Thermal insulation during recovery from anesthesia: a systematic review and meta-analysis
Introduction
Studies have shown that hypothermia can occur in anesthetized patients during surgery and lead to chills, restlessness and other serious complications that can have a negative impact on both the surgery and postoperative recovery (1-3). At low body temperature, the skeletal muscle shows rhythmic contractions, which can lead to increased oxygen consumption, aggravate the burden on the heart, more likely induce acidosis and increase the risk of cardiovascular and cerebrovascular disease (4-6).
The cause is related to blood distribution during anesthesia, which is less to the kidney and liver and thus increases the metabolic time of narcotic drugs, increasing the postoperative recovery time (7-9). At the same time, intraoperative hypothermia also affects normal coagulation function and material metabolism of patients, thus increasing the surgical risk and affecting the patient’s prognosis.
Some studies have pointed out that perioperative hypothermia can increase the incidence of coagulation disease, acidosis, stroke, sepsis, pneumonia and myocardial infarction. Therefore, perioperative monitoring and maintaining normal body temperature are of great significance (10,11).
Thermal insulation (TI) is a special type of nursing for patients with hypothermia during surgery (10-12). Increasing the body temperature significantly improves the pharmacokinetics of narcotic drugs and prevents the delayed recovery caused by slow metabolism.
Several studies have evaluated the association between TI and stroke (2-4), with various research designs, recruitment and exclusion criteria, and measurements, but there is little meta-analyses. We therefore performed a meta-analysis to assess the correlation between TI and stroke. This research comprehensively analyzed effects of thermal insulation during recovery from anesthesia from the beginning of recovery to the end. We present the following article in accordance with the PRISMA reporting checklist (available at https://dx.doi.org/10.21037/apm-21-2716).
Methods
Search strategy
The meta-analysis was planned and implemented based on the PRISMA statement and the Cochrane Intervention System Evaluation Manual’s preferred reporting project. We searched for all articles published from January 2000 to January 2018 in PubMed, Springer, EMBASE and Chinese journal full-text databases. Two members of the team searched for articles independently using the following keywords: (I) thermal insulation OR TI; (II) recovery of anesthesia. In order to obtain higher accuracy and more relevant research, the reference list of each article retrieved was also reviewed.
Citation selection
All articles after the first screening were further selected by two other researchers. The titles and abstracts were independently and carefully screened. If the research met the inclusion criteria, full-text was obtained.
Inclusion criteria
- Randomized control trial study or a controlled clinical trial study.
- Comparison between patients with TI and control group.
- Availability of full text.
Exclusion criteria
- Not randomized.
- Patients with complications other than anesthesia recovery.
- Lack of outcome measures or comparable results.
The bibliography of each selected article was manually searched to determine other articles that met the selection criteria. If multiple publications were available, and the number of patients in the same group increased or the follow-up time was extended, only the data from the latest article was used for statistical analysis.
Data extraction
Two reviewers read the full text and extracted the relevant data of each study into a Microsoft Excel table: the name of the first author, publication year, year of onset, sample size (TI/control group), patient age range, and other information related to TI patient and control groups.
Statistical analysis
We used Review Manager (RevMan) 5.0 (Cochrane Collaboration, 2011) to conduct a meta-analysis to evaluate the differences between the TI and control groups and assess heterogeneity, sensitivity, and publication bias. The effect size of a numerical variable is expressed as the mean difference of the 95% confidence interval (CI); categorical data are expressed as relative risk (RR) with 95% CI. When data in individual studies were described in terms of median and range, they were converted to estimated mean ± standard deviation (SD) before analysis. We set the percentages at ≈25% (I2=25), 50% (I2=50) and 75% (I2=75), respectively, for low heterogeneity, medium heterogeneity and high heterogeneity. A χ2-based Q test was also performed to check for heterogeneity between studies. When the I2 value was >50, a random-effects model could be adopted when calculating moderate heterogeneity between studies, or we used a fixed-effects model. For results with significant heterogeneity among different studies, a sensitivity analysis tested the effect of each study on the aggregated data by omitting each study in turn using RevMan software. The quality evaluation of included articles used a bias risk table in the software for evaluation. In addition, we created a funnel plot to estimate possible publication bias.
Results
Search results
We conducted a preliminary search of 985 related titles and abstracts in the electronic databases. After a comprehensive review, seven papers finally met all the selection criteria. The other 978 articles were excluded because of repeated or irrelevant studies, no controls, incomplete data or comparisons, other operations, reviews, or incomplete articles. Figure 1 is a flowchart of the search process and the reasons for exclusion.
