
Experiences of caregivers and hospice leaders with telehealth for palliative care: a mixed methods study
Introduction
The COVID-19 pandemic catapulted telehealth into everyday use for health care worldwide to limit patient and health care worker exposure to the virus (1). In the US, Medicare facilitated the telehealth response to the pandemic by temporarily providing coverage and payment of virtual services (2,3). As the pandemic subsides, there is a bipartisan push for legislation to make permanent the temporary waived restrictions on telehealth use (4).
Telehealth is the provision of health care services to patients from providers who are not at the same location; for hospice and palliative care, that means remotely delivering comfort care focused on improving quality of life. With about 1.55 million terminally ill Medicare beneficiaries receiving hospice care annually (5) and millions more seriously ill Americans eligible for palliative care (6), ensuring telehealth care is delivered in a high-quality and equitable way to hospice and palliative care patients is critical. Thus far, it is unclear what the impact of the expanded telehealth service delivery has had on the seriously ill population. Before making telehealth procedures and regulations more permanent in this area, it is imperative to have a deeper understanding of this form of service delivery and the ramifications for its recipients.
To better understand the informal caregiver’s experience with telehealth, we present quantitative and qualitative data collected from a national survey we conducted on informal caregivers’ perception of their sick patient’s experience using telehealth, many of whom used it for hospice and palliative care. To better understand the hospice leader’s perspective, we present the qualitative results from interviews with hospice leaders nationwide about their experience using telehealth during the pandemic. Finally, we discuss our mixed methods findings in terms of public policy implications and put forth challenges to and opportunities for telehealth increasing access and quality in hospice and palliative care. We present the following article in accordance with the Journal Article Reporting Standards (JARS) Mixed Methods Article Reporting Standards checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-21-3899/rc) (7).
Methods
We used a mixed methods sequential explanatory design to better answer our research question about the impact of telehealth service delivery on the seriously ill population by obtaining telehealth utilization and satisfaction information (quantitative and qualitative data) from caregivers and perspectives (qualitative data) from hospice leaders.
Informal caregiver survey
In March 2021, we conducted a cross-sectional survey of a sample of 595 individuals across the United States. The respondent characteristics are provided in Table 1. We used the Qualtrics survey platform, which uses multiple panels to recruit survey respondents and collect responses. Qualtrics made the survey available to their survey respondent base of whom those who identified themselves as informal caregivers of seriously ill patients across the US whose patients used telehealth during the prior five years could respond. Given the process in which Qualtrics curated respondents, a traditional response rate is not reported. Respondents were compensated in accordance with their individual agreements with Qualtrics. Several methods helped ensure quality data, including a unique digital fingerprinting technology and verifying that the open-ended responses did not contradict the Likert scale responses.
Table 1
| Characteristic | No. (%) | |
|---|---|---|
| Total (n=595) | Hospice only (n=228) | |
| Race | ||
| Patients | ||
| White | 442 (74.0) | 166 (73.0) |
| Black or African American | 120 (20.0) | 54 (24.0) |
| Asian | 22 (4.0) | 6 (3.0) |
| American Indian or Alaska Native | 8 (1.5) | 0 (–) |
| Native Hawaiian or Other Pacific Islander | 3 (0.5) | 2 (1.0) |
| Caregivers | ||
| White | 442 (74.0) | 166 (73.0) |
| Black or African American | 119 (20.0) | 53 (23.0) |
| Asian | 23 (4.0) | 7 (3.0) |
| American Indian or Alaska Native | 8 (1.5) | 0 (–) |
| Native Hawaiian or Other Pacific Islander | 3 (0.5) | 2 (1.0) |
| Gender | ||
| Patients | ||
| Female | 342 (57.0) | 132 (58.0) |
| Male | 247 (42.0) | 92 (40.0) |
| Other | 6 (1.0) | 4 (2.0) |
| Caregivers | ||
| Female | 303 (50.9) | 100 (44.0) |
| Male | 289 (48.6) | 128 (56.0) |
| Other | 3 (0.5) | 0 (–) |
| Patient metropolitan status† | ||
| Rural | 84 (14.0) | 25 (11.0) |
| Urban | 511 (86.0) | 203 (89.0) |
| Over 65 years old | ||
| Patients | 272 (46.0) | 93 (41.0) |
| Caregivers | 70 (12.0) | 13 (6.0) |
| Telehealth timing‡ | ||
| Pre-COVID | 219 (37.0) | 126 (55.0) |
| During COVID | 346 (58.0) | 90 (39.0) |
| Indeterminate | 30 (5.0) | 12 (5.0) |
†, metropolitan status as determined by Rural Urban Commuting Area (RUCA) classification system. ‡, determined by caregiving end year: 2019 or prior = Pre-COVID; 2021 = During COVID; 2020 = Indeterminate.
