
A case report on the treatment of total placenta increta after transvaginal delivery with integrated traditional Chinese and western medicine
Introduction
Placenta increta refers to a group of diseases in which trophoblast cells invade part or all of the myometrium. In recent years, the disease has been collectively referred to as placenta accrete spectrum (PAS) (1). However, the clinical treatment of total placenta increta after vaginal delivery is a thorny issue in obstetrics, and to date, no specific guidelines or expert consensus as to its treatment exist. In recent years, with the adjustment of the fertility policy, the increase in the rate of cesarean section, and the increase in uterine cavity operations, the incidence of placenta increta has also gradually increased (2). The pre-delivery diagnosis of this disease mainly relies on imaging examinations that have limited diagnostic value. Some missed cases are only diagnosed during delivery. Its unpredictability and suddenness make pre-plans insufficient and easily lead to postpartum hemorrhage, infection, and even sepsis. The disease is life-threatening (3).
Hysterectomy is currently a common method for the treatment of PAS, but it can cause maternal loss of fertility (4). Further, 40% to 50% of patients will still suffer from serious postoperative complications, and 7% of pregnant women will die in the early stage (4). Some cases implement placenta in-situ preservation and expectant treatment. Serious complications may occur during conservative treatments, such as late postpartum hemorrhages, severe infection, sepsis, septic shock, peritonitis, uterine necrosis, fistula formation, adjacent organ damage, acute pulmonary edema, acute renal failure, deep vein thrombosis, pulmonary embolism, and death (5). Given the significance of uterine preservation and the adverse consequences of conservative clinical treatments, a comprehensive treatment method urgently needs to be established that not only preserves the uterus, but also reduces the short- and long-term complications as much as possible in clinical settings. By reviewing the relevant literature and accumulating clinical experience, we successfully integrated traditional Chinese and Western medicine to treat total placenta increta. This report outlines the case an advanced-age woman with whole placenta increta who underwent vaginal delivery after vaginal delivery.
We present the following article in accordance with the CARE reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-21-3794/rc).
Case presentation
The 36-year-old patient was admitted to hospital with “menopause for 37+1 weeks, vaginal fluid for 10+ h”. The patient had not undergone regular check-ups during pregnancy. At OCTT, the patient was diagnosed with gestational diabetes. Her gestational diabetes was managed, but her blood sugar was not strictly controlled. 10+ hours before admission, the patient noted vaginal fluid (clear in color, and thin in quality), and experienced irregular contractions and vaginal bleeding. A pedestrian abortion was performed once (details unknown), and the patient denied any history of hemorrhage and infection.
The results of the admission examination were as follows: Temperature: 36.0 °C; Pulse: 100 beats/min; blood pressure (BP): 129/88 mmHg (1 mmHg =0.133 kPa); height: 160 cm; weight 64 kg; uterine contractions: irregular; uterine fundus height: 32 cm; abdominal circumference: 104 cm; fetal position: left occiput anterior (LOA); fetal heart rate: 142 beats/min; fetal weight: 2,500 g; cervical score: 4 points; and fetal membranes: broken. At admission, routine blood test was taken to examine coagulation function, liver function and renal function, and the results were all normal. The diagnosis at admission was as follows: (I) G3P1 37+2 weeks of gestation LOA; (II) premature rupture of fetal membranes; and (III) gestational diabetes.
The patient and her family members had a strong desire for vaginal delivery, but the fetal membranes were now broken. To avoid prolonging the rupture of the membranes and causing a uterine cavity infection, antibiotics were administered prophylactically. Generally, if the rupture of the membranes does not enter the labor process within 24 h, a small dose of oxytocin is given to induce labor. The first stage of labor lasted 6.5 h, the second stage of labor lasted 14 min with normal childbirth, and the third stage lasted 15 min after the fetus was delivered.
