
Measurement of the relative position of the femoral head center, greater trochanter, and lesser trochanter
Introduction
Hip fracture is a common fracture in the elderly, affecting around 6% of men and 18% of women (1). It is a serious trauma for the elderly, both physically and psychologically (2,3) For elderly patients with displacement, as an important way to treat the fracture (4,5) achieving appropriate limb length is a basic goal of hip arthroplasty (6-9). Due to the displacement of the fracture, the original lower limb length of the surgical side cannot be accurately referenced. To achieve this goal, we often refer to images of the healthy contralateral hip joint. However, if the contralateral hip has a deformity, trauma, or failed hip surgery, it also cannot be accurately referenced. If the reconstructed center of the femoral head can be judged by some anatomical landmarks of the hip, such as the tip of the greater trochanter and the lesser trochanter, it will aid in avoiding serious mistakes and achieving an appropriate lower limb length (10,11). Therefore, it is necessary to understand the basic data of normal hip anatomical markers and their relationship to the femoral head center. We have designed a relatively simple and convenient method to measure the anatomical markers, and analyzed the relationship between them. We present the following article in accordance with the MDAR reporting checklist (available at https://dx.doi.org/10.21037/apm-21-2538).
Methods
We retrieved the antero-posterior pelvic X-rays with both lower limbs at 10–15° internal rotation in the picture archiving communication system. The femoral head diameter (D), the linear distance (G) from the femoral head center (C) to the greater trochanter, and the linear distance (L) from the femoral head center to the lesser trochanter were measured (Figure 1). The basic information of the data was analyzed, and the ratios of G to D and L to D were calculated. The functional relationship between the data was analyzed after the factors of gender and age were included, and the 95% reference intervals of the basic data and ratio data were calculated.
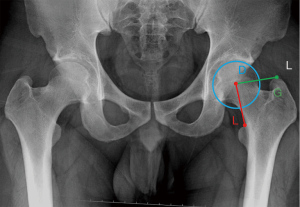
The diameter and femoral head center were determined by referring to the best fit circle method (12). However, different from the best fit circle method, the circle for measuring the femoral head diameter was drawn from the midline of the gap between the superior surface of the femoral head and the acetabulum as the cartilage cannot be shown by X-ray (Figure 1). The magnification of the imaging system was 110% and the measurement accuracy was 0.01 cm.
This study is a retrospective study, conducted in accordance with the Declaration of Helsinki (as revised in 2013), and approved by the Ethics Committee of Beijing Tongren Hospital (TRECKY2021-071). The patient personal privacy, identity information, and identifiable feature are not involved. With the approval of the ethics committee of our hospital, the informed consent of the patients was exempted.
Inclusion and exclusion criteria
The inclusion criteria for the X-ray films were: (I) the X-ray films were taken with both lower limbs straight and internal rotation 10–15°; (II) gender was not limited, and the bone was mature. The exclusion criteria were: (I) developmental dysplasia of the hip; (II) the accuracy of the measurement is affected by previous trauma or surgery, femoral head necrosis, osteoarthritis, degeneration, or other causes leading to hip joint deformation.
Statistical analysis
IBM SPSS statistics 23.0 software (IBM, Armonk, NY, USA) was used for statistical analysis. The Kolmogorov-Smirnov test was used to check the normality of age, diameter D, and the distance of G and L, and the results were expressed as mean and SD. Data between genders were compared using the two independent samples t-test. The relationships between the distance of G and L, age, gender (g), and diameter D were analyzed by linear regression, with gender: males =1, females =0. The 95% reference ranges of G, L, D, and the ratios G to D and L to D were calculated.
Results
A total of 97 patients with 194 hips (44 males, 88 hips; 53 females, 106 hips) were included in the study. The Kolmogorov-Smirnov test showed that age, diameter D, and the distances of G and L all fit the normal distribution. The mean age was 46.44±15.69 years (16–81 years), the diameter D was 5.08±0.43 cm (4.14–6.34 cm), the distance G was 4.68±0.45 cm (3.65–5.86 cm), and the distance L was 4.28±0.49 cm (3.21–5.56 cm).
Linear regression
Regression analysis of G, L, and D was conducted after gender (g) and age factors were included. Using the stepwise selection regression method, it was found that G was not affected by age, while L was not related to age and gender. The regression equations were as follows:
95% reference range
The 95% reference ranges of D, G, and L are shown in Table 1 for males and Table 2 for females. According to two independent samples t-test analysis, there was no statistical difference in the G/D or L/D ratio between genders, and the corresponding 95% reference intervals are shown in Table 3.
Table 1
| Distance | Lower end of the 95% range | Upper limit of the 95% range | Mean |
|---|---|---|---|
| D (cm) | 4.70 | 6.06 | 5.38 |
| G (cm) | 4.18 | 5.64 | 4.91 |
| L (cm) | 3.64 | 5.32 | 4.48 |
D, the femoral head diameter; G, the linear distance from the femoral head center to the greater trochanter; L, the linear distance from the femoral head center to the lesser trochanter.
