
A systematic review and meta-analysis of risk factors in the conservative treatment of cesarean scar pregnancy
Introduction
Cesarean scar pregnancy (CSP) is a special ectopic pregnancy in which the gestational sac implants at the scar of the lower uterine segment cesarean incision. Its villi adhere to and implant at the scar and can penetrate the uterine layer, resulting in uterine rupture, causing massive hemorrhage and endangering the patient’s life (1). In the last decade, with the worldwide use of cesarean section, the incidence of CSP has shown an increasing trend (2). At present, the pathogenesis of CSP is not clear in the academic community, and some studies (3) suggest that the poor healing of the cesarean scar results in a cleft between it and the endometrium, which may create conditions for ectopic implantation of the gestational sac. Ultrasound examination is an important tool for the early CSP diagnosis, in addition, there is still a lack of clear guidance for the treatment of CSP, which needs to be comprehensively considered according to the patient’s fertility requirements, condition, age, and other realistic conditions (4). In view of the possible risks caused by CSP, it is generally recommended to terminate pregnancy after diagnosis and perform conservative treatment, which including uterine curettage, scar repair, and other treatment methods. However, data (5) shows that the failure rate of the conservative treatment of CSP can be up to 44.1%. Once conservative treatment fails, patients may develop serious complications such as massive hemorrhage and uterine rupture, and hysterectomy surgery has to be performed to save the patient’s life, which makes the patient infertile (6). Therefore, it is important to investigate the risk factors of the failure of conservative treatment for CSP in order to determine the right treatment method, reduce the treatment complications and mortality, and preserve the fertility of patients. In this study, we analyzed the risk factors of conservative treatment failure by means of evidence-based medicine to provide an objective basis for clinical practice. We present the following article in accordance with the PRISMA reporting checklist (available at https://dx.doi.org/10.21037/apm-21-2169).
Methods
Literature search databases
The literature language was limited to English. PubMed, MEDLINE, Embase, and the Cochrane Library database were selected as the databases for this study.
Search strategy
The keywords were in the Embase database: “cesarean pregnancy” AND “treatment” with quick search method. In other databases, the advanced search method was used. The search keywords were: “cesarean” AND “scar” AND “pregnancy”, or “cesarean” AND “ectopic scar” AND “pregnancy” AND “methotrexate”, or “CSP” AND “scar”, or “CSP” AND “uterine artery embolization”, or “CSP” AND “surgery”. All articles found should be published after January 2005.
Inclusion criteria
The literature met the following criteria: (I) all articles were observational studies, including cohort studies, cross-sectional surveys, case-control studies, time series studies, case series reports, and other types, and did not limit the number of centers in the study; (II) the study subjects were female patients definitely diagnosed with CSP; (III) the conservative treatment methods of CSP were reported in the study: drug treatment or uterine curettage, or a combination of the 2, which was to preserve the fertility of patients; (IV) the study provided the criteria for conservative treatment failure, including β-hCG not reduced to the normal range within 90 days, massive vaginal bleeding, and the need to undergo laparotomy (or laparoscopic surgery) to remove the uterine lesions; (V) the study indicated the number of successful and failed conservative treatment cases; (VI) the study had detailed records for the data before and after treatment, including the basic data of patients before treatment (age, number of cesarean sections, β-hCG value, ultrasound type) and observation indicators after treatment (complications such as whether there was massive hemorrhage, whether there was uterine rupture, and the days required for the β-hCG value to return to normal).
Exclusion criteria
The literature exclusion criteria were as follows: (I) reviews, case analyses, heterogeneity studies, investigations, which are not observational studies; (II) lacking observation indicators.
Literature screening
The literature search was completed by two researchers who worked independently. The recorded information of the retrieved articles included title, publication date, author. The full texts of the articles were obtained, and repeated articles were excluded. Preliminary screening for the literature was conducted by reading the abstracts of the articles, and articles that obviously did not meet the requirements were excluded. If there was uncertainty, the full texts of the articles were read, and they were screened one by one according to the inclusion and exclusion criteria. In case of any disagreement or doubt about the literature, or the information was not complete, the original author should be contacted to obtain comprehensive information, or the information should be included first and then determined in the subsequent quality analysis.
Data extraction
The included articles were collated, and the basic information of the articles were extracted and recorded using excel tables, including the study characteristics and observation indicators. This work was independently completed by two researchers, and if the data of the two researchers were inconsistent during the final verification, it was evaluated and arbitrated by a third researcher.
