
Pressure ulcers in patients with diabetes: a bibliometrics analysis
Introduction
Pressure ulcer (PU) refers to ulceration and necrosis of the local tissues of the body, especially the tissues of bone protuberances. In PU, the blood supply to the tissues is blocked due to long-term pressure and friction, resulting in skin and subcutaneous tissue ischemia and hypoxia (1). PU brings suffering to patients, reduces the quality of life of patients, prolongs the length of hospital stay, and increases medical expenses (2,3). PUs often occur in patients who are bedridden for a long time (4,5). As the proportion of older adults in the population continues to grow, the number of older adult patients with various chronic diseases, especially diabetes (4) and PUs has increased significantly. Diabetic wounds are not easily healed, and once a pressure sore occurs, management becomes extremely challenging (6). PUs in diabetic patients are mainly foot ulcers and arise because of peripheral neuropathy, which leads to long-term insensitivity to compression, necrosis, and the nonhealing of the compressed areas (7). Moreover, even if the necrotic site is amputated, the patient’s risk of recurrent PU remains high (8,9). Previous studies suggested that the main causes leading to the high risk of recurrent PU in patients with diabetes included advanced age, long-time pressure, malnutrition, uncontrolled blood sugar (10).
Regarding the problem of PU in patients with diabetes, research includes 4 major areas: mechanism, prevention, treatment, and prognosis (11). Bibliometrics is the analysis of the literature on a specific subject that can capture the current state of the research in a field. Bibliometrics is conducive to evaluating related research on a topic and provides researchers with a rough outline of the focus and existing problems in a field (12). Different from systematic review and meta-analysis which focused on some specific question (13), the purpose of this study was to analyze the current research state of PU research in patients with diabetes through a bibliometric approach.
Methods
Data source
At present, the main data source of bibliometrics is the Science Citation Index Expanded (SCI-E) database in the Web of Science Core Collection (WOSCC), which was founded and by the American Institute of Scientific Information in 1957. The database contains papers from more than 8,000 important journals and their cited information. SCIE is not only an\valuable citation retrieval tool but is also an important platform for bibliometric and scientific research evaluation. Our study used SCIE as the target database for retrieval and analysis.
Search strategy
For topic retrieval, the topic terms were “Pressure Ulcer” and “Diabetes”. The publication time of the target document was from the publication time of the earliest document that could be retrieved [1965] to the last retrieval date of this study (June 28, 2021).
Analysis
We exported all the records of the search results and the cited references into text format to create the original data file, and then used Citespace software to analyze the data file. The content of the analysis included the annual distribution of the number of target documents; the countries, institutions, and journals that published these articles; authors; keywords used in the articles; and changes in keywords frequency over time.
Statistical analysis
As the aim of this study was to capture and describe the current state of research in diabetic PU, no comparison between groups or correlation analysis was performed. The data are mainly expressed as numbers and percentages.
Results
Search results
The preliminary search results yielded a total of 1,356 research literature records, including 1,069 original articles, 185 reviews, 77 conference proceedings, 9 editorial materials, 5 early access papers, 5 meeting abstracts, 3 book chapters, 2 letters, and 1 note. After 85 duplicates were eliminated, 1,271 documents were entered into the final analysis (Table 1). In terms of annual change, the number of publications continued to increase for the most part (Table 2, Figure 1). The citation frequency of these documents totaled 47,081 citations, the h-index was 101, and the average number of citations per document was 37.04 (Figure 2). The number of citations showed a significant increase year by year.