The survey utilized questions from two previously published and validated surveys, the Centers for Medicare & Medicaid Services’ (CMS) CAHPS® Hospice Survey (8) and the Telehealth Usability Questionnaire (9). Demographic questions were based on the CAHPS Hospice Survey and telehealth questions were based on the Telehealth Usability Questionnaire. The survey consisted of 41 items with the majority utilizing a Likert scale from 1 (disagree) to 7 (agree) on questions pertaining to telehealth usability, seriously ill patients’ satisfaction with telehealth as perceived by their caregiver, and caregivers’ satisfaction with telehealth. Three open-ended items asked respondents to expand on their responses within these categories. The remaining questions were related to the demographic information about both the patient and caregiver and descriptive information about their telehealth use. The full survey can be found in a supplementary appendix online (available online: https://cdn.amegroups.cn/static/public/10.21037apm-21-3899-1.pdf).
Statistical analysis
We used a multiple linear regression model (10) to assess all associations between the dependent variables and independent variables for the entire sample and for the sample subset who indicated the patient received hospice or palliative care. The dependent variables were grouped by question sets about telehealth usability (question numbers 7–10), seriously ill patients’ satisfaction with telehealth as perceived by their caregiver (question numbers 14–20), and caregivers’ satisfaction with telehealth (question numbers 21–24). The independent variables included telehealth timing regarding COVID (prior, during, or unknown), percent of telehealth experiences that included video, being aged 65 or older, metropolitan status (urban or rural), race (White or Non-White), and electronic accessibility. For the rural or urban dichotomous classification, we used criteria based on the Rural Urban Commuting Area (RUCA) classification system (11). Electronic accessibility was assessed using a group of three questions that asked about access to necessary equipment, access to an internet connection, and having good quality internet access. Additionally, we checked for multicollinearity using variance inflation factor (12). All statistical tests were two-sided with a P value less than or equal to 0.05 indicating a statistically significant effect. All models were fit using statistical software SPSS, version 26.
Hospice leader interviews
Between May and July of 2021, we conducted 25 semi-structured telephone interviews with hospice leaders across the US about telehealth for hospice care. We identified potential hospice leaders for participation from the researchers’ hospice contacts, National Hospice Locator (12) and state hospice organizations. We recruited participants by sending 712 email invitations to hospice leaders asking them if we could interview them or a member of their professional team ‘to learn more about the quality of telehealth services, implications of telehealth for traditionally underserved groups, and policies and programs that may facilitate better care’. Our survey results informed our interview focus areas. The interview questions were open-ended and asked about the three main topics included in the study invitation to hospice leaders mentioned previously. These open-ended questions related to the major concerns and benefits reported in the caregiver survey. Interested individuals were sent an informed consent email. The informed consent included that their names and organizations would not be individually identified in any reports resulting from the project. There were no payments or incentives provided to the interviewees.
The interviews were divided between three researchers (MK, MCH, and EV), held for 7 to 39 minutes with an average of 19 minutes in length, recorded and transcribed, and conducted until the researchers believed they reached saturation. The same three researchers read all the transcripts and iteratively developed a coding structure after examining and discussing the data. We used a codebook thematic analysis approach to examine the data (13). The qualitative data analysis tool Dedoose V.8.0.35 (SocioCultural Research Consultants, www.dedoose.com) was used to code and categorize interview responses by the three researchers who collectively identified themes based on codes and reviewing transcripts. The research team reviewed the codes and themes through a series of discussions before the final themes were chosen (14,15). Additionally, throughout the process, the researchers reviewed the team’s interview notes to ensure that themes accurately reflected the actual interview content.
