
Systematic review and meta-analysis of the effects of group painting therapy on the negative emotions of depressed adolescent patients
Introduction
According to the China Youth Development Report, about 30 million children and adolescents under 17 years of age in China are suffering from various emotional disorders and behavioral problems; however, the overall rate of consultation is less than 1/3 of this number (1). Multiple studies have shown that during adolescence there is a substantial increase in the incidence of mood disorders that is second only to behavioral disorders (2-4). Adolescent depression, which is one of the most common emotional disorders in adolescence, refers to depression in adolescents (5). The main clinical symptoms include apathy, complaints of pain, difficulty concentrating, difficulty making decisions, excessive feelings of guilt, irresponsible behavior, a lack of interest in food or compulsive overeating resulting in rapid weight loss or gain, forgetfulness, fear of death and end-of-life, rebellious behavior, feelings of sadness, anxiety or despair, sleeplessness at night, and excessive daytime sleep (6). In relation to the etiology of depression, some studies have found that genetic factors are the main reasons for the continuous development of depression in early adolescence (7). However, the dominant factor for the sustained development of depression among adolescents in mid-adolescence is environmental factors (8).
At present, the treatment methods for adolescent depression include drug therapy, cognitive behavioral therapy, and combination therapy (9). However, there are few drugs for adolescent depression, and many antidepressants are not suitable for people under 14 years old. Therefore, cognitive behavior therapy is widely used in the treatment of adolescent depression, and art treatment is one of them. Group painting therapy is one of the methods for psychological art treatment, which enables painters to present the repressed feelings and conflicts in the subconscious through the creative process of painting and using non-verbal tools, and obtain the expression and satisfaction in the process of painting, so as to achieve a good effect of diagnosis and treatment (10). Both adults and children can present a complete performance between the two dimensions, and can meet the psychological needs in the process of “appreciating oneself”.
In recent years, there have been reports related to the application of group painting therapy to the treatment of psychological diseases among teenagers in China and abroad (11). However, the sample size of patients included in most articles is small, and the sample is relatively single, most of which are conducted in a certain hospital or a certain area as the center. Therefore, different research results can’t be consistent. At present, there is no sound theoretical basis for systematic evaluation of the effect of clinical group painting on the negative emotions of adolescent depression in China. In this study, the meta-analysis was used to comprehensively analyze the impact of group painting on the negative emotions of adolescent depression patients based on the references on the treatment of adolescent depression by group painting published since the establishment of the database, so as to provide a reliable reference for further guiding the clinical treatment of adolescent depression. We present the following article in accordance with the PRISMA reporting checklist (available at https://dx.doi.org/10.21037/apm-21-2474).
Methods
Literature searching
China Biomedical Literature Database, Wanfang Database, VIP Database, Baidu Academic, CMCI, Medline, Embase, and PubMed were searched for articles on randomized controlled trials (RCTs) on the effects of group painting therapy (GPT) on adolescent depression published between the establishment of the databases and March 15, 2021. The relevant articles were selected using the Boolean logic retrieval method of compound logic. The Chinese databases were searched using a combination of search terms, such as “adolescent”, “juvenile”, “minor”, “depression”, “excessive anxiety”, “affective disorder”, “selective mutism”, “neurosis”, “group painting therapy”, “art therapy”, and “negative emotion”. The English databases were searched using a combination of search terms, such as “adolescent depression”, “panic attack specifier”, “Group painting therapy”, “art therapy”, “overanxious disorder”, “Negative emotions”, “depress”, “dysthymia”, “mood disorder”, “selective mutism”, “avoidant disorder”, “affective disorder”, “anxiety”, “anxious”, “panic disorder”, “agoraphobia”, “combat disorder”, “mixed disorder”, and “neurosis”. The quality of the retrieved articles was evaluated using the Cochrane system (RevMan 5.3).