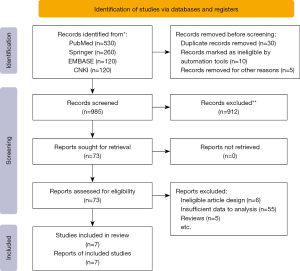
Characteristics of the included studies
Table 1 lists the parameters for each study that was included. All articles were published between 2000 and 2018, and the sample size was between 20 and 246. The meta-analysis had included 723 patients, with 360 in the TI group and 363 in the control group.
Table 1
| Study | Year | Language | Country | No. of patients (female/male) | Age range (years, mean) | Group | n | Study time period |
|---|---|---|---|---|---|---|---|---|
| Jun et al. (13) | 2018 | English | Korea | 20/30 | 65.5±9.1 | TI | 25 | January 2017 to March 2018 |
| Control | 25 | |||||||
| Li (14) | 2016 | Chinese | China | 68/52 | 40.8±13.3 | TI | 60 | May 2015 to August 2016 |
| Control | 60 | |||||||
| de Oliveira et al. (15) | 2017 | English | Brazil | 1/20 | 44.5±8.7 | TI | 10 | January 2012 to November 2013 |
| Control | 11 | |||||||
| Peng (16) | 2016 | Chinese | China | 92/68 | 47.8±11.6 | TI | 80 | April 2014 to June 2015 |
| Control | 80 | |||||||
| Torossian et al. (17) | 2016 | English | Germany | 188/58 | 45.7±14.4 | TI | 122 | September 2009 to May 2015 |
| Control | 124 | |||||||
| D’Angelo Vanni et al. (18) | 2007 | English | Brazil | 6/14 | 39.2±5.9 | TI | 10 | January 1999 to December 2005 |
| Control | 10 | |||||||
| Wang (19) | 2017 | Chinese | China | 36/70 | 44.6±2.7 | TI | 53 | October 2015 to March 2016 |
| Control | 53 |
TI, thermal insulation.
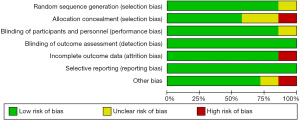
Quality assessment
The deviation table in the Review Manager 5.0 tutorial shows the criteria for evaluating design-related deviations to assess each study’s risk. The risk of bias in this study is shown in Figure 2, and the risk details of each article are shown in Figure 3. The bias and quality assessment graph showed almost no bias between participants and interviewees.

Results of meta-analysis
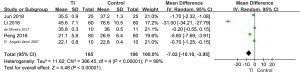
Meta-analysis of awakening time after anesthesia
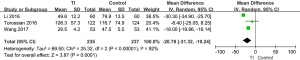
Five articles studied awakening time after anesthesia. Figure 4 is a forest plot for awakening time after anesthesia (min) in the TI and control groups. Four studies showed statistically significant differences in awakening time after anesthesia between groups. The meta-analysis also suggested a significant difference in awakening time after anesthesia in the TI and control groups [MD =–7.02, 95% CI: –10.10 to –3.95, P<0.00001; P for heterogeneity <0.00001, I2=99%]. The awakening time after anesthesia in the TI group was shorter than that of the control group.
Meta-analysis of length of stay in Postanesthesia Care Unit (PACU)
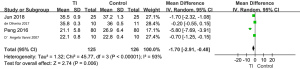
A forest plot of the meta-analysis of the length of stay in PACU (min) is presented in Figure 5. The results demonstrated that the length of stay in PACU in the TI group was shorter than that of the control group (MD =–20.78, 95% CI: –31.32 to –10.24, P=0.0001; P for heterogeneity <0.00001, I2=92%).
Meta-analysis of shivering rate
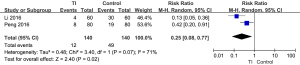
Four studies included the shivering rate (Figure 6). The overall result indicated a significant difference in shivering rate between patients with TI and controls (RR =0.25, 95% CI: 0.08 to 0.77, P=0.02; P for heterogeneity =0.07, I2=71%).
Sensitivity analysis
The meta-analysis showed high heterogeneity of awakening time after anesthesia (I2=99%). Figure 7 shows that the heterogeneity of awakening time after anesthesia might be attributed to the different results of each study. When the article of Li et al. in 2016 was excluded, I2 changed from 99% to 93%, which implied that the results of this meta-analysis were robust.
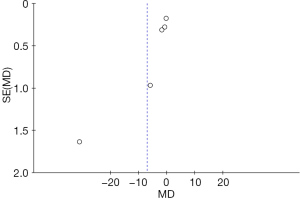
Bias analysis
A funnel plot of awakening time after anesthesia among patients with TI and controls is presented in Figure 8. All studies were included in the plot, which had good symmetry and little publication bias. The result of Begg’s test suggested that no significant evidence of potential publication bias existed (z=1.31; P=0.172). The result of Egger’s test suggested that no significant evidence of potential publication bias existed (t=1.19; P=0.321).