Data items
The data of outcome items included the total number of patients who received conservative treatment and the number of patients who failed conservative treatment, the age of patients before treatment, the number of pregnancies, the number of cesarean sections, preoperative blood pressure, β-hCG value, ultrasound type, fetal heart beat, gestational time from cesarean section interval. If the data was missing, the article was excluded.
Literature quality assessment
The Newcastle-Ottawa Scale (NOS) (7) was used to analyze the quality of the included literatures. The scale was used to evaluate subject selection, comparability, and the outcome indicators of the literatures. The maximum score was 9 points, and a score of more than 5 points was considered to be good quality. The higher the score was, the better the quality of the article was, and the bias of the article was less.
Statistical analysis
The RevMan 5.3.5 software package was used for statistical analysis. The Q statistic test was used to determine heterogeneity between studies. P>0.05 indicated no heterogeneity and good consistency. Fixed effect model analysis was used to calculate odd ratio (OR) by the Mantel-Haenszel method. If heterogeneity existed, random effect model analysis was used to calculate OR by the Der Simonian and Laird method. All of the above effect analyses considered P<0.1 as statistically significant. The article by article exclusion method was used to conduct the sensitivity analyses of literatures with heterogeneity. The effect analysis was presented in the form of a forest plot, while the publication bias was displayed using an inverted funnel plot, If the results of fixed effect analysis and random effect analysis were consistent, this indicated that the synthesis results were stable.
Results
Literature search and screening results
In this study, 1,538 relevant articles were initially found, including 522 single case reports, 387 reviews, 238 clinical trial studies, and 391 documents. After screening by the inclusion and exclusion criteria, 56 articles were left. After quality evaluation, articles with a score <5 were removed. A total of 7 articles were left for final analysis, as shown in Figure 1. A total of 251 cases were involved, of which 79 cases failed conservative treatment, accounting for 31.5%. The quality scores of the 7 articles were all above 5, but there might have been bias. The basic characteristics, common risk factors, and the quality scores of the documents are shown in Table 1.
Table 1
| Author | Total cases | Number of failures | Age (years) | Number of pregnancies | Number of cesarean sections (times) | Serum β-hCG value (10,000× U/L) | Ultrasonic classification | Presence of fetal heart beat | Interval between pregnancy and cesarean section (years) | Quality score (points) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <35 | ≥35 | <3 | ≥3 | 1 | ≥2 | <2 | ≥2 | Gestational sac type | Mass CSP | None | Yes | <3 | ≥3 | ||||||||||
| Deb et al. [2007] (8) | 20 | 6 | 15 | 5 | 14 | 6 | – | – | – | – | 12 | 8 | – | – | – | – | 5 | ||||||
| Timor-Tritsch et al. [2012] (9) | 13 | 4 | 6 | 7 | 7 | 6 | 8 | 5 | 6 | 7 | 5 | 8 | 5 | 8 | – | – | 7 | ||||||
| Zhu et al. [2015] (10) | 44 | 15 | 21 | 23 | 31 | 13 | – | – | 12 | 32 | 17 | 27 | 31 | 13 | – | – | 6 | ||||||
| Boza et al. [2016] (11) | 76 | 24 | 41 | 35 | 55 | 21 | 57 | 19 | 26 | 50 | 36 | 40 | – | – | – | – | 6 | ||||||
| Yang et al. [2016] (12) | 55 | 17 | 25 | 30 | – | – | 30 | 25 | 23 | 32 | 25 | 30 | 23 | 32 | 31 | 24 | 7 | ||||||
| Kelekçi et al. (2014) (13) | 18 | 6 | 5 | 13 | – | – | 11 | 7 | – | – | 12 | 6 | – | – | 11 | 7 | 6 | ||||||
| Jachymski et al. [2020] (14) | 25 | 7 | 13 | 12 | – | – | 14 | 11 | – | – | – | – | – | – | 13 | 12 | 5 | ||||||
CSP, cesarean scar pregnancy.
Meta-analysis results
Patient age
All 7 studies reported the number of cases of conservative treatment failure for patients at different age levels. A total of 126 cases were younger than 35 years old and 125 cases were older than 35 years old. There was no heterogeneity between the studies (I2=0%, P=0.70). The fixed effect model analysis showed that there was no significant difference in the failure rate of conservative treatment between the two groups of patients at different age levels [OR =1.25, 95% CI: (0.87, 1.79), P=0.23]. The results of fixed effect analysis and random effect analysis were consistent, indicating that the results of the sensitivity analysis were stable, as shown in Figure 2.
