbent position, the gastric contents refluxing rate are reduced, followed by a reduction of bacterial colonization in the oropharynx, thereby reducing the possibility of infections (17). However, the elevation angle of the bed head inevitably increases the pressure on the sacrococcygeal skin contact surface, which increases the risk of pressure sores (18). This meta-analysis revealed that there was a significant difference in the incidence of pressure sores between the 45° semi-recumbent position and the 30° position, suggesting that the 45° semi-recumbent position was more prone to inducing pressure sores, which meant that patients should change their position more often than the 30° position (most probably every 2 hours).
In addition, although raising the head of the bed to 45° is a simple method for the prevention of VAP, it is very difficult to maintain this position. In a survey on semi-sitting positions, only 26.4% of bedridden patients were able to maintain an elevation angle of more than 30° (19). Some studies have also suggested that the lack of sufficient comfort, fear of pressure ulcers, frequent change of position are all the factors effecting the adherence to 45° position (20). Therefore, the decision to adopt a bedside elevation of 45° should be determined based on the patient’s condition and physical tolerance. Several guidelines from the American Thoracic Society, the Infectious Diseases Society of America, and others have recommended the semi-recumbent positioning with an elevation head-of-bed angle of 30° to 45°, which implying an angle slightly lower than 45° might be the best choice for the patients who could not endure the fully 45° recumbent position (21). Besides, nurses need knowledge and education about the 45° recumbent position, a precise adjustment and permanent monitoring of the slope of bed using electronic devices may help maintaining the elevation of head of bed (HOB) to 45 degrees due to the degree wasn’t always that accurate (22).
In this study, RevMan software was used to analyze the publication bias of seven documents. Both sides of the funnel plot showed asymmetry, suggesting that there may be selective literature publication bias. In addition, analysis of the three indicators showed homogeneity among the studies, which may be due to the limited number of randomized trials in this meta-analysis preventing the detection of heterogeneity between literatures, and thus, resulting in bias in the results. As there is currently no fixed criteria for VAP diagnosis in clinical practice, there may be a bias in the statistics of VAP. The included literatures also had problems such as unclear random sequence generation method, unclear blinding method, and unclear hidden method, which may pose a risk of bias to the final results. Future work should include more RCTs to enable in-depth analysis of this topic.
Conclusions
The 45° semi-recumbent position is effective for reducing the incidence VAP, but it may also increase the risk of pressure sores. Future research should focus on methods to maintain the continuity of the 45° semi-recumbent position, and developing management regimens to reduce the incidence of pressure sores.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://dx.doi.org/10.21037/apm-21-2359
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/apm-21-2359). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Marklin GF, O'Sullivan C, Dhar R. Ventilation in the prone position improves oxygenation and results in more lungs being transplanted from organ donors with hypoxemia and atelectasis. J Heart Lung Transplant 2021;40:120-7. [Crossref] [PubMed]
- Kurihara M, Nishimura S. Estimation of the head elevation angle that causes clinically important venous air embolism in a semi-sitting position for neurosurgery: a retrospective observational study. Fukushima J Med Sci 2020;66:67-72. [Crossref] [PubMed]
- Martinez BP, Marques TI, Santos DR, et al. Influence of different degrees of head elevation on respiratory mechanics in mechanically ventilated patients. Rev Bras Ter Intensiva 2015;27:347-52. Erratum in: Rev Bras Ter Intensiva 2016;28:96. [Crossref] [PubMed]