Table 1
| Literature type | Number | % (N=1,271) |
|---|---|---|
| Articles | 1,069 | 84.11 |
| Review articles | 185 | 14.56 |
| Conference proceedings | 77 | 6.06 |
| Editorial materials | 9 | 0.71 |
| Early access | 5 | 0.39 |
| Meeting abstracts | 5 | 0.39 |
| Book chapters | 3 | 0.24 |
| Letters | 2 | 0.16 |
| Notes | 1 | 0.08 |
Table 2
| Publication year | Number | % (N=1,271) |
|---|---|---|
| 2021 | 20 | 1.57 |
| 2020 | 110 | 8.65 |
| 2019 | 92 | 7.24 |
| 2018 | 85 | 6.69 |
| 2017 | 67 | 5.27 |
| 2016 | 91 | 7.16 |
| 2015 | 72 | 5.66 |
| 2014 | 63 | 4.96 |
| 2013 | 65 | 5.11 |
| 2012 | 64 | 5.04 |
| 2011 | 41 | 3.23 |
| 2010 | 45 | 3.54 |
| 2009 | 52 | 4.09 |
| 2008 | 58 | 4.56 |
| 2007 | 34 | 2.68 |
| 2006 | 21 | 1.65 |
| 2005 | 30 | 2.36 |
| 2004 | 28 | 2.20 |
| 2003 | 27 | 2.12 |
| 2002 | 30 | 2.36 |
| 2001 | 20 | 1.57 |
| 2000 | 17 | 1.34 |
| 1999 | 31 | 2.44 |
| 1998 | 25 | 1.97 |
| 1997 | 17 | 1.34 |
| 1996 | 16 | 1.26 |
| 1995 | 8 | 0.63 |
| 1994 | 10 | 0.79 |
| 1993 | 13 | 1.02 |
| 1992 | 12 | 0.94 |
| 1991 | 7 | 0.55 |
Countries and institutions
In order to understand the distribution of countries from which the literature originated, we used CiteSpace software to analyze the text of search results and generate a map of countries (Figure 3) In all, 63 countries were recorded as the source of the published literature, and there were 314 instances of cooperation between countries. A similar map for institutions was also generated (Figure 4). In all, 161 institutions were identified, with 338 collaborations between institutions. The statistical results show that the top 5 countries in the number of publications consisted of the United States, the United Kingdom, China, Australia, and the Netherlands; the top 5 countries in centrality included the Netherlands, the United States, Canada, Japan, and France (Tables 3,4). The top institutions in terms of the number of published studies were the University of Amsterdam, Cardiff University, The University of Washington, and the University of Manchester. The institutions with the highest centrality included the University of Amsterdam, the University of Groningen, the University of Washington, the University of Adelaide, Baylor College of Medicine, and Queensland University of Technology (Tables 5,6).

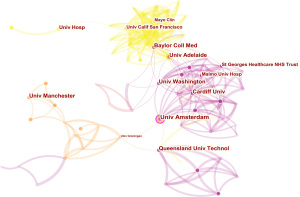
Table 3
| Rank | Country | Publications |
|---|---|---|
| 1 | The United State of America | 109 |
| 2 | England | 42 |
| 3 | China | 36 |
| 4 | Australia | 29 |
| 5 | The Netherlands | 26 |
| 6 | Italy | 17 |
| 7 | Japan | 14 |
| 8 | France | 13 |
| 9 | Germany | 12 |
| 10 | Scotland | 12 |
Table 4
| Rank | Countries | Centrality |
|---|---|---|
| 1 | The Netherlands | 0.18 |
| 2 | The United State of America | 0.16 |
| 3 | Canada | 0.12 |
| 4 | Japan | 0.11 |
| 5 | France | 0.10 |
| 6 | Switzerland | 0.06 |
| 7 | Belgium | 0.05 |
| 8 | Colombia | 0.05 |
| 9 | Egypt | 0.05 |
| 10 | Romania | 0.05 |
Table 5
| Rank | Institutions | Publications |
|---|---|---|
| 1 | University of Amsterdam | 9 |
| 2 | Cardiff University | 8 |
| 3 | University of Washington | 8 |
| 4 | University of Manchester | 8 |
| 5 | University of Adelaide | 7 |
| 6 | Baylor College of Medicine | 7 |
| 7 | Queensland University of Technology | 7 |
| 8 | Washington University Hospital | 6 |
| 9 | University of Sao Paulo | 5 |
| 10 | St Georges Healthcare NHS Trust | 5 |
Table 6
| Rank | Institution | Centrality |
|---|---|---|
| 1 | University of Amsterdam | 0.17 |
| 2 | University of Groningen | 0.13 |
| 3 | University of Washington | 0.08 |
| 4 | University of Adelaide | 0.08 |
| 5 | Baylor College of Medicine | 0.08 |
| 6 | Queensland University of Technology | 0.08 |
| 7 | University of Arizona | 0.06 |
| 8 | Cardiff University | 0.05 |
| 9 | Harvard Medical School | 0.05 |
| 10 | Malmo University Hospital | 0.03 |
Author analysis
The authors with a high number of publications included Bus SA, Apelqvist J, the International Working Group on the Diabetic Foot (IWGDF), and Hinchliffe RJ (Table 7). Only 2 authors had a centrality score above 0.01, and the IWGDF is a research group, which suggests that there is relatively little cooperation between authors (Table 8, Figure 5). The most prolific authors also had a high frequency of citations. The top 5 most prolific authors were Armstrong DG, Boulton AJM, Bus SA, Lavery LA, and Singh N (Table 9); the top 5 most-cited authors were Reiber GE, Birke JA, Van Netten JJ, Wu SC, and Brownrigg JRW (Figure 6, Table 10).