Number of pregnancies
A total of 4 studies reported the number of cases of conservative treatment failure in patients with different numbers of pregnancies, including 46 patients with more than 3 pregnancies and 107 patients with less than 3 pregnancies. There was no statistical heterogeneity between the studies (I2=48%, P=0.12). The fixed effect model analysis showed that there was no significant difference in the failure rate of conservative treatment between the two groups of patients with different numbers of pregnancies [OR =0.91, 95% CI: (0.43, 1.89), P=0.79], as shown in Figure 3.
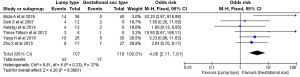
Number of cesarean sections
A total of 5 articles reported the number of conservative treatment failures in patients with different numbers of cesarean sections. There were 67 patients with more than 2 cesarean sections and 120 patients with only 1 cesarean section. There was no statistical heterogeneity between the studies (I2=0%, P=0.77). The fixed effect model analysis showed that the failure rate of conservative treatment was higher in patients with more than 2 cesarean sections [OR =1.79, 95% CI: (0.94, 3.42), P=0.08], as shown in Figure 4.
Serum β-hCG value
A total of 4 articles reported the number of treatment failures in patients with different preoperative serum β-hCG values, including 121 patients with serum β-hCG values <20,000 U/L and 67 patients with serum β-hCG values ≥20,000 U/L. There was no statistical heterogeneity between the studies (I2=0%, P=0.89). Fixed effect model analysis was used to analyze the failure rate of conservative treatment in patients with serum β-hCG values <20,000 U/L was higher [OR =1.81, 95% CI: (0.92, 3.54), P=0.09], as shown in Figure 5.
Ultrasonic classification of scars
A total of 4 articles reported the number of conservative treatment failures in patients with different ultrasonic classifications of scars, including 107 cases of gestational sac type and 119 cases of mass type. There was no statistical heterogeneity between the studies (I2=27%, P=0.23). The failure rate of conservative treatment in patients with type obtained by fixed effect model analysis [OR =4.06, 95% CI: (2.11, 7.81), P<0.0001], as shown in Figure 6.
Presence or absence of fetal heart beat
A total of 3 articles reported the number of treatment failures in patients with different fetal heart beats, including 53 patients with fetal heart beats and 59 patients without fetal heart beats. There was no statistical heterogeneity between the studies (I2=0%, P=0.79). The fixed effect model analysis showed that there was no significant difference in the failure rate of conservative treatment between the two groups [OR =1.04, 95% CI: (0.46, 2.37), P=0.93], as shown in Figure 7.
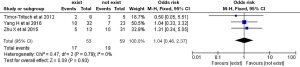
Time interval between pregnancy and cesarean section
A total of 3 articles reported the number of treatment failures in patients with different cesarean section time intervals, including 55 cases with pregnancy time more than 3 years from the last cesarean section and 43 cases with pregnancy time less than 3 years. There was no statistical heterogeneity between the studies (I2=28%, P=0.25). The failure rate of the conservative treatment was higher in patients with pregnancy intervals more than 3 years from the last cesarean section determined by fixed effect model analysis [OR =4.12, 95% CI: (1.29, 13.08), P=0.02], as shown in Figure 8.

Analysis of publication bias
The publication bias analysis was performed for the above factors with statistically significant differences, and the funnel plot was basically symmetrical, as shown in Figure 9 (ultrasound classification).
Discussion
WHO statistics (15) showed that the cesarean section rate in Asia reached 48.9% in 2010. Over time, a study (16) showed that the cesarean section rate had an increasing trend, reaching up to 50% in some hospital and the popularity of cesarean section increases the risk of CSP. Since there is no uniform treatment plan for CSP, the treatment methods may be quite different according to different individual cases, and the treatment complications also show great differences. In the study by Timor-Tritsch et al. (17), the author pointed out that curettage and systemic methotrexate therapy and embolization as single treatments should be avoided if possible, transvaginal- or transabdominal guided local and ultrasound-directed methotrexate injection and hysteroscopic directed procedures had the lowest complication rates; the curettage treatment could lead to profuse bleeding and loss of the uterus, and systemic methotrexate may not prevent embryonic development, the uterine artery embolization should be used only as a rescue procedure.
In this study, the occurrence of serious complications (massive hemorrhage, uterine rupture) and failure to reduce the β-hCG level to the normal range within 90 days were classified as treatment failure, and the risk factor analysis was performed on the basis of evidence-based medicine. Meta-analysis showed that the risk factors associated with the failure of conservative treatment of CSP were the number of cesarean sections, serum β-hCG value, ultrasound classification, and time interval from pregnancy to cesarean section, while there was no significant difference in the age of patients, the number of pregnancies, and the presence or absence of fetal heart beat for the failure of conservative treatment of CSP.