The above literature search terms were freely combined to identify the included references after multiple searches, and then the search engine was used to determine the literature tracing. Experts and researchers in the field were contacted for updates on the latest research progress.
Literature inclusion and exclusion criteria
To be eligible for inclusion in this meta-analysis, the articles had to meet the following inclusion criteria: (I) the subjects comprised adolescents (aged 13–18 years old); (II) the study was a RCT; (III) the subjects did not have an organic brain injury, physical injury, or serious chronic disease; (IV) the diagnostic criteria for the experimental group included the American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders, Diagnostic and Statistical Manual of Mental Disorders (DSM-IV), and the International Classification of Diseases and Related Health Problems (ICD-10), and the subjects’ anxiety or depression symptom scale scores were above the diagnostic thresholds; (V) all the subjects had signed the informed consent form.
Articles were excluded from the meta-analysis, if they met any of the following exclusion criteria: (I) the studies did not include a randomized control group; (II) the patients had other mental disorders (e.g., schizophrenia or bipolar disorder); (III) the patients had psychotic depression or treatment-resistant depression, or the research object was a special population, and age and gender were restricted; (IV) the article was about a repeatedly published study; (V) the article was a conference speech, literature review, case study report, lecture, or critical literature; (VI) complete data for the study could not be obtained; (VII) the study examined the effects of GPT combined with antidepressants.
The abstract and full text of each article were screened by two senior experts, and three pre-experiments were conducted in advance of the screening. In case of dissension, consensus conclusions were reached through discussion among the experts.
Observation indicators
The negative emotions of depressed adolescent patients were tested by a number of scales, including the general situation survey form, the positive and negative affect scale (PANAS), the Connor-Davidson resilience scale (CD-RISC), the self-esteem scale (SES), the Wisconsin card sorting test (WCST) [which includes the number of correct responses (Re) and the number of continuous responses (Rp)], the MATRICS consensus cognitive battery (MCCB) [which includes a language memory test (HVLT-R), a visual memory test (BVMT-R), and a maze test (NAB-Mazes)], and an emotion management test (MSCEIT-ME).
Data extraction
Two experts used unified Microsoft Excel to independently extract the data, and 3 pre-experiments were conducted before data extraction. When there was a disagreement between the 2 experts, a consensus was reached via discussion. The data extracted included: (I) the study title; (II) the name of the first author and the publication year; (III) the title of the publication; (IV) the research design types; (V) general information about the subjects, including region, sample size, gender, and age; (VI) the evaluation indexes.
Risk of bias and quality assessment
Risk of bias was assessed by two researchers simultaneously. If the two researchers disagreed, the results were determined via discussion. Quality was evaluated using recommendations from the National Institute of Clinical Excellence (NICE). The specific quality assessment items are set out in Table 1. Two researchers made a quality judgment of “high risk bias”, “low risk bias”, and “unclear” for the entries in Table 1, and then compared the consistency of the judgment results, and if the opinion was no agreement, the consistency evaluation was obtained through discussion. The score of low risk evaluation result for each entry in Table 1 was 1, while high risk bias and unclear were not scored, and the scores ranged from 0 to 8. If the final score was 6–8, the included literature was judged to be a high-quality study, if the final score was 3–6, the included literature was judged to be a medium-quality study, and if the final score was 0–2, the included literature was judged to be a low-quality study.