Table 7
| Rank | Authors | Published works |
|---|---|---|
| 1 | Bus SA | 10 |
| 2 | Apelqvist J | 6 |
| 3 | IWGDF | 6 |
| 4 | Hinchliffe RJ | 5 |
| 5 | Price PE | 4 |
| 6 | Schaper NC | 4 |
| 7 | Fitridge R | 3 |
| 8 | Chuter VH | 3 |
| 9 | Malecki MT | 3 |
IWGDF, The International Working Group for the Diabetic Foot.
Table 8
| Rank | Authors | Centrality |
|---|---|---|
| 1 | IWGDF | 0.03 |
| 2 | Price PE | 0.01 |
IWGDF, The International Working Group for the Diabetic Foot.
Table 9
| Rank | Authors | Number of citations |
|---|---|---|
| 1 | Armstrong DG | 95 |
| 2 | Boulton AJM | 79 |
| 3 | Bus SA | 72 |
| 4 | Lavery LA | 67 |
| 5 | Singh N | 50 |
| 6 | PROMPERS L | 42 |
| 7 | Cavanagh PR | 39 |
| 8 | Frykberg RG | 37 |
| 9 | Lipsky BA | 37 |
| 10 | Veves A | 35 |
Table 10
| Rank | Authors | Centrality |
|---|---|---|
| 1 | Reiber GE | 0.11 |
| 2 | Birke JA | 0.11 |
| 3 | Van Netten JJ | 0.10 |
| 4 | Wu SC | 0.10 |
| 5 | Brownrigg JRW | 0.10 |
| 6 | Cavanagh PR | 0.09 |
| 7 | Sawacha Z | 0.09 |
| 8 | Alavi A | 0.09 |
| 9 | Frykberg RG | 0.08 |
| 10 | Driver VR | 0.08 |
Distribution of journals
The 1,271 articles in this study were from 469 journals. Among them, 11 journals published more than 20 articles (Table 11). These journals published 346 articles, accounting for 27.22% of the total literature (Table 11). Based on these results, it is speculated that journals such as Diabetes Metabolism Research and Reviews, Diabetes Care, and Journal of Wound Care have considerable influence in this field compared with others. The top 5 journals by number of citations were Diabetes Care, Diabetes-metabolism research and reviews, Diabetic Medicine, International Wound Journal, and Diabetologia (Table 12). The top 5 journals for centrality were Cochrane Database Systematic Review, Arch Surg-Chicago, Med Clin N Am, BMJ Open, and Circ Res (Table 13).
Table 11
| Publication titles | Number | % (N=1,271) |
|---|---|---|
| Diabetes Metabolism Research and Reviews | 54 | 4.25 |
| Diabetes Care | 46 | 3.62 |
| Journal of Wound Care | 38 | 2.99 |
| Diabetic Medicine | 37 | 2.91 |
| International Wound Journal | 29 | 2.28 |
| Wounds a Compendium of Clinical Research and Practice | 29 | 2.28 |
| Foot Ankle International | 25 | 1.97 |
| Journal of The American Podiatric Medical Association | 24 | 1.89 |
| Ostomy Wound Management | 24 | 1.89 |
| Diabetes Research and Clinical Practice | 20 | 1.57 |
| International Journal of Lower Extremity Wounds | 20 | 1.57 |
Table 12
| Rank | Journal | Number of citations |
|---|---|---|
| 1 | Diabetes Care | 228 |
| 2 | Diabetes Metabolism Research and Reviews | 148 |
| 3 | Diabetic Medicine | 145 |
| 4 | International Wound Journal | 118 |
| 5 | Diabetologia | 115 |
| 6 | Lancet | 113 |
| 7 | Wound Repair Regeneration | 103 |
| 8 | JAMA-Journal of American Medicine Association | 98 |
| 9 | New England Journal of Medicine | 95 |
| 10 | J Vascular Surgery | 94 |
Table 13
| Rank | Journals | Centrality |
|---|---|---|
| 1 | Cochrane DataBase of Systematic Review | 0.10 |
| 2 | Archive of Surgery-Chicago | 0.09 |
| 3 | Medical Clinics of North America | 0.08 |
| 4 | BMJ Open | 0.07 |
| 5 | Circulation Research | 0.07 |
| 6 | Journal of Tissue Viability | 0.06 |
| 7 | Science | 0.06 |
| 8 | American Heart Journal | 0.06 |
| 9 | Critical Care Medicine | 0.06 |
| 10 | Advances in Wound Care | 0.05 |
Keyword analysis
We use CiteSpace software to analyze the use of keywords and generate a keyword co-occurrence map (N=248, E=1,238). A total of 248 keywords were used in these documents and had 1,238 links between them. The top 5 most frequently used keywords were “diabetic foot ulcer”, “diabetes”, “risk”, “ulcer”, and “management” (Table 14). The top 4 keywords for centrality were “association”, “guideline”, “peripheral arterial disease”, and “ankle” (Table 15, Figure 7). Keyword analysis indicated that the use of keywords in this field is not uniform. According to the use of keywords, we speculate that the research on the subject of PUs in patients with diabetes is centralized around the risk and management of foot ulcers.