Table 2
| Distance | Lower end of the 95% range | Upper limit of the 95% range | Mean |
|---|---|---|---|
| D (cm) | 4.21 | 5.45 | 4.83 |
| G (cm) | 3.68 | 5.29 | 4.48 |
| L (cm) | 3.19 | 5.04 | 4.12 |
D, the femoral head diameter; G, the linear distance from the femoral head center to the greater trochanter; L, the linear distance from the femoral head center to the lesser trochanter.
Table 3
| Ratio | Lower end of the 95% range | Upper limit of the 95% range | Mean |
|---|---|---|---|
| G/D | 0.78 | 1.06 | 0.92 |
| L/D | 0.68 | 1.00 | 0.84 |
D, the femoral head diameter; G, the linear distance from the femoral head center to the greater trochanter; L, the linear distance from the femoral head center to the lesser trochanter.
Discussion
In our previous study (13), we measured the contralateral side femoral head diameter (non-fracture side) and the distance from the femoral head center to the lesser trochanter in antero-posterior pelvic X-ray film before hip hemiarthroplasty for a patient with femoral neck fracture, and calculated the ratio of this distance to the diameter. During surgery, after measuring the femoral head diameter (fracture side) with a vernier caliper. According to the contralateral ratio, the distance that should be obtained from the femoral head prosthesis center to the lesser trochanter was calculated. Subsequently, the distance was checked after implanting the femoral component. Using this method, we obtained a satisfactory leg length discrepancy (LLD), with a mean value of 4.4±3.2 mm. This confirms that measuring the relationship between hip anatomical markers is helpful to avoid LLD. However, we have encountered some specific cases of femoral neck fracture in which the contralateral hips have a deformity, trauma, or failed hip surgery, and failed to be referenced. This problem prompted us to carry out this study.
In this situation, the shuck test and drop-kick test may be used to achieve satisfactory length of the lower limb, but the shortcomings are also obvious. In principle, these 2 tests are used to check the tension of the soft tissue around the hip joint, which is an indirect inference of whether the length of the lower limb is accurate, and therefore their accuracy is limited (14). In addition, the reliability of the tests will be affected by the type of anesthesia (15).
Some reports have performed similar measurements to our study, measuring the distance between the femoral head center and the lesser trochanter (16-18), and comparing this distance with the femoral head diameter (16,17). Unnanuntana et al.’s measurement is more similar to ours, as they have reported both the data of the distances from the femoral head center to the greater trochanter and to the lesser trochanter (16). However, the distance from the femoral head center to the greater trochanter they measured was parallel to the proximal femoral shaft, and this parallel direction is very difficult to determine in surgery due to the limited exposure range of the proximal femur. Our method of measuring linear distance is more convenient and maybe more valuable for clinical application in surgery.
We analyzed the relationship between the anatomical landmarks of the hip. The regression equations of linear distances G and L were obtained after gender and age factors were included, and the 95% reference intervals of the basic data and ratio data were calculated. These data may provide a reference for restoring appropriate lower limb length during hip arthroplasty for hip fracture, especially in the absence of a contralateral hip reference. More importantly, if data obtained during the operation exceed the 95% reference range, we may be doing something wrong. For thin or obese patients, a study has shown that X-ray magnification will be reduced by 15% or increased by 25%. (19). With this in mind, the ratio data are more convenient for application (13).
There are some limitations in our study. X-ray cannot accurately show the thickness of cartilage. Different from the best fit circle method (12), and same as our previous research (13), the circle measuring the femoral head diameter was drawn through the midline of the gap between the superior surface of the femoral head and the acetabulum. Previous study showed that the femoral head cartilage thickness was 1.76±0.30 mm and the acetabular cartilage thickness was 1.59±0.31 mm in this area, with an average difference of 0.17 mm between them (20). Referring to Ranawat et al. and Woolson and Harris’s criteria of 6 mm for determining the difference of lower limb length (21,22), the difference value of 0.17 mm is much smaller than that of 6 mm, which may have no significant effect on the lower limb length.
This is an imaging study, and the data obtained have not been applied in surgery. However, our data may provide us with insights and some data references for special hip arthroplasty cases without a contralateral reference, and it is also the basis of our future clinical research.