Table 1
| Serial number | Item | Evaluation results |
|---|---|---|
| 1 | Cases were selected from different levels of medical institutions and studied at multiple centers | (I) High-risk bias; (II) low-risk bias; (III) unclear-risk bias |
| 2 | The main purpose of the study was clearly described | (I) High-risk bias; (II) low-risk bias; (III) unclear-risk bias |
| 3 | The inclusion and exclusion criteria were strict | (I) High-risk bias; (II) low-risk bias; (III) unclear-risk bias |
| 4 | Clear definition of the study’s measurements were provided | (I) High-risk bias; (II) low-risk bias; (III) unclear-risk bias |
| 5 | The data collected should meet the expected metrics. | (I) High-risk bias; (II) low-risk bias; (III) unclear-risk bias |
| 6 | The patients enrolled were continuously recruited | (I) High-risk bias; (II) low-risk bias; (III) unclear-risk bias |
| 7 | The main findings of the study were described in detail | (I) High-risk bias; (II) low-risk bias; (III) unclear-risk bias |
| 8 | A hierarchical analysis of outcome indicators was performed, and the results were reported | (I) High-risk bias; (II) low-risk bias; (III) unclear-risk bias |
Statistical methods
The statistical analysis was performed using StataSE 12.0 (College Station, USA). The risk of bias of each included article was assessed using the bias-risk assessment diagram of RevMan 5.3. Each effect was expressed using a 95% confidence interval (CI). When P>0.01 and I2<50%, a fixed-effects model was used for the meta-analysis. When P<0.01 and I2>50%, a random-effects model was used for the meta-analysis.
Results
The retrieval results and the basic information of the included articles
A total of 307 articles were retrieved from the database search, leaving 289 articles after duplicity screening and automated quality screening. Based on a review of abstracts and titles, 147 of these articles were removed. After reading the full text, a further 136 articles were removed. Reasons for exclusion were mainly: 48 articles had subjects who were not adolescents, 56 studies did not have a randomised controlled analysis of cases, 18 studies had subjects whose age could not be distinguished, and relevant information could not be extracted for 14 studies. Finally, 6 articles (12-17) were included in the meta-analysis, which included 567 inclusion criteria for the subjects. Figure 1 shows the flowchart of the search used for the articles.
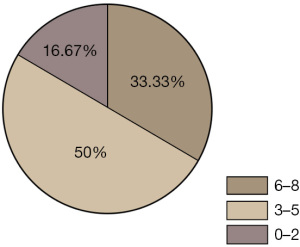
The quality of the selected articles was evaluated according to the quality evaluation table of recommendations of the National Institute of Clinical Excellence, UK, and the obtained data were plotted (see Figure 2). Among the included articles, 2 articles had scores of 6–8 (33.33%), 3 had scores of 3–5 (50%), and 1 had a score of 0–2 (16.67%).
Of the 567 participants in the 6 clinical studies that were included in the meta-analysis, 2 clinical studies were conducted with a small sample size of 25 and 58 patients, respectively, aged between 13 and 18 years. Of the 6 articles that were included, the sample size, disease type, age, treatment modality, duration of treatment, and effectiveness of GPT were described in detail in young adults with depression. The treatment methods included GPT, treatment as usual (Tau; routine care without any structured treatment), waiting-list control (WL; these patients did not receive any treatment, but were told that treatment would be available after a certain period), psychological placebo (PBO; these patients were given general counselling and attended follow-up examinations, but were not given any actual treatment), and the non-treatment (NT) control. Table 2 sets out the basic details of the included articles.
Table 2
| Author | Publication year | Disease type | Age (years) | Sample size | Inclusion criteria | Treatment methods | Treatment duration (months) | Effectiveness |
|---|---|---|---|---|---|---|---|---|
| Bar-Sela G | 2007 | Depression | 12–18 | 144 | BDI >14 | GPT =23 vs. WL =23 | 1 | GPT vs. WL, –0.73 (–1.47, –0.11) |
| Brandão FMV | 2019 | Depression | 13–19 | 53 | ADIS-IV-C/P | GPT =32 vs. NT =32 | 1.5 | GPT vs. WL, –0.34 (–0.98, –0.07) |
| Dolle K | 2013 | Depression | 12–18 | 60 | CES-D ≥20 | GPT =40 vs. PBO =40 | 1 | GPT vs. PBO, 0.56 (0.17, 1.23) |
| Dolle K | 2014 | Depression | 13–19 | 90 | CDI >10; HAM ≥10 | GPT =32 vs. NT =32 | 2 | GPT vs. NT, –0.96 (–1.89, –0.56) |
| Jorm AF | 2006 | Depression | 11–18 | 100 | CES-D ≥20 | GPT =51 vs. NT =51 | 1.5 | GPT vs. NT, –0.45 (–1.11, –0.25) |
| Tahmasebi Z | 2017 | Depression | 13–18 | 120 | CDI >10; HAM ≥10 | GPT =60 vs. WL =60 | 2 | GPT vs. WL, –0.86 (–1.34, 0.09) |
GPT, group painting therapy; WL, waiting-list; NT, non-treatment; PBO, placebo.