As there was about 100 mL of active vaginal bleeding, and no signs of placental dissection, after strict disinfection, the uterine cavity was explored with bare hands, and the placenta was found to be tightly adhered to the uterine wall, and difficult to peel off. Given the possibility of placenta increta, a bedside B-ultrasound was conducted. The ultrasound revealed placental-like tissue echoes from the right side of the uterine cavity to the bottom of the uterus, which was about 87 mm × 92 mm × 101 mm in size, an unclear myometrium boundary, and an abundant blood flow signal, suggesting placenta increta with a large area. At this time, uterine contraction was poor, and the total amount of active bleeding was 500 mL. Hemapex was given to promote uterine contractions, and start the rescue plan for postpartum hemorrhage. We also communicated and explained the issue to the patient and her family. After the communication, conservative treatment was strongly requested, and a 1-time intrauterine balloon compression was performed to stop the bleeding.
The urgent blood routine work results were as follows: white blood cell (WBC) count: 12.91×109/L; neutrophil (NEU) percentage: 89.40%; hemoglobin: 121 g/L; APTT 36: 80 s; D-dimer: 5.45 mg/L; and normal liver and kidney function. Due to the large area of placenta increta and postpartum hemorrhage, after uterine balloon compression to stop the bleeding, the uterus contracted well. There was a small amount of vaginal bleeding, dark red in color. Cefazolin and tinidazole were administered to prevent infection. The uterine balloon was taken out 12 h postpartum. To prevent late postpartum hemorrhage, the patient and her family members agreed to her undergoing double lateral uterine artery embolization.
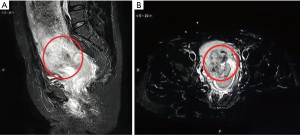
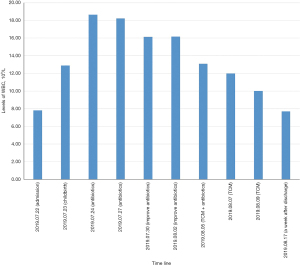
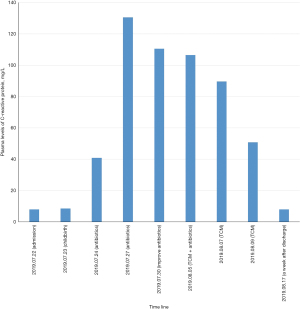
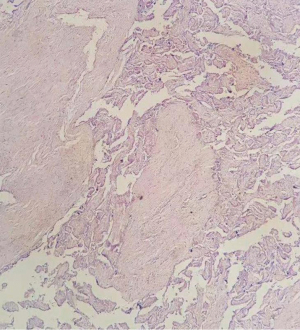
A preoperative pelvic MR plain scan showed a uterine hemorrhage, and an uneven signal in the uterine cavity, suggesting placenta increta (see Figure 1). On the first day after childbirth, the breasts secreted a small amount of milk, the abdomen was soft, the uterus was well contracted and flat, the umbilical cord was flat, the uterine contour was clear, there was no tenderness, the lochia was red in color and medium in volume, there was no peculiar smell, and the patient had a fever (her highest body temperature on the second day after childbirth was 39 °C). The re-checked routine blood results were as follows: WBC: 18.64×109/L; NEU percentage: 87.3%; C-reactive protein (CRP): 40.80 mg/L; and procalcitonin: 1.53 pg/mL. We changed the antibiotics to cefoperazone and sulbactam. A physical examination revealed a soft abdomen, poor uterine contraction, a clear outline of the uterus, tenderness, a moderate amount of red lochia, and no peculiar smell.
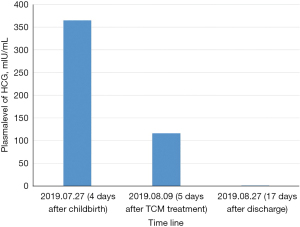
On the fourth day after delivery, the patient’s body temperature fluctuated between 38–38.5 °C. To remove the lesion, an ultrasound-guided clamp operation was conducted, but failed. The patient’s body temperature suddenly increased to 39.5 °C on the night of the clamp operation. The blood test results were as follows: WBC: 18.22×109/L; NEU percentage: 91.8%; CRP: 130.52 mg/L; procalcitonin: 1.99 pg/mL; blood HCG: 364.6 mIU/mL; and. blood culture: normal. A B-ultrasound re-examination showed the following: (I) a puerperal uterus; and (II) a fundus solid echo cluster (approximately 107 mm × 136 mm × 89 mm in size, with multiple strong echo spots inside, a visible comet tail sign, and an unclear boundary myometrium with little punctuated blood flow signal around it). The antibiotic was replaced with meropenem.