Discussion
In this study, we focused on the difference between thermal insulation and control after surgery in the recovery of anesthesia. General anesthesia reduces the normal metabolic rate of the human body by 30%, and is thus more likely to induce postoperative hypothermia than other forms such as intraspinal anesthesia (20-22). Poor management of hypothermia could increase the incidence of postoperative infection and fluid requirements, prolong anesthesia recovery time and hospital stay, and thus increase medical costs (23-25). Therefore, it is of great clinical significance to monitor and control hypothermia after general anesthesia.
The use of heating blankets, liquid heating and other methods to maintain the perioperative body temperature of patients improve the shivering of patients during operation, and shorten the time to extubation after operation (26-29). Maintaining normal body temperature during the perioperative period is vitally important to both improve the quality of anesthesia and reduce adverse reactions of patients.
This meta-analysis showed significant differences in awakening time after anesthesia and length of stay in PACU among patients in the TI group and the control group, which suggested that TI can reduce both awakening time and length of stay in PACU, and further promote the patient’s recovery. Our results concurred with Torossian’s research that TI is an effective measure during convalescence of anesthesia (17).
With regard to the shivering rate, the difference between the TI and control groups was also significant. Xiao et al. stated that TI could reduce the incidence of complications after anesthesia, which is consistent with our results (30). In order to avoid postoperative stroke, we should also avoid hypotension, low blood oxygen, hypoglycemia or hyperglycemia and preventive treatment with drugs can be conducted when necessary (29,30).
The normal value of central body temperature is about 37.5 °C. Every 1 °C increase or decrease in temperature will have a great impact on the body. The central temperature below 36 °C is called hypothermia. Hypothermia is a common phenomenon after surgery, especially after some long-time and traumatic surgery, the incidence can reach 50–70%. The loss of body temperature mainly occurs in every link before, during and after operation through conduction, convection and radiation. Therefore, we should intervene in controllable risk factors. Comprehensive heat preservation nursing measures start from many aspects. They use more humanized measures and more accurate and easy-to-operate equipment to achieve the purpose of heat preservation and temperature increase. In particular, using a variable temperature blanket can quickly increase the body surface temperature to achieve the purpose of heat preservation and temperature increase (28-30).
In conclusion, our meta-analysis showed that the application of TI during the recovery period of anesthesia is safe and effective, and the results were consistent with those of other studies. The heterogeneity of the meta-analysis was low, and according to both the funnel chart and the Berger test, there was no publication bias, which better supports our conclusion. The main limitation of this study is that more parameters of the TI and control groups need to be analyzed and evaluated in the future. We intend to carry out further study to elucidate this issue.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://dx.doi.org/10.21037/apm-21-2716
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/apm-21-2716). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Li FU, Anesthesiology DO. Clinical analysis of the effect of heat preservation and nursing on intraoperative stress and postoperative revival in patients with general anesthesia. China Continuing Medical Education 2018;28:32-5.
- Xu L, Su YC, Liu P. The Retrospective Analysis on the Effect of Different Thermal Way in Chest and Abdomen Surgery of Newborn. Medical Innovation of China 2017;14:87-93.
- Xingwei LI, Analgesia DO, Hospital ZM. Effects of comprehensive thermal insulation measures on body temperature in elder patients of orthopedic surgery under general anesthesia. Chinese Journal of Geriatric Care 2013;21:93-8.
- Peng YN, Bo JH, Yuan GJ, et al. Study on influence of comprehensive thermal insulation on body temperature of patients undergoing abdominal surgery. Chinese Journal of Nosocomiology 2014;33:128-33.
- Xiao Y, Xian CJ, Li HY, et al. Influence of thermal insulation techniques on body temperature of renal transplant patients and stress responses during perioperative period. Chinese Journal of Nosocomiology 2012;18:33-8.
- Song T, Shen J, Cai HF, et al. Impact analysis insulation intervention to abdominal surgery perioperative body temperature to the newborn. Journal of Clinic Nursing’s Practicality 2017;14:32-3.
- Zhang J, Sun ML, Li F. Application of Comprehensive Thermal Insulation Measure in Fast Track Surgery for Patients Undergoing Retroperitoneal Laparoscopic Adrenal Gland Resection. Medical Innovation of China 2017;22:128-31.
- Zhang F, Lin Q, Zeng M, et al. Effect of Thermal Insulation Measures on Operation of Patients With Lung Cancer Under General Anesthesia. China Health Standard Management 2018;23:38-44.
- Huang Q, Li D, Zhu Z, et al. Effects of anesthesia body temperature change on analepsia effect and extubation time after anesthesia. China Medicine and Pharmacy 2019;34:31-6.
