
Ultrasound-guided 3-in-1 trigger point injection for treating myofascial pain syndrome in muscles of the lateral scapular area: a case report
Introduction
Myofascial pain syndrome (MPS) is the most commonly diagnosed musculoskeletal condition (1). Poor posture is the primary cause of MPS (1). Due to the prevalence of office work in the modern work force, workers tend to spend a lot of time sitting in the office in front of computers during their working hours. Many sit in an incorrect posture, such as with rounded shoulders (i.e., internal shoulder rotation) or with cervical kyphosis (2). Additionally, excessive office work causes prolonged shoulder adduction, which, along with adduction, causes excessive elongation of the shoulder external rotators and adductors and seems to be associated with MPS in the deltoid, infraspinatus, and teres major muscles.
Because the deltoid, infraspinatus, and teres major muscles are located close together, treating all of these muscles evenly with a blind technique is not easy. Additionally, trigger point injection (TPI) with a blind technique can induce various complications, including pneumothorax as well as nerve or vascular injury (3,4). Ultrasound (US)-guided TPI allows for accurate injection of the targeted muscles and has been shown to prevent complications.
In the current case report, we introduce the use of the TPI technique in three muscles (i.e., the deltoid, infraspinatus, and teres major muscles) with the same sonographic view for the purpose of treating MPS in the lateral scapular area. We present the following case in accordance with the CARE reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-22-189/rc).
Case presentation
A 48-year-old woman presented with dull pain in the right lateral scapular area that had persisted for four months (Figure 1). The patient visited the rehabilitation department of our hospital on December 4, 2021, at which time her numeric rating scale (NRS) pain score was 5. The pain was not aggravated or relieved by any specific posture or action, and the patient experienced persistent pain even in a resting posture.

On physical examination, taut bands were found in the muscles of the right lateral scapular area, and the muscles were tender on palpation with reproduction of the usual pain. External rotation and abduction of the right shoulder aggravated the pain. The patient’s range of motion was normal. No motor weakness or sensory deficit was observed. Spurling test results were negative. Cervical spine magnetic resonance imaging revealed no abnormal findings, including stenosis and herniated disc. Electrodiagnostic testing of her right upper extremity was unremarkable. Based on her pain characteristics and physical examination findings, we diagnosed her with MPS in the muscles of the right lateral scapular area (deltoid, infraspinatus, and teres major muscles).
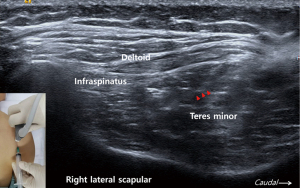
US examination of the lateral scapular area was unremarkable. Under US guidance (18-MHz linear transducer, S2000, Siemens; Seoul, South Korea), a TPI was administered with the patient in the prone position and the right upper extremity in a neutral position at the side of the body (Figure 2) (Video 1). The US probe was placed on the right lateral scapular area at the sagittal plane. The deltoid, infraspinatus, and teres minor muscles were identified near the right lateral scapular margin. The most superficial layer is the deltoid muscle. The infraspinatus and teres minor muscles are located under the deltoid muscle. A mixed solution of 1 mL of 2% lidocaine and 2 mL of normal saline was injected layer-by-layer into the three muscles within the same sonographic view. Fifteen minutes after the TPI, the pain completely disappeared. Two weeks after the TPI, the patient still experienced no pain. At the 1-month follow-up (F/U), the patient reported slight initial pain (NRS score, 1). The patient reported no adverse or unanticipated events after undergoing TPI.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Herein, we report the successful treatment of MPS in the muscles of the lateral scapular area using US-guided TPI administered to the deltoid, infraspinatus, and teres major muscles. This procedure was conducted with a single injection performed under US guidance within a single sonographic view.
Many previous studies have demonstrated the usefulness of US-guided TPI for controlling pain in MPS (5-8). Moreover, pneumothorax, nerve injury, vascular injury, and hematoma can be avoided by meticulous US scanning. In addition, implementing US-guided TPI allows clinicians to use less local anesthetic, which can be helpful in preventing systemic anesthetic toxicity (9). Most previous studies have performed TPI in only one muscle per injection (5,6,8). However, MPS occurs in several muscles, and the simultaneous treatment of these muscles enhances the therapeutic effects of TPI. Moreover, when administering TPI to one muscle with a single injection, the position of the US probe has to be moved every time each muscle is treated. This increases the procedural time as well the associated risk of infection (10). In contrast, TPI administered to multiple muscles with a single injection within a single US plane would be expected to overcome the disadvantages of pre-existing (i.e., established) US-guided TPI methods.
In the current report, we performed TPI in the deltoid, infraspinatus, and teres major muscles using a single injection. Our novel technique, which applies TPI to multiple muscles through a single injection, reduces procedural time as well as pain during TPI. Our US-guided 3-in-1 TPI technique is a useful therapeutic option for patients with MPS of the muscles in the lateral scapular area. However, our report is limited in that we present a case study rather than a rigorously designed epidemiologic investigation. Well-designed clinical trials enrolling large numbers of subjects are required in the future in order to conclusively demonstrate the usefulness of our TPI technique.
Acknowledgments
Funding: The present study was supported by a National Research Foundation of Korea grant funded by the Korean government (Grant No. 2019M3E5D1A02068106).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-22-189/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-22-189/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cao QW, Peng BG, Wang L, et al. Expert consensus on the diagnosis and treatment of myofascial pain syndrome. World J Clin Cases 2021;9:2077-89. [Crossref] [PubMed]
- Nejati P, Lotfian S, Moezy A, et al. The relationship of forward head posture and rounded shoulders with neck pain in Iranian office workers. Med J Islam Repub Iran 2014;28:26. [PubMed]
- Ahiskalioglu EO, Alici HA, Dostbil A, et al. Pneumothorax after trigger point injection: A case report and review of literature. J Back Musculoskelet Rehabil 2016;29:895-7. [Crossref] [PubMed]
- Kim JB, Chang MC. Spinal cord injury by direct damage during trigger point injection: a case report. J Int Med Res 2021;49:3000605211012367. [Crossref] [PubMed]
- Anwar N, Li S, Long L, et al. Combined effectiveness of extracorporeal radial shockwave therapy and ultrasound-guided trigger point injection of lidocaine in upper trapezius myofascial pain syndrome. Am J Transl Res 2022;14:182-96. [PubMed]
- Niraj G, Collett BJ, Bone M. Ultrasound-guided trigger point injection: first description of changes visible on ultrasound scanning in the muscle containing the trigger point. Br J Anaesth 2011;107:474-5. [Crossref] [PubMed]
- Ricci V, Ricci C, Gervasoni F, et al. From Histo-anatomy to Sonography in Myofascial Pain Syndrome: EURO-MUSCULUS/USPRM Approach. Am J Phys Med Rehabil 2022; Epub ahead of print. [Crossref] [PubMed]
- Tantanatip A, Patisumpitawong W, Lee S. Comparison of the Effects of Physiologic Saline Interfascial and Lidocaine Trigger Point Injections in Treatment of Myofascial Pain Syndrome: A Double-Blind Randomized Controlled Trial. Arch Rehabil Res Clin Transl 2021;3:100119. [Crossref] [PubMed]
- Torp KD, Metheny E, Simon LV. Lidocaine Toxicity. Treasure Island, FL, USA: StatPearls Publishing, 2022.
- Alakkad H, Naeeni A, Chan VW, et al. Infection related to ultrasound-guided single-injection peripheral nerve blockade: a decade of experience at toronto Western hospital. Reg Anesth Pain Med 2015;40:82-4. [Crossref] [PubMed]