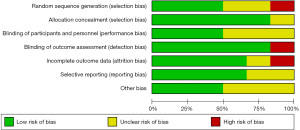
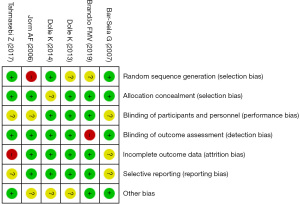
Results of the risk of bias evaluation of articles
Figure 3 and Figure 4 show the evaluation results of multiple bias-risk analyses of articles drawn by RevMan 5.3 software. In this study, among the 6 RCTs, only 4 (66.66%) (11,13-15) described the correct random allocation method, and 1 (16.67%) (12) described the hidden allocation scheme in detail. One (16.67%) (16) article evaluated the results using the blind method; however, the other articles were not evaluated using the blind method.
Meta-analysis of patients’ treatment effects
Figure 5 shows the effects of GPT on adolescent depression. In 6 studies, depression and anxiety symptoms were significantly improved in adolescents with depression after GPT for a period [mean deviation (MD) score =–8.23; 95% CI: –12.14 to –4.32; P<0.00001]. The results showed high heterogeneity in the efficacy outcomes of group drawing therapy for adolescent depression, with highly significant and statistically significant differences (I2=88%, P<0.01).

Meta-analysis results of PANAS score
Figure 6 and Figure 7 display the results of the meta-analysis forest plots for the positive and negative affective scale scores, respectively. A heterogeneity analysis was conducted on the PANAS scores of the adolescents. As Figure 6 shows, the chi-square test (Chi2) =7.09, degree of freedom (df) =4, I2=44%<50% (P>0.01). Thus, there was no substantial heterogeneity, and the fixed-effects model was used for the statistical analysis. It was found that the positive affective scale scores of patients in the GPT group were significantly higher than those of patients’ in the control group (MD =4.62; 95% CI: 3.79–5.45; P<0.01). As Figure 7 shows, Chi2 =14.77, df =4, I2=73%>50% (P<0.01). Thus, there was substantial heterogeneity, and the random-effects model was used for the statistical analysis. The results showed that the negative affective scale scores of patients in the GPT group were significantly lower than those of patients in the control group [MD =–1.88; 95% CI: –2.29 to –1.46; P<0.00001].
Meta-analysis results of CD-RISC scores
Figure 8 shows the forest plot of the meta-analysis of the CD-RISC scores. Based on the mean difference and standard deviation (SD) of CD-RISC scores in the 6 articles, the relevant data of 5 articles were extracted to analyze the heterogeneity of total sleep time of adolescent patients with depression. The results showed that Chi2 =30.81, df =3, I2=90%>50% (P<0.00001). Thus, there was substantial heterogeneity, and the random-effects model was used for the statistical analysis. We found that patients’ CD-RISC scores after GPT were significantly higher than those of patients in the control group [MD =13.66; 95% CI: 10.76–16.67; P<0.00001].