Table 14
| Rank | Keywords | Number of utility |
|---|---|---|
| 1 | Diabetic foot ulcer | 121 |
| 2 | Diabetes | 90 |
| 3 | Risk | 76 |
| 4 | Ulcer | 68 |
| 5 | Management | 59 |
| 6 | Pressure ulcer | 46 |
| 7 | Prevention | 44 |
| 8 | Pressure | 36 |
| 9 | Amputation | 35 |
| 10 | Plantar pressure | 34 |
Table 15
| Rank | Keywords | Centrality |
|---|---|---|
| 1 | Association | 0.17 |
| 2 | Guideline | 0.11 |
| 3 | Peripheral arterial disease | 0.08 |
| 4 | Ankle | 0.08 |
| 5 | IWGDF guidance | 0.07 |
| 6 | Quality of life | 0.07 |
| 7 | Diabetes | 0.06 |
| 8 | Ulcer | 0.06 |
| 9 | Prevention | 0.06 |
| 10 | Infection | 0.06 |
IWGDF, The International Working Group for the Diabetic Foot.
Discussion
In this study, 1,271 articles about PUs in diabetic patients were retrieved by topic term search. Relative to the large number of patients with diabetes and PUs, there were few studies in this field. Of the published works, we found that the United States, the United Kingdom, China and other countries had published more documents, while the Netherlands, the United States, Canada, and other countries engaged in more international cooperation. Among the institutions, the University of Amsterdam not only published the most documents but also collaborated the most. The number of articles published by each author was not high, and there was little collaboration between authors. In terms of journals, the literature was mainly published in professional journals of diabetes or wound management. Keywords were used frequently, and our analysis showed that the current research focuses lies on the management of the risk of PUs in patients with diabetes.
We found that although the United States, the United Kingdom, China, and other countries had published more documents, the country with the highest centrality was the Netherlands. Furthermore, the institution with the highest number of publications and centrality was the University of Amsterdam in the Netherlands, which may be attributed to the population size, high social welfare, and the status of the University of Amsterdam in the Netherlands. However, the analysis of the authors found that there was less collaboration between the authors. This result suggested that in most literature, the number of authors was small and collaboration between different institution was also few. Additionally, we found there to be no pattern in the use of keywords. There are a total of 248 keywords used in the literature under this topic, many of which are repeated words. Based on the above results, we believe that there is still a lot of work to be done in the study of PUs in patients with diabetes. First, with the intensification of an aging society, the number of older adult patients and disabled older adults has gradually increased, resulting in a significant increase in the number of these patients who are bedridden or have limited mobility for extended periods. These patients often have diabetes and poor blood sugar control. They have a high risk of PUs, but this pressure is not restricted to the feet, and may occur especially in the sacrococcygeal area, hips, and joint protrusions. Related research should not be limited to the prevention and treatment of diabetic foot but should increase attention to PUs in other parts of the body. Second, according to our clinical practice and related literature reports, we know that once PUs occur in diabetic patients, especially older ones, it is very difficult to cure (14). Therefore, research should concentrate particularly on prevention. According to the current concepts in chronic disease management, prevention work should be integrated into the management of chronic diseases of diabetes, and the role of the chronic disease management team should, as much as possible, focus on control of blood sugar, reducing the time of partial pressure on the patient’s body, and improving the nutritional status of long-term bedridden patients.