Ethics statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional review boards of Seattle University and Northern Illinois University (No. HS21-0421) and informed consent was taken from all individual participants.
Results
Informal caregiver survey
We obtained 618 completed surveys. Of those, we discarded 23 surveys due to low quality (e.g., straightlining, unrealistic completion time, gibberish responses), resulting in a final sample size of 595 respondents.
The Cronbach’s alpha (12) for each of the dependent and independent variable question groups were 0.85 or higher, indicating good internal consistency. For perceived patients’ satisfaction, 51.4% of the variability was explained by the independent variables. Having higher video usage, the patient being younger than 65, and having better electronic accessibility were statistically significant risk factors that increased perceived patient satisfaction. A one unit increase in better electronic accessibility was associated with a 0.676 (SE =0.030, P<0.001) increase in perceived patients’ satisfaction with telehealth (both variables measured using a 1–7 Likert scale), on average, after controlling for other independent variables. For caregivers’ satisfaction with telehealth, only 25.2% of the variability was explained by the regression model. Telehealth taking place prior to COVID, having higher video usage, the caregiver being younger than 65, and better electronic accessibility were statistically significant factors in greater caregiver satisfaction. Caregivers’ satisfaction with telehealth during the pandemic was, on average, 0.34 (on a scale of 1 to 7) less than caregivers’ satisfaction with telehealth prior to the pandemic, after controlling for other independent variables. In all regressions, no evidence for multicollinearity was found since all variance inflation factor values are close to 1. The regression results for the entire sample are presented in Table 2.
Table 2
| Variable | Telehealth usability (R-squared =0.437) | Perceived patients’ satisfaction (R-squared =0.514) | Caregivers’ satisfaction (R-squared =0.252) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | SE | P value | Estimate | SE | P value | Estimate | SE | P value | |||
| Intercept | 1.642 | 0.227 | 0.000 | 1.247 | 0.212 | 0.000 | 2.232 | 0.301 | 0.000 | ||
| COVID (during) | 0.003 | 0.087 | 0.970 | 0.077 | 0.081 | 0.340 | −0.344 | 0.115 | 0.003 | ||
| COVID (unknown) | 0.059 | 0.194 | 0.761 | 0.022 | 0.181 | 0.903 | −0.124 | 0.259 | 0.631 | ||
| Video usage | 0.311 | 0.132 | 0.019 | 0.377 | 0.124 | 0.002 | 0.608 | 0.176 | 0.001 | ||
| Aged 65 or older† | −0.058 | 0.082 | 0.480 | −0.249 | 0.076 | 0.001 | −0.294 | 0.109 | 0.007 | ||
| Urban | −0.066 | 0.118 | 0.577 | 0.014 | 0.110 | 0.902 | 0.007 | 0.156 | 0.962 | ||
| White | −0.016 | 0.093 | 0.862 | 0.019 | 0.087 | 0.825 | −0.079 | 0.123 | 0.524 | ||
| Electronic accessibility | 0.635 | 0.032 | 0.000 | 0.676 | 0.030 | 0.000 | 0.515 | 0.043 | 0.000 | ||
†, the variable “Aged 65 or older” is referring to the patient’s age for the categories “telehealth usability” and “perceived patients’ satisfaction” and referring to the caregiver’s age for the category “caregivers’ satisfaction”.
The sample subset who answered yes to whether their patient received hospice or palliative care (n=228) closely mirrored the descriptive statistics of the entire sample in terms of age of patient and caregiver, race, gender, urban setting, and care during the COVID period. The regression results for this sample subset were also very similar to the entire sample, except that some significant independent variables in the larger sample become insignificant in the subset due to the sample size reduction. The regression results for the subset are presented in Table 3.