On the seventh day after delivery, the patient’s body temperature continued to fluctuate between 38–39 °C, and the patient was anxious, irritable, and depressed. After the Western medicine treatment, the patient had a repeated fever, the placenta was not delivered, and the serum inflammation index had decreased significantly. The Chinese medicine doctor observed mental irritability, thirst and polydipsia, a high fever, a poor diet, uterine contraction, uterine contraction, between the umbilical, shame of the uterus, a clear outline, light tenderness, yellow urine, bowel movements, a dark red tongue, yellow fur, and a stringy pulse. The diagnosis of the Chinese medicine doctor was postpartum fever-damp and heat, blood stasis, and yin deficiency.
To treat heat-clearing and dampness, promote blood circulation and nourish the yin, Simiao Yongan decoction was prescribed. The recipe is as follows: honeysuckle (20 g), turtle shell (6 g for the first decoction), angelica (20 g), scrophulariaceae (20 g), magnolia root (10 g), atractylodes (12 g), grass cardamom (10 g), Rehmannia glutinosa (10 g), and cat’s claw (20 g). One dose of the concoction was taken per day in 3 divided doses.
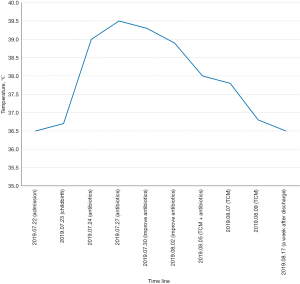
1 day after taking the medicine, the patient’s body temperature dropped below 38 °C (see Figure 2), the antibiotics were stopped, and the oral administration of the traditional Chinese medicine was continued. Three days after taking the medicine, the patient’s body temperature had completely returned to normal. The results of further routine blood tests were as follows: WBC: 12.01×109/L; NEU percentage: 84.10%; and CRP: 89.70 mg/L. 5 days after taking the medicine, the results of further blood tests were as follows: WBC: 10.02×109/L; NEU percentage: 79.9%; CRP: 50.7 mg/L; and blood HCG: 116.19 mIU/mL. The B-ultrasound results were as follows: postpartum uterus (about 133 mm × 117 mm × 83 mm in size), uneven echo of the uterine wall, unclear endometrium line, strong echoic masses in the uterine cavity (with a range of about 106 mm × 90 mm × 58 mm), an unclear myometrium boundary, and no obvious blood flow signal. After being informed of her condition, the patient asked to be discharged from hospital.
1 week later, the patient had normal routine blood test results (Figures 3,4), normal CRP levels (Figure 5), and normal procalcitonin levels. Fetal membrane-like tissue (about 5 cm × 10 cm in size) was discharged 10 days after discharge, and organized placental tissue (about 10 cm × 8 cm in size) was discharged 17 days after discharge from the hospital, accompanied by a foul smell, but not much bleeding. The pathological findings of the discharge were as follows: placental tissue and smooth muscle tissue. The smooth muscle was infiltrated by a large number of inflammatory cells, some of which were degenerated and necrotic (see Figure 6).

1 month after discharge from the hospital, the lochia was clean, and the follow-up B-ultrasound showed that the uterus (which was about 71 mm × 69 mm × 58 mm in size) was in the anterior position, normal in shape, and had a smooth capsule. Further, the echo of the uterine wall was normal, the endometrium was clear and centered, and there was an irregular liquid dark area (with a range of about 24 mm × 13 mm) in the uterine cavity near the fundus. Additionally, multiple strong echo light spots were observed near the fundus of the uterine cavity, and no obvious blood flow signals were detected. The double ovaries were not found. The patient had blood HCG of 2.19 mIU/mL (Figure 7), no lower abdominal pain, and abnormal vaginal bleeding. The patient resumed a normal sex life with strict contraception.