The number of cesarean sections will affect the conservative treatment effect of CSP. With more cesarean sections, the destruction of the endometrium will be more serious, the healing of the scar will be more difficult. The gestational trophoblasts produced by the gestational sac at the scar site will invade the uterine tissue, the embryonic villous tissue will also adhere to the uterus during growth and development and even invade and penetrate the entire uterus, resulting in uterine rupture and massive hemorrhage, which greatly increases the risk of conservative treatment (18). In this study, 5 studies reported a total of 67 patients who underwent cesarean section more than twice and 120 patients who underwent cesarean section only once. The results of meta-analysis showed that there was a statistical difference in the failure rate of conservative treatment of CSP between the two groups. The failure rate of more than 2 cesarean sections was high [OR =1.79, 95% CI: (0.94, 3.42), P=0.08], and the results were consistent with the study by Naji et al. (19).
In this study, it was also found that ultrasound classification was a factor contributing to conservative treatment failure of CSP. The treatment failure rate of mass type was higher than that of the gestational sac type, and the difference was statistically significant [OR =4.06, 95% CI: (2.11, 7.81), P=0.0001]. The reason for this is that mass type CSP is deeply buried in the scar site, and during embryonic development, it is very likely to cause uterine rupture and form massive hemorrhage due to penetration into the muscle (20). Therefore, if the patient has mass type CSP during ultrasonography, the patients should be informed of the risks in a timely manner, and surgical treatment should be considered first.
Meta-analysis also showed that the failure rate of conservative treatment in patients with serum β-hCG value <20,000 U/L was higher than patients with serum β-hCG value ≥20,000 U/L [OR =1.81, 95% CI: (0.92, 3.54), P=0.09], suggesting that a higher serum β-hCG value is a protective factor for conservative treatment. The β-hCG values are stably incrementing after conception in women, and if the increment rate slows down, it predicts abnormal embryonic development or ectopic pregnancy (21). Therefore, regular monitoring of β-hCG values is required to guide subsequent conservative treatment.
In this study, there were 55 cases with pregnancy time more than 3 years after the last cesarean section, while 43 cases had pregnancy time less than 3 years. Meta-analysis found that the failure rate of conservative treatment in patients with pregnancy time over 3 years after last cesarean section was higher [OR =4.12, 95% CI: (1.29, 13.08), P=0.02]. The reason was that the scar tissue structure would change gradually over time, the extensibility would be reduced, and that will halt the scar’s healing process, which add the odds of treatment failure. In the study by Belachew et al. (22), it was pointed out that the timing of re-pregnancy was the best at an interval of 2 to 5 years from the last cesarean section, which could effectively reduce the chance of conservative treatment failure.
This study did not find an effect of patient age, number of pregnancies, and fetal heart beat on the outcome of conservative treatment of CSP. In addition, some important factors such as the size of the pregnancy sac and the thickness of the anterior wall of the uterus were not included in the statistical analysis because no sufficient evidence was retrieved in the literature. In the quality evaluation of the literature, it was found that the studies might have certain selection and measurement biases. However, the bias analysis performed for the factors (ultrasonic classification) with more included literature finally found that the 2 sides of the funnel plot were basically symmetrical, indicating that there was no publication bias.