Given the aging demographics of current society, PUs will become a greater problem throughout the world. Epidemiology shows that approximately 1–3 million patients acquire PU in the United States each year (15). The rate of PUs higher in hospitalized patients with acute and critical illness (16,17); for instance, one study showed that of 42,000 patients, 14.8% had PUs (18). Therefore, for older adult patients, especially those with diabetes or critical illness, special attention should be paid to the prevention and treatment of PUs.
There have been no breakthroughs in the treatment of PUs. Although PUs are small, the mechanisms involved are complicated. Moreover, if the pressure on the diseased area cannot be continuously relieved, it will be difficult for any treatment to exert a real effect (19). The mechanism of PUs involves the following: first, for a variety of reasons, the local soft tissues of the bone protrusion may be continuously compressed for a long time, which directly leads blockage in local blood supply, requiring the pressure to be effectively relieved. Second, shear and friction can damage the subcutaneous vascular bed and cause ischemia (20). In addition, the moist skin in the local environment remains in maceration for an extended period, which makes the skin more susceptible to shear and friction damage, and creates an environment conducive to the breeding of pathogens and local infection (21). Current treatment of PUs mainly includes medicinal dressings and external disinfectants containing silver and iodine (22). Relevant drug treatment studies are marred by inconsistent drug formulation specifications, lack of evaluations with an endpoint of complete PU healing, and a lack of large-scale, multicenter, randomized controlled studies. Moreover, few analyses on systemic adverse drug reactions exist (23). We believe that the medical treatment of PUs should focus on promoting local tissue healing, increasing local drug concentration, prolonging drug release time, and reducing systemic adverse drug reactions. The medication method should focus on topical administration, and a drug-carrying matrix with good performance to reduce the impact of sweat and secretions on drug adhesion should be developed (24).
In the prevention of PUs in patients with diabetes, the most important issue is controlling blood sugar. It should be noted that, according to the current diabetes prevention and control guidelines, the goals of blood sugar control for older adults and susceptible patients should be appropriately relaxed (25). Excessively strict dietary control that leads to malnutrition of patients should be avoided, as this makes patients prone to PUs and is not conducive to their being healed (26). Additionally, diabetic patients who have been bedridden for an extended period should pay full attention to reducing the long-term pressure on the body. During the nursing process, attention should be paid to observing the local skin and reducing the influence of shear and friction in the operation (22,27). In conclusion, our present study revealed an overview of the status of PU research in diabetic patient. Taking our findings into consideration, investigators should put more attention to this field to promote the care for these diabetic patients with PU. Maybe in the future, the treatment and prevention methods for these patients will be made great progress.
Some limitations of this study should be noted. First, as this study used topic term retrieval, we might have missed documents that could be retrieved by other retrieval strategies, resulting in a nonrepresentative analysis of the state of research. This can also be confirmed by the use of keywords, because we found that the use of keywords was rather confusing and led us to omit some when conducting our search. Second, there might have been a few documents derived from the same research, leading to the possibility of duplicates being present in the analysis.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/apm-21-2757). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hajhosseini B, Longaker MT, Gurtner GC. Pressure Injury. Ann Surg 2020;271:671-9. [Crossref] [PubMed]
- Sen CK. Human Wound and Its Burden: Updated 2020 Compendium of Estimates. Adv Wound Care (New Rochelle) 2021;10:281-92. [Crossref] [PubMed]
- López-Franco MD, Parra-Anguita L, Comino-Sanz IM, et al. Attitudes of Spanish Nurses towards Pressure Injury Prevention and Psychometric Characteristics of the Spanish Version of the APuP Instrument. Int J Environ Res Public Health 2020;17:8543. [Crossref] [PubMed]