- Huang L, He XY, Huang HY. Effect Analysis of Comprehensive Thermal Insulation Measures in Prevention of Shivering after PACU General Anesthesia. Medical Innovation of China 2014;11:51-8.
- Casati A, Fanelli G, Ricci A, et al. Shortening the discharging time after total hip replacement under combined spinal/epidural anesthesia by actively warming the patient during surgery. Minerva Anestesiol 1999;65:507-14. [PubMed]
- He LP, Liu PZ. Influences of thermal insulation at different temperatures on inflammatory response and postoperative reha-bilitation in children undergoing congenital dislocation hip surgery. Chinese Journal of Nursing 2017;25:75-8.
- Jun JH, Chung MH, Kim EM, et al. Effect of pre-warming on perioperative hypothermia during holmium laser enucleation of the prostate under spinal anesthesia: a prospective randomized controlled trial. BMC Anesthesiol 2018;18:201. [Crossref] [PubMed]
- Li Y. Insulation care awakening intraoperative and postoperative stress in patients with general anesthesia. China Modern Medicine 2016;23:194-6.
- de Oliveira SA, Lucio LM, Modolo NS, et al. The Humidity in a Low-Flow Dräger Fabius Anesthesia Workstation with or without Thermal Insulation or a Heat and Moisture Exchanger: A Prospective Randomized Clinical Trial. PLoS One 2017;12:e0170723 [Crossref] [PubMed]
- Peng W. Effect of perioperative heat preservation nursing on the quality of anesthesia recovery in patients with general anesthesia. Internal Med 2016;11:799-800.
- Torossian A, Van Gerven E, Geertsen K, et al. Active perioperative patient warming using a self-warming blanket (BARRIER EasyWarm) is superior to passive thermal insulation: a multinational, multicenter, randomized trial. J Clin Anesth 2016;34:547-54. [Crossref] [PubMed]
- D'Angelo Vanni SM, Castiglia YM, Ganem EM, et al. Preoperative warming combined with intraoperative skin-surface warming does not avoid hypothermia caused by spinal anesthesia in patients with midazolam premedication. Sao Paulo Med J 2007;125:144-9. [Crossref] [PubMed]
- Wang J. Effect of heat preservation nursing on intraoperative stress and postoperative recovery in patients with general anesthesia. Journal of Clinical Medicine in Practice 2017;21:179-80.
- Cheng SH, Tong QZ, Zhao Y, et al. Effect of Comprehensive Thermal Insulation Measures on Strabotomy under General Anesthesia in Children. Practical Clinical Medicine 2018;55:128-32.
- Xie S, Zhou Q, Huang Y, et al. Effect of perioperative thermal insulation nursing on stress response and recovery in patients undergoing general anesthesia. Contemporary Medicine 2019;15:23-7.
- Farong Z, Liang H, Zhou J, et al. Effect of Intravenous Fast Tracking Anesthesia Combined with Combined Heat Preservation on Homeostasis in Elderly Patients Undergoing Spinal Surgery. Journal of Ningxia Medical University 2016;112:38-44.
- Liu H, Liang H, Zhou J. Intravenous fast-tracking anesthesia combined with composite thermal insulation on internal environment homeostasis and postoperative cognitive dysfunction in elderly patients undergoing spinal surgery. Medical Journal of National Defending Forces in Northwest China 2016;33:38-42.
- Deng QH. The effect of integrated thermal insulation measures during surgery on trauma patients’ temperature and anesthesia recovery time. Journal of Qiqihar University of Medicine 2015;118:88-93.
- Wu XH, JMa J, Wang T, et al. Effect of active thermal insulation intervention measures preventing intraoperative hypothermia in patients with general anesthesia. Chinese contemporary medicine 2019;30:256-8.
- Chen SZ, Cai H. Affect of thermal insulation measures on anesthesia recovery general anesthesia of elderly patients’ body temperature. Jilin Medical Journal 2015;16:150-1.
- Ma WW, Miao H, Room O. Thermal insulation nursing and the effect on adverse reactions in patients undergoing surgery for thyroid tumors under general anesthesia. Chinese Journal of Clinical Oncology and Rehabilitation 2018;3:83-6.
- Deping LV, Xiao H, Yang Y. The nursing effects of compound thermal insulation measures on body temperature control in patients receiving abdominal surgery. Hebei Medical Journal 2018;2:151-7.
- Li JF. Effect of comprehensive thermal insulation nursing on fluctuation of vital signs and degree of chill after anesthesia in transurethral resection of prostate patients. Nursing Practice and Research 2018;23:111-2.
- Xiao WJ, Fang T, Anesthesiology DO. Effect of different thermal insulation measures on the recovery from anesthesia in patients with lung cancer under general anesthesia. Chinese Journal of Clinical Oncology and Rehabilitation 2018;25:128-34.
(English Language Editor: K. Brown)