Conclusions
In this meta-analysis of the risk factors for conservative treatment failure of CSP, a total of 7 studies were included. The results showed that more than 2 cesarean sections, mass type CSP, serum β-hCG value <20,000 U/L, and pregnancy more than 3 years from the last cesarean section were risk factors for the failure of conservative treatment of CSP. Patients with the above risk factors should be screened and informed of the possibility of conservative treatment failure in a timely manner, and different treatment methods should be considered comprehensively.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://dx.doi.org/10.21037/apm-21-2169
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/apm-21-2169). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Riaz RM, Williams TR, Craig BM, et al. Cesarean scar ectopic pregnancy: imaging features, current treatment options, and clinical outcomes. Abdom Imaging 2015;40:2589-99. [Crossref] [PubMed]
- Jurkovic D, Ben-Nagi J, Ofilli-Yebovi D, et al. Efficacy of Shirodkar cervical suture in securing hemostasis following surgical evacuation of Cesarean scar ectopic pregnancy. Ultrasound Obstet Gynecol 2007;30:95-100. [Crossref] [PubMed]
- Kim K, Pietrzak A, Gonzalez S, et al. Severe hemorrhage in a first-trimester cesarean scar pregnancy during dilation and curettage. Int J Obstet Anesth 2010;19:348-9. [Crossref] [PubMed]
- Tian H, Li S, Jia W, et al. Risk factors for poor hemostasis of prophylactic uterine artery embolization before curettage in cesarean scar pregnancy. J Int Med Res 2020;48:300060520964379 [Crossref] [PubMed]
- Kochhar PK, Sarangal M, Gupta U. Conservative management of cesarean scar pregnancy with uterine arteriovenous malformation: a case report. J Reprod Med 2013;58:81-4. [PubMed]
- Li X, Sun W, Chen L, et al. Cesarean scar pregnancy combined with arteriovenous malformation successfully treated with transvaginal fertility-sparing surgery: A case report and literature review. Medicine (Baltimore) 2020;99:e21432 [Crossref] [PubMed]
- Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603-5. [Crossref] [PubMed]
- Deb S, Clewes J, Hewer C, et al. The management of Cesarean scar ectopic pregnancy following treatment with methotrexate--a clinical challenge. Ultrasound Obstet Gynecol 2007;30:889-92. [Crossref] [PubMed]
- Timor-Tritsch IE, Monteagudo A, Santos R, et al. The diagnosis, treatment, and follow-up of cesarean scar pregnancy. Am J Obstet Gynecol 2012;207:44.e1-13. [Crossref] [PubMed]
- Zhu X, Deng X, Wan Y, et al. High-intensity focused ultrasound combined with suction curettage for the treatment of cesarean scar pregnancy. Medicine (Baltimore) 2015;94:e854 [Crossref] [PubMed]
- Boza A. Md, Boza B Md, Api M Md PhD. Cesarean Scar Pregnancy Managed with Conservative Treatment. Iran J Med Sci 2016;41:450-5. [PubMed]
- Yang H, Li S, Ma Z, et al. Therapeutic effects of uterine artery embolisation (UAE) and methotrexate (MTX) conservative therapy used in treatment of cesarean scar pregnancy. Arch Gynecol Obstet 2016;293:819-23. [Crossref] [PubMed]
- Kelekçi S, Aydoğmuş S, Aydoğmuş H, et al. Ineffectual Medical Treatment of Cesarean Scar Ectopic Pregnancy With Systemic Methotrexate: A Report of Two Cases. J Investig Med High Impact Case Rep 2014;2:2324709614528903 [Crossref] [PubMed]
- Jachymski T, Moczulska H, Guzowski G, et al. Conservative treatment of abnormally located intrauterine pregnancies (cervical and cesarean scar pregnancies): a multicenter analysis (Polish series). J Matern Fetal Neonatal Med 2020;33:993-8. [Crossref] [PubMed]
- Lumbiganon P, Laopaiboon M, Gülmezoglu AM, et al. Method of delivery and pregnancy outcomes in Asia: the WHO global survey on maternal and perinatal health 2007-08. Lancet 2010;375:490-9. [Crossref] [PubMed]
- Yang C, Ouyang D. Variation trend and influential factors for cesarean section rate in a general hospital in Changsha from 2008 to 2017. Zhong Nan Da Xue Xue Bao Yi Xue Ban 2019;44:334-7. [PubMed]
- Timor-Tritsch IE, Monteagudo A. Unforeseen consequences of the increasing rate of cesarean deliveries: early placenta accreta and cesarean scar pregnancy. A review. Am J Obstet Gynecol 2012;207:14-29. [Crossref] [PubMed]
- Li H, Guo HY, Han JS, et al. Endoscopic treatment of ectopic pregnancy in a cesarean scar. J Minim Invasive Gynecol 2011;18:31-5. [Crossref] [PubMed]
- Naji O, Wynants L, Smith A, et al. Does the presence of a Caesarean section scar affect implantation site and early pregnancy outcome in women attending an early pregnancy assessment unit? Hum Reprod 2013;28:1489-96. [Crossref] [PubMed]
- Stevens EE, Ogburn P. Cesarean scar ectopic pregnancy: a case report of failed combination local and systemic methotrexate management requiring surgical intervention. J Reprod Med 2011;56:356-8. [PubMed]
- Yamaguchi M, Honda R, Honda T, et al. Transvaginal methotrexate injection is effective for the treatment of cesarean scar pregnancy despite hCG levels. Placenta 2015;36:A8-A9. [Crossref]
- Belachew J, Cnattingius S, Mulic-Lutvica A, et al. Risk of retained placenta in women previously delivered by caesarean section: a population-based cohort study. BJOG 2014;121:224-9. [Crossref] [PubMed]
(English Language Editor: C. Betlazar-Maseh)