- Børsting TE, Tvedt CR, Skogestad IJ, et al. Prevalence of pressure ulcer and associated risk factors in middle- and older-aged medical inpatients in Norway. J Clin Nurs 2018;27:e535-43. [Crossref] [PubMed]
- Fritz A, Gericke L, Höch A, et al. Time-to-treatment is a risk factor for the development of pressure ulcers in elderly patients with fractures of the pelvis and acetabulum. Injury 2020;51:352-6. [Crossref] [PubMed]
- Rayman G, Vas P, Dhatariya K, et al. Guidelines on use of interventions to enhance healing of chronic foot ulcers in diabetes (IWGDF 2019 update). Diabetes Metab Res Rev 2020;36:e3283 [Crossref] [PubMed]
- van Netten JJ, Raspovic A, Lavery LA, et al. Prevention of foot ulcers in the at-risk patient with diabetes: a systematic review. Diabetes Metab Res Rev 2020;36:e3270 [Crossref] [PubMed]
- Blume P, Wu S. Updating the Diabetic Foot Treatment Algorithm: Recommendations on Treatment Using Advanced Medicine and Therapies. Wounds 2018;30:29-35. [PubMed]
- Brownrigg JR, Hinchliffe RJ, Apelqvist J, et al. Performance of prognostic markers in the prediction of wound healing or amputation among patients with foot ulcers in diabetes: a systematic review. Diabetes Metab Res Rev 2016;32:128-35. [Crossref] [PubMed]
- Wei R, Chen HL, Zha ML, et al. Diabetes and pressure ulcer risk in hip fracture patients: a meta-analysis. J Wound Care 2017;26:519-527. [Crossref] [PubMed]
- Primadhi RA, Herman H. Diabetic foot: Which one comes first, the ulcer or the contracture? World J Orthop 2021;12:61-8. [Crossref] [PubMed]
- Roldan-Valadez E, Salazar-Ruiz SY, Ibarra-Contreras R, et al. Current concepts on bibliometrics: a brief review about impact factor, Eigenfactor score, CiteScore, SCImago Journal Rank, Source-Normalised Impact per Paper, H-index, and alternative metrics. Ir J Med Sci 2019;188:939-51. [Crossref] [PubMed]
- Liu P, He W, Chen HL. Diabetes mellitus as a risk factor for surgery-related pressure ulcers: a meta-analysis. J Wound Ostomy Continence Nurs 2012;39:495-9. [Crossref] [PubMed]
- Jaul E. Assessment and management of pressure ulcers in the elderly: current strategies. Drugs Aging 2010;27:311-25. [Crossref] [PubMed]
- Attali E, Yogev Y. The impact of advanced maternal age on pregnancy outcome. Best Pract Res Clin Obstet Gynaecol 2021;70:2-9. [Crossref] [PubMed]
- Robnett MK. The incidence of skin breakdown in a surgical intensive care unit. J Nurs Qual Assur 1986;1:77-81. [Crossref] [PubMed]
- Pachá HHP, Faria JIL, Oliveira KA, et al. Pressure Ulcer in Intensive Care Units: a case-control study. Rev Bras Enferm 2018;71:3027-34. [Crossref] [PubMed]
- Amlung SR, Miller WL, Bosley LM. The 1999 National Pressure Ulcer Prevalence Survey: a benchmarking approach. Adv Skin Wound Care 2001;14:297-301. [Crossref] [PubMed]
- Teo CSM, Claire CA, Lopez V, et al. Pressure injury prevention and management practices among nurses: A realist case study. Int Wound J 2019;16:153-63. [Crossref] [PubMed]
- Bhattacharya S, Mishra RK. Pressure ulcers: Current understanding and newer modalities of treatment. Indian J Plast Surg 2015;48:4-16. [Crossref] [PubMed]
- Edsberg LE. Pressure ulcer tissue histology: an appraisal of current knowledge. Ostomy Wound Manage 2007;53:40-9. [PubMed]
- Mervis JS, Phillips TJ. Pressure ulcers: Prevention and management. J Am Acad Dermatol 2019;81:893-902. [Crossref] [PubMed]
- Chou R, Dana T, Bougatsos C, et al. Pressure ulcer risk assessment and prevention: a systematic comparative effectiveness review. Ann Intern Med 2013;159:28-38. [Crossref] [PubMed]
- Gould L, Stuntz M, Giovannelli M, et al. Wound Healing Society 2015 update on guidelines for pressure ulcers. Wound Repair Regen 2016;24:145-62. [Crossref] [PubMed]
- LeRoith D, Biessels GJ, Braithwaite SS, et al. Treatment of Diabetes in Older Adults: An Endocrine Society* Clinical Practice Guideline. J Clin Endocrinol Metab 2019;104:1520-74. [Crossref] [PubMed]
- Munoz N, Posthauer ME, Cereda E, et al. The Role of Nutrition for Pressure Injury Prevention and Healing: The 2019 International Clinical Practice Guideline Recommendations. Adv Skin Wound Care 2020;33:123-36. [Crossref] [PubMed]
- Fremmelevholm A, Soegaard K. Pressure ulcer prevention in hospitals: a successful nurse-led clinical quality improvement intervention. Br J Nurs 2019;28:S6-S11. [Crossref] [PubMed]
(English Language Editor: J. Gray)