Meta-analysis of the SES scores
Figure 9 shows the meta-analysis forest plot of the SES scores. The mean difference and SD of the SES scores were described in detail in 6 articles, and the relevant data of 5 articles were extracted to conduct a heterogeneity analysis on the SES scores of the depressed adolescent patients. The results showed that Chi2 =67.28, df =4, I2=94%>50%, (P<0.00001). Thus, there was substantial heterogeneity, and the random-effects model was used for the statistical analysis. We found that the SES scores of depressed adolescent patients treated with GPT were significantly higher than those of patients in the control group [MD =8.85; 95% CI: 5.82–11.88; P<0.0001].
Meta-analysis results of WCST test results
Figures 10-13 show the meta-analysis results for the WCST test results. Figure 10 shows the meta-analysis forest plot for the MSCEIT-ME scores. The results of a heterogeneity analysis of the WCST test showed that Chi2 =33.40, df =4, I2=88%>50% (P<0.00001). Thus, there was substantial heterogeneity, and the random-effects model was used for the statistical analysis. We found that the MSCEIT-ME scores of depressed adolescent patients treated with GPT were significantly higher than those of patients in the control group [MD =4.17; 95% CI: 2.94–5.41; P<0.00001].
Figure 11 shows the meta-analysis results of SC scores. The results in Figure 11 show that Chi2 =16.46, df =3, I2=82%>50% (P<0.00001). Thus, there was substantial heterogeneity, and the random-effects model was used for the statistical analysis. We found that the SC scores of depressed adolescent patients treated with GPT were significantly higher than those of patients in the control group [MD =11.81; 95% CI: 9.27–14.35; P<0.00001].
Figure 12 shows the meta-analysis forest plot of BVMT-R score. The results show that Chi2 =35.86, df =4, I2=89%>50% (P<0.00001). Thus, there was substantial heterogeneity, and the random-effects model was used for the statistical analysis. We found that the BVMT-R scores of depressed adolescent patients treated with GPT were significantly lower than those of patients in the control group [MD =6.37; 95% CI: 4.72–8.03; P<0.00001].
Figure 13 shows the meta-analysis forest plot of Nab-Mazes scores. The results show that Chi2 =17.53, df =3, I2=83%>50% (P<0.00001). Thus, there was substantial heterogeneity, and the random-effects model was used for the statistical analysis. We found that that the NAB-Mazes scores of patients in the GPT group were significantly lower than those of patients in the control group [MD =7.60; 95% CI: 5.84–9.35; P<0.00001].
Meta-analysis results of MCCB test
Figure 14 and Figure 15 show the results of the meta-analysis of the MCCB test scores in GPT for adolescent patients with depression. Figure 14 shows the meta-analysis forest plot of the Re scores. The results showed that Chi2 =63.82 df =5, I2=92%>50% (P<0.00001). Thus, there was substantial heterogeneity, and the random-effects model was used for the statistical analysis. We found that that the Re scores of patients in the GPT group were significantly lower than those of patients in the control group [MD =12.43; 95% CI: 8.70–16.15; P<0.00001].
Figure 15 shows the meta-analysis forest map of the Rp scores. The results showed that Chi2 =15.37, df =5, I2=67%>50% (P<0.01). Thus, there was substantial heterogeneity, and the random-effects model was used for the statistical analysis. We found that the Rp scores of the depressed adolescent patients treated with GPT were significantly lower than those of patients in the control group [MD =–13.66; 95% CI: –14.81 to –12.51; P<0.01].
Publication bias
Figure 16 shows the funnel plot of the publication bias of the included articles. A meta-analysis was conducted on the negative emotion scores of the depressed adolescent patients before and after GPT. The circle and midline of some of the studies are basically symmetrical, which indicates that there was no bias in the publications; thus, the conclusions drawn are relatively credible.
Discussion
With the increasing pressure of modern people’s life, the number of patients with depression in the youth group is increasing year by year (18). As the target of attention from all walks of life, the treatment of depression has become a hot topic in scientific research. This study included 6 literatures, with a total of 567 cases of adolescent depression. This study adopted the recommendations of the National Institute of Clinical Optimization for quality evaluation. After strict scoring criteria, the results showed that among the adopted references, 2 had 6–8 scores (33.33%), 3 had 3 scores (50%), and 1 had 0–2 scores (16.66%).