Table 3
| Variable | Telehealth usability (R-squared =0.490) | Perceived patients’ satisfaction (R-squared =0.535) | Caregivers’ satisfaction (R-squared =0.298) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | SE | P value | Estimate | SE | P value | Estimate | SE | P value | |||
| Intercept | 1.487 | 0.368 | 0.000 | 1.054 | 0.369 | 0.005 | 2.099 | 0.478 | 0.000 | ||
| COVID (during) | 0.034 | 0.137 | 0.806 | 0.070 | 0.138 | 0.612 | −0.133 | 0.179 | 0.456 | ||
| COVID (unknown) | 0.144 | 0.306 | 0.638 | 0.118 | 0.309 | 0.702 | −0.280 | 0.400 | 0.485 | ||
| Video usage | 0.301 | 0.237 | 0.205 | 0.830 | 0.239 | 0.001 | 0.799 | 0.308 | 0.010 | ||
| Aged 65 or older‡ | −0.027 | 0.134 | 0.840 | −0.422 | 0.136 | 0.002 | −0.314 | 0.175 | 0.075 | ||
| Urban | −0.072 | 0.214 | 0.736 | 0.133 | 0.211 | 0.531 | 0.105 | 0.274 | 0.702 | ||
| White | 0.018 | 0.145 | 0.903 | 0.005 | 0.146 | 0.973 | −0.061 | 0.190 | 0.748 | ||
| Electronic accessibility | 0.671 | 0.051 | 0.000 | 0.658 | 0.052 | 0.000 | 0.515 | 0.067 | 0.000 | ||
†, author’s analysis of survey sample where respondents answered yes to whether their patient used hospice or palliative care (n=228); ‡, the variable “Aged 65 or older” is referring to the patient’s age for the categories “telehealth usability” and “perceived patients’ satisfaction” and referring to the caregiver’s age for the category “caregivers’ satisfaction”.
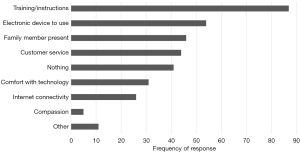
To showcase representative data from the surveys, Table 4 presents survey responses to selected items about the experience using telehealth. Responses to our open-ended question asking what helped the patient and family use telehealth is shown in Figure 1. Over one-fourth of the 341 respondents who answered this question indicated that having training or instructions helped, with 28% of them specifically mentioning “in-person” training or instructions. Other top responses included having an electronic device to use, a family member present, and customer service.
Table 4
| Item | Disagree  Agree Agree |
Not applicable | Average score [1–7] | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |||
| General telehealth usability | |||||||||
| Telehealth improves/improved my family member’s access to services | 21 | 13 | 34 | 81 | 134 | 134 | 159 | 19 | 5.31 |
| It is/was simple to use telehealth | 7 | 13 | 30 | 79 | 132 | 149 | 176 | 9 | 5.50 |
| Seriously ill patients’ satisfaction with telehealth as perceived by their caregiver | |||||||||
| My family member can/could use telehealth without my or another caregiver’s assistance | 72 | 35 | 43 | 85 | 102 | 97 | 149 | 12 | 4.71 |
| My family member likes/liked using telehealth | 33 | 32 | 57 | 67 | 114 | 138 | 140 | 14 | 5.01 |
| Caregivers’ satisfaction with telehealth | |||||||||
| I receive(d) support for my religious and spiritual beliefs using telehealth | 50 | 28 | 43 | 53 | 77 | 75 | 94 | 175 | 4.62 |
| Overall I am satisfied with telehealth | 21 | 25 | 26 | 57 | 111 | 165 | 189 | 1 | 5.46 |
Hospice leader interviews
The interview respondents represented all the major regions of the US. Table 5 shows the characteristics of the respondents.
Table 5
| Characteristic | No. [%] |
|---|---|
| Size (patients/day) | |
| Small [0–49] | 4 [16] |
| Medium [50–124] | 8 [32] |
| Large [125–199] | 4 [16] |
| Extra large [200+] | 9 [36] |
| Ownership | |
| For-profit | 15 [60] |
| Nonprofit | 10 [40] |
| Metropolitan statusa | |
| Rural | 5 [20] |