- ve BK. Cook DJ. Semirecumbency among mechanically ventilated ICU patients: A multicenter observational study. Clinical Intensive Care 1999;10:241-4. [Crossref]
- Fernández-Crehuet R, Díaz-Molina C, de Irala J, et al. Nosocomial infection in an intensive-care unit: identification of risk factors. Infect Control Hosp Epidemiol 1997;18:825-30. [PubMed]
- Torres A, Serra-Batlles J, Ros E, et al. Pulmonary aspiration of gastric contents in patients receiving mechanical ventilation: the effect of body position. Ann Intern Med 1992;116:540-3. [Crossref] [PubMed]
- Wang L, Li X, Yang Z, et al. Semi-recumbent position versus supine position for the prevention of ventilator-associated pneumonia in adults requiring mechanical ventilation. Cochrane Database Syst Rev 2016;2016:CD009946 [Crossref] [PubMed]
- Ghezeljeh TN, Kalhor L, Moghadam OM, et al. The comparison of the effect of the head of bed elevation to 30 and 45 degreess on the incidence of ventilator associated pneumonia and the risk for pressure ulcers: a controlled randomized clinical trial. Iran Red Crescent Med J 2017;19:e14224 [Crossref]
- Schallom M, Dykeman B, Metheny N, et al. Head-of-bed elevation and early outcomes of gastric reflux, aspiration and pressure ulcers: a feasibility study. Am J Crit Care 2015;24:57-66. [Crossref] [PubMed]
- Güner CK, Kutlutürkan S. Role of head-of-bed elevation in preventing ventilator-associated pneumonia bed elevation and pneumonia. Nurs Crit Care 2021; Epub ahead of print. [Crossref] [PubMed]
- Göcze I, Strenge F, Zeman F, et al. The effects of the semirecumbent position on hemodynamic status in patients on invasive mechanical ventilation: prospective randomized multivariable analysis. Crit Care 2013;17:R80. [Crossref] [PubMed]
- van Nieuwenhoven CA, Vandenbroucke-Grauls C, van Tiel FH, et al. Feasibility and effects of the semirecumbent position to prevent ventilator-associated pneumonia: a randomized study. Crit Care Med 2006;34:396-402. [Crossref] [PubMed]
- Li FQ, Gao S, Yang Y, et al. Effects of different mechanical angles of semirecumbent positions on critically ill patients undergoing ventilation. Chinese Journal of Nosocomiology 2015;25:4911-3.
- Jiang QX, Liu J, Liu YX, et al. Effects of semirecumbent positions of different degrees on mechanical ventilation and prevention of complications for ventilated patients. Journal of Medical Postgraduates 2016;29:1083-8.
- Leng YX, Song YH, Yao ZY, et al. Effect of 45 degree angle semirecumbent position on ventilator-associated pneumonia in mechanical ventilated patients: a meta-analysis. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue 2012;24:587-91. [PubMed]
- Villamil Morales IM, Gallego Ospina DM, Otero Regino WA. Impact of head of bed elevation in symptoms of patients with gastroesophageal reflux disease: a randomized single-blind study (IBELGA). Gastroenterol Hepatol 2020;43:310-21. [Crossref] [PubMed]
- Palazzo P, Brooks A, James D, et al. Risk of pneumonia associated with zero-degree head positioning in acute ischemic stroke patients treated with intravenous tissue plasminogen activator. Brain Behav 2016;6:e00425 [Crossref] [PubMed]
- Yeon DY, Yoo C, Lee TE, et al. Effects of head elevation on intraocular pressure in healthy subjects: raising bed head vs using multiple pillows. Eye (Lond) 2014;28:1328-33. [Crossref] [PubMed]
- Vinagre Gaspar R, Morales Sánchez C, Frade Mera MJ, et al. Evaluation of the compliance of semirecumbent position between 30-45° in intubated patients. Enferm Intensiva 2011;22:117-24. [Crossref] [PubMed]
- Lyerla F, LeRouge C, Cooke DA, et al. A nursing clinical decision support system and potential predictors of head-of-bed position for patients receiving mechanical ventilation. Am J Crit Care 2010;19:39-47. [Crossref] [PubMed]
- American Thoracic Society. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 2005;171:388-416. [Crossref] [PubMed]
- Wolken RF, Woodruff RJ, Smith J, et al. Observational study of head of bed elevation adherence using a continuous monitoring system in a medical intensive care unit. Respir Care 2012;57:537-43. [PubMed]
(English Language Editor: J. Teoh)