The results of this study also showed that after GPT, the positive emotion scores of depressed adolescent patients improved significantly compared to those of patients in the control group [MD =4.62; 95% CI: 3.79–5.45; P<0.01]. GPT patients’ negative emotion scores also improved significantly [MD =–1.88; 95% CI: –2.29 to –1.46; P<0.01]. Patients’ CD-RISC scores after GPT were significantly higher than those of patients in the control group [MD =13.66; 95% CI: 10.76–16.67; P<0.01]. GPT patients’ SES scores were also significantly higher than those of patients in the control group [MD =8.85; 95% CI: 5.82–11.88; P<0.01]. Thus, GPT significantly improves the self-esteem and resilience levels of depressed adolescent patients. This may be related to the content of the painting courses, which have different themes, and the timely positive feedback and positive performance evaluations the patients receive from their peers in the courses, which increase their levels of satisfaction, and correct their negative self-views (19). The establishment of supportive, encouraging, and trusting relationships in GPT groups helps patients to master the correct way to vent negative emotions, improve their communication skills, identify their own problems, accept their own shortcomings, and approach problems in life with a positive and dialectical attitude, which in turn improves their resilience (20).
The meta-analysis of the WCST test results showed that patients’ MSCEIT-ME [MD =4.17; 95% CI: 2.94–5.41; P<0.01], SC [MD =11.81; 95% CI: 9.27–14.35; P<0.01], BVMT-R [MD =6.37; 95% CI: 4.72–8.03; P<0.01], and NAB-Mazes [MD =7.60; 95% CI: 5.84–9.35; P<0.01] scores all varied significantly, which indicates that GPT, as an anti-depressant method, restores the cognitive function of depressed adolescent patients to a certain extent. It may be that the entire painting process of GPT requires multiple areas of the brain to coordinate with each other and interact together, which accelerates the recovery of patients’ cognitive function to a certain extent. The meta-analysis results for the MCCB test scores showed that compared to patients in the control group, depressed adolescent patients who underwent GPT had significantly improved Re [MD =12.43; 95% CI: 8.70–16.15; P<0.01] and Rp [MD =–13.66; 95% CI: –14.81 to –12.51; P<0.01] scores, which suggests that GPT improves the executive function of depressed adolescent patients to a certain extent.
A meta-analysis was conducted to compare the efficacy of group painting therapy for adolescent depression before and after treatment. The funnel plot was drawn to show that there was no publication bias, and the obtained conclusion was credible. Risk bias was not the main factor affecting the conclusion.
Conclusions
In this study, 6 articles related to the negative emotional performance of adolescents with depression were identified using the Boolean logic retrieval method of compound logic retrieval. A meta-analysis was conducted to evaluate the effects of GPT on negative emotions in adolescent patients with depression. The results confirmed that GPT significantly improves the depressive symptoms of adolescent patients with depression, and also improves their positive emotion, CD-RISC, SES, WCST, and MCCB scores. A limitation of this study is that some of the included articles had certain levels of heterogeneity, which may have affected the results. Further studies need to be conducted in the future to confirm our results. In conclusion, this study provides a scientific basis for the use of GPT in the treatment of adolescent depression.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://dx.doi.org/10.21037/apm-21-2474