Conclusions
We determined the relationship between anatomical landmarks of the hip. The measurement was designed to be convenient for clinical application, and we hope to provide some reference for avoiding obvious mistakes and restoring appropriate lower limb length in hip arthroplasty.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the MDAR reporting checklist. Available at https://dx.doi.org/10.21037/apm-21-2538
Data Sharing Statement: Available at https://dx.doi.org/10.21037/apm-21-2538
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/apm-21-2538). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was a retrospective study, conducted in accordance with the Declaration of Helsinki (as revised in 2013), and approved by the Ethics Committee of the Beijing Tongren Hospital (TRECKY2021-071). It does not involve patient personal privacy, identity information, and identifiable features. With the approval of the ethics committee of our hospital, the informed consent of the patients was exempted.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Veronese N, Maggi S. Epidemiology and social costs of hip fracture. Injury 2018;49:1458-60. [Crossref] [PubMed]
- Alexiou KI, Roushias A, Varitimidis SE, et al. Quality of life and psychological consequences in elderly patients after a hip fracture: a review. Clin Interv Aging 2018;13:143-50. [Crossref] [PubMed]
- Peeters CM, Visser E, Van de Ree CL, et al. Quality of life after hip fracture in the elderly: A systematic literature review. Injury 2016;47:1369-82. [Crossref] [PubMed]
- Bhandari M, Swiontkowski M. Management of Acute Hip Fracture. N Engl J Med 2017;377:2053-62. [Crossref] [PubMed]
- Gjertsen JE. Should Total Hip Arthroplasty Be Used for Hip Fracture? N Engl J Med 2019;381:2261-2. [Crossref] [PubMed]
- Debbi EM, Rajaee SS, Mayeda BF, et al. Determining and Achieving Target Limb Length and Offset in Total Hip Arthroplasty Using Intraoperative Digital Radiography. J Arthroplasty 2020;35:779-85. [Crossref] [PubMed]
- Sculco PK, Cottino U, Abdel MP, et al. Avoiding Hip Instability and Limb Length Discrepancy After Total Hip Arthroplasty. Orthop Clin North Am 2016;47:327-34. [Crossref] [PubMed]
- Zhao JX, Su XY, Zhao Z, et al. Radiographic assessment of the cup orientation after total hip arthroplasty: a literature review. Ann Transl Med 2020;8:130. [Crossref] [PubMed]
- Clark CR, Huddleston HD, Schoch EP 3rd, et al. Leg-length discrepancy after total hip arthroplasty. J Am Acad Orthop Surg 2006;14:38-45. [Crossref] [PubMed]
- Polishchuk DL, Patrick DA Jr, Gvozdyev BV, et al. Predicting femoral head diameter and lesser trochanter to center of femoral head distance: a novel method of templating hip hemiarthroplasty. J Arthroplasty 2013;28:1603-7. [Crossref] [PubMed]
- Kim JI, Moon NH, Shin WC, et al. Reliable anatomical landmarks for minimizing leg-length discrepancy during hip arthroplasty using the lateral transgluteal approach for femoral neck fracture. Injury 2017;48:2548-54. [Crossref] [PubMed]
- Young EY, Gebhart JJ, Bajwa N, et al. Femoral head asymmetry and coxa magna: anatomic study. J Pediatr Orthop 2014;34:415-20. [Crossref] [PubMed]
- Wang G, Guo A, Yu F, et al. A simple method to minimize leg length discrepancy in hip hemiarthroplasty. Clin Interv Aging 2019;14:1601-5. [Crossref] [PubMed]
- Naito M, Ogata K, Asayama I. Intraoperative limb length measurement in total hip arthroplasty. Int Orthop 1999;23:31-3. [Crossref] [PubMed]
- Sathappan SS, Ginat D, Patel V, et al. Effect of anesthesia type on limb length discrepancy after total hip arthroplasty. J Arthroplasty 2008;23:203-9. [Crossref] [PubMed]
- Unnanuntana A, Toogood P, Hart D, et al. The evaluation of two references for restoring proximal femoral anatomy during total hip arthroplasty. Clin Anat 2010;23:312-8. [Crossref] [PubMed]
- Boymans TAEJ, Veldman HD, Grimm BP, et al. Femoral Head Size is Correlated With Head Position in Very Elderly Patients. J Arthroplasty 2017;32:587-93. [Crossref] [PubMed]
- Matsuda K, Nakamura S, Matsushita T. A simple method to minimize limb-length discrepancy after hip arthroplasty. Acta Orthop 2006;77:375-9. [Crossref] [PubMed]
- Della Valle AG, Padgett DE, Salvati EA. Preoperative planning for primary total hip arthroplasty. J Am Acad Orthop Surg 2005;13:455-62. [Crossref] [PubMed]
- Shepherd DE, Seedhom BB. Thickness of human articular cartilage in joints of the lower limb. Ann Rheum Dis 1999;58:27-34. [Crossref] [PubMed]
- Ranawat CS, Rao RR, Rodriguez JA, et al. Correction of limb-length inequality during total hip arthroplasty. J Arthroplasty 2001;16:715-20. [Crossref] [PubMed]
- Woolson ST, Harris WH. A method of intraoperative limb length measurement in total hip arthroplasty. Clin Orthop Relat Res 1985;207-10. [Crossref] [PubMed]