About 4 months postpartum, the B-ultrasound showed that the uterus was normal, and the endometrial line was clear and centered. Further, no abnormal blood flow signals were detected. At 5 months postpartum, the patient’s menstruation cycle had returned; the menstrual volume had decreased by about 1/3, the menstruation period was 5 days, there were no changes compared to before, the menstrual color was dark red, the blood clots were trapped, the patient occasionally felt intermittent but tolerable pain in the lower abdomen, the amount of leucorrhea was moderate, the color was yellow, and there was no peculiar smell and no vulva itching. All procedures performed in this study were in accordance with the ethical standards of national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
In the past 40 years, the incidence of placenta increta has increased by about 10 times (6). A 2016 study showed that the incidence of placenta increta in the United States had reached 1 in 272 (7), and the incidence of PAS in Hong Kong, China had also increased from 1 in 5,882 in 1999–2003 to 1 in 1,266 in 2009–2013 (8). Compared to the placenta increta disease found during cesarean section, total placenta increta found after vaginal delivery is sudden, blind, and often, only the midwife is present. PAS patients are prone to major bleeding, and may need blood transfusions. PAS can also easily lead to the death of pregnant women. Additionally, PAS increases the chance of hysterectomy and prolongs the hospitalization time, leading to many undesirable outcomes. Thus, the treatment of total placenta increta after vaginal delivery is still an urgent problem in obstetrics. Ultrasonography is a common method to detect and confirm placenta increta. During placental increta, ultrasound mainly manifests as disappearance or irregularity of the posterior placenta space, uneven echo of the myometrium below the decidua, loss or complete interruption of the muscle layer, and CDFI shows that there is abundant blood flow and blood behind the placenta or in the placental parenchyma sinus, blood flow is turbulent and turbulent (9).
At present, partial or total uterine resection is still the mainstream treatment. As a conservative treatment, methotrexate, mifepristone have been used empirically in the past (10,11). However, it is no longer recommended, as in recent years, it has been shown to cause bone marrow suppression in patients and can lead to other complications. The expected treatment of indwelling placenta in situ has follow-up difficulties, which leads to the neglect of the condition. Further, prolonged stress can increase the risk of postpartum depression. The risks include medical disputes, unpredictable late postpartum hemorrhage, secondary infections leading to sepsis, and life-threatening and other serious adverse consequences. At present, there are no relevant guidelines and no expert consensus on the choice of treatment for placenta increta after vaginal delivery. Intervention and physical therapy can be adopted for postpartum hemorrhage caused by placenta increta in situ, but the retention of the lesions can lead to infection. Additionally, antibiotics are not effective.
This patient was diagnosed with placenta increta and active vaginal bleeding after delivery. An emergency uterine artery embolization was performed to stop the bleeding. A postoperative clamp was added to remove the residual placental tissue, but later failed. Postoperatively, the patient had a repeated fever, and the anti-infective treatment effect was not good.
As the long-term use of antibiotics can lead to a flora imbalance and fungal infections, the patient asked for a consultation with Professor Liu Shangyi, a master of traditional Chinese medicine. Professor Liu believes that the postpartum wasting of qi and blood, the emptiness of veins, inadequate physiology, the infirmity of Wei Yang, the long-term infusion of liquid in the body, flowing through the whole body, water dampness, and yin and evil enter due to deficiency, directly offend the uterus, stay in the Chongren, the blood vessels, and enter the internal heat, causing the postpartum yin and blood to become suddenly deficient. The yin does not agglomerate the yang, the yang is not attached, and is deficient. The yang floats outside, and the blood chamber is open after childbirth. The water is damp and cold, the blood vessels are stagnated, the siltation is blocked, the qi is blocked, the camp and the guard are in harmony, and fever is caused. In accordance with the rule of “do not be restricted to the postpartum, and do not forget the postpartum”, and combined with the tongue coating and pulse condition, Professor Liu prescribed the Simiao Yongan decoction. Honeysuckle, angelica, and scrophulariaceae clear away heat, detoxify, promote blood circulation, and remove blood stasis, while turtle carapace and rehmannia glutinosa reduce steaming, soften and clear knots, nourish yin and yang, relieve swelling, reduce swelling and detoxify. The combined use of various medicines can strengthen the body and eliminate evils, and children’s urine can be used as a guide to treat the combination of the 3 evils of “toxin, blood stasis, and dampness”. Traditional Chinese medicine masters in obstetrics adopt a flexible use of treatments according to individual conditions.