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/apm-21-2474). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Weersing VR, Jeffreys M, Do MT, et al. Evidence Base Update of Psychosocial Treatments for Child and Adolescent Depression. J Clin Child Adolesc Psychol 2017;46:11-43. [Crossref] [PubMed]
- Rice F, Riglin L, Lomax T, et al. Adolescent and adult differences in major depression symptom profiles. J Affect Disord 2019;243:175-81. [Crossref] [PubMed]
- Johnco C, Rapee RM. Depression literacy and stigma influence how parents perceive and respond to adolescent depressive symptoms. J Affect Disord 2018;241:599-607. [Crossref] [PubMed]
- Harder VS, Barry SE, French S, et al. Improving Adolescent Depression Screening in Pediatric Primary Care. Acad Pediatr 2019;19:925-33. [Crossref] [PubMed]
- Malhi GS, Mann JJ. Depression. Lancet 2018;392:2299-312. [Crossref] [PubMed]
- Mendelson T, Tandon SD. Prevention of Depression in Childhood and Adolescence. Child Adolesc Psychiatr Clin N Am 2016;25:201-18. [Crossref] [PubMed]
- Weersing VR, Shamseddeen W, Garber J, et al. Prevention of Depression in At-Risk Adolescents: Predictors and Moderators of Acute Effects. J Am Acad Child Adolesc Psychiatry 2016;55:219-26. [Crossref] [PubMed]
- Spiro-Levitt C, Gallop R, Young JF. Trajectories of change in maternal and adolescent depressive symptoms in the depression prevention initiative. J Affect Disord 2019;253:176-83. [Crossref] [PubMed]
- Blomdahl C, Guregård S, Rusner M, et al. A manual-based phenomenological art therapy for individuals diagnosed with moderate to severe depression (PATd): A randomized controlled study. Psychiatr Rehabil J 2018;41:169-82. [Crossref] [PubMed]
- Johnstone KM, Kemps E, Chen J. A Meta-Analysis of Universal School-Based Prevention Programs for Anxiety and Depression in Children. Clin Child Fam Psychol Rev 2018;21:466-81. [Crossref] [PubMed]
- Dietz LJ. Family-Based Interpersonal Psychotherapy: An Intervention for Preadolescent Depression. Am J Psychother 2020;73:22-8. [Crossref] [PubMed]
- Bar-Sela G, Atid L, Danos S, et al. Art therapy improved depression and influenced fatigue levels in cancer patients on chemotherapy. Psychooncology 2007;16:980-4. [Crossref] [PubMed]
- Brandão FMV, Silva CV, da Silva Gonçalves de Oliveira KR, et al. Art as a Therapeutic Tool in Depressive Disorders: a Systematic Review of the Literature. Psychiatr Q 2019;90:871-82. [Crossref] [PubMed]
- Dolle K, Schulte-Körne G. The treatment of depressive disorders in children and adolescents. Dtsch Arztebl Int 2013;110:854-60. [Crossref] [PubMed]
- Dolle K, Schulte-Körne G. Complementary treatment methods for depression in children and adolescents. Prax Kinderpsychol Kinderpsychiatr 2014;63:237-63. [Crossref] [PubMed]
- Jorm AF, Allen NB, O'Donnell CP, et al. Effectiveness of complementary and self-help treatments for depression in children and adolescents. Med J Aust 2006;185:368-72. [Crossref] [PubMed]
- Tahmasebi Z, Maghsoudi J, Talakoub S. The Effect of Painting on Depression in Children with Cancer Undergoing Chemotherapy. Iran J Nurs Midwifery Res 2017;22:102-5. [Crossref] [PubMed]
- Zhang K, Ma J, Chen J, et al. Effects of Drawing Therapy on Pediatric Oncology Patients: A Systematic Review. Cancer Nurs 2021; Epub ahead of print. [Crossref] [PubMed]
- Green EP, Cho H, Gallis J, et al. The impact of school support on depression among adolescent orphans: a cluster-randomized trial in Kenya. J Child Psychol Psychiatry 2019;60:54-62. [Crossref] [PubMed]
- Goh KK, Chang SC, Chen CH, et al. Therapeutic Strategies for Treatment-resistant Depression: State of the Art and Future Perspectives. Curr Pharm Des 2020;26:244-52. [Crossref] [PubMed]
(English Language Editor: L. Huleatt)