The Simiao Yongan decoction was first recorded in “The Secret Biography of Huatuo’s Divine Doctor”, written by Sun Simiao in the Tang Dynasty, and later included in Bao Xiangao’s “New Compilation of Prescriptions” in the Qing Dynasty, where it was officially named. The main treatment of this prescription is the prevention of gangrene caused by a heat toxin, which has the effects of clearing away heat and detoxifying, promoting blood circulation, and removing blood stasis (12). Modern pharmacological studies have confirmed that the prescription has anti-inflammatory effects, protects blood vessels, stabilizes arterial plaque, and is an anticoagulant (13,14). It is widely used in dermatology, endocrinology, and cardiovascular medicine (15-17), but it is rarely used in obstetrics.
Urine is widely used in Chinese medicine and has a long history. It has always been valued by physicians of past generations. “Shen Nong’s Materia Medica: Human Urine” states, “Human urine is the turbid body fluid that seeps into the bladder. Its taste is salty, but there is no cold air and [it is] not poison[ious]. It is a holy medicine for eliminating fatigue, steaming bones, coughing and vomiting blood, and women’s postpartum blood dizziness.” Zhu Danxi’s “Materia Medica Supplement” states that a child’s urine provides the “fastest reduction in fire”, and is a good medicine to treat postpartum fever and postpartum lochia. Gong’s day states, “because of mother and childbirth, blood in the abdomen flows into the placenta and is swollen by blood. It is hard to get off the old placenta, but when Jin San loses blood in the placenta, the belt will break.” In Jin San prescriptions, a boy’s urine is used as medicine, and blood circulation is mainly used to treat various postpartum diseases. Its “cold” nature can reduce fire and cure heat syndrome, which is in line with the treatment principle of “hot one is cold,” degrade heat toxins, promote blood circulation, remove blood stasis, and promote the elimination of cell clothes.
Congestion refers to the effect of removing dampness and evil. For patients with total placenta in vaginal delivery, traditional Chinese medicine adopts a holistic view. The traditional Chinese medicine is taken orally due to the human physique. It removes blood stasis and relieves symptoms, so that the placenta and its implantation site are necrotic and detached, the discharge of placenta and infection foci are promoted, the body’s righteousness is then replenished, the blood stasis toxins are expelled, and the body heat is reduced. The effect is definite. This case provides a new treatment choice for the treatment of placenta increta and its complications after vaginal delivery. The integrated Chinese and Western medicine improve the efficiency of the conservative treatment, improves the quality of life of patients after childbirth, promotes the expertise of famous doctors, and serves patients. In a previous study, Jiang et al. also demonstrated that integrated Chinese and Western medicine treated placenta increta effectively (18). They treated patients with methotrexate and mifepristone, combined with Yiqi Huoxue Zhuyu Decoction, and achieved satisfying outcome (18). The outcome of the case in our report was similar with Jiang’s study. In the future, we will include more cases and further examine the mechanism.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-21-3794/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-21-3794/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Silver RM, Branch DW. Placenta Accreta Spectrum. N Engl J Med 2018;378:1529-36. [Crossref] [PubMed]
- Khaliq Showman HA, Alizzi FJ, Helmi ZR, et al. Placenta accrete spectrum disorders: A single centre experience over four years in the view of international guidelines. J Pak Med Assoc 2019;69:S68-S72. [PubMed]
- Yasin N, Slade L, Atkinson E, et al. The multidisciplinary management of placenta accreta spectrum (PAS) within a single tertiary centre: A ten-year experience. Aust N Z J Obstet Gynaecol 2019;59:550-4. [Crossref] [PubMed]
- Morlando M, Collins S. Placenta Accreta Spectrum Disorders: Challenges, Risks, and Management Strategies. Int J Womens Health 2020;12:1033-45. [Crossref] [PubMed]
- Di Mascio D, Cali G, D'Antonio F. Updates on the management of placenta accreta spectrum. Minerva Ginecol 2019;71:113-20. [Crossref] [PubMed]
- Solheim KN, Esakoff TF, Little SE, et al. The effect of cesarean delivery rates on the future incidence of placenta previa, placenta accreta, and maternal mortality. J Matern Fetal Neonatal Med 2011;24:1341-6. [Crossref] [PubMed]
- Mogos MF, Salemi JL, Ashley M, et al. Recent trends in placenta accreta in the United States and its impact on maternal-fetal morbidity and healthcare-associated costs, 1998-2011. J Matern Fetal Neonatal Med 2016;29:1077-82. [Crossref] [PubMed]
- Cheng KK, Lee MM. Rising incidence of morbidly adherent placenta and its association with previous caesarean section: a 15-year analysis in a tertiary hospital in Hong Kong. Hong Kong Med J 2015;21:511-7. [Crossref] [PubMed]
- Lerner JP, Deane S, Timor-Tritsch IE. Characterization of placenta accreta using transvaginal sonography and color Doppler imaging. Ultrasound Obstet Gynecol 1995;5:198-201. [Crossref] [PubMed]
- Einerson BD, Branch DW. Surgical Management of Placenta Accreta Spectrum. Clin Obstet Gynecol 2018;61:774-82. [Crossref] [PubMed]
- Morgan M, Atalla R. Mifepristone and Misoprostol for the management of placenta accreta - a new alternative approach. BJOG 2009;116:1002-3. [Crossref] [PubMed]
- Li L, Chen X, Su C, et al. Si-Miao-Yong-An decoction preserves cardiac function and regulates GLC/AMPK/NF-kappaB and GLC/PPARalpha/PGC-1alpha pathways in diabetic mice. Biomed Pharmacother 2020;132:110817. [Crossref] [PubMed]
- Zhao Y, Sun D, Chen Y, et al. Si-Miao-Yong-An Decoction attenuates isoprenaline-induced myocardial fibrosis in AMPK-driven Akt/mTOR and TGF-beta/SMAD3 pathways. Biomed Pharmacother 2020;130:110522. [Crossref] [PubMed]
- Zhu ZB, Song K, Huang WJ, et al. Si-Miao-Yong-An (SMYA) Decoction May Protect the Renal Function Through Regulating the Autophagy-Mediated Degradation of Ubiquitinated Protein in an Atherosclerosis Model. Front Pharmacol 2020;11:837. [Crossref] [PubMed]
- Cui W, Xin S, Zhu L, et al. Si-Miao-Yong-An Decoction Maintains the Cardiac Function and Protects Cardiomyocytes from Myocardial Ischemia and Reperfusion Injury. Evid Based Complement Alternat Med 2021;2021:8968464. [Crossref] [PubMed]
- Liu Z, Zhang Y, Zhang R, et al. Promotion of classic neutral bile acids synthesis pathway is responsible for cholesterol-lowing effect of Si-miao-yong-an decoction: Application of LC-MS/MS method to determine 6 major bile acids in rat liver and plasma. J Pharm Biomed Anal 2017;135:167-75. [Crossref] [PubMed]
- Zhang C, Xu Y, Tan HY, et al. Neuroprotective effect of He-Ying-Qing-Re formula on retinal ganglion cell in diabetic retinopathy. J Ethnopharmacol 2018;214:179-89. [Crossref] [PubMed]
- Jiang Y, Zhu HP. Clinical observation on the treatment of placental implants with integrated traditional Chinese and western medicine. Chinese Emergency in Traditional Chinese Medicine 2014;23:124-5.
(English Language Editor: L. Huleatt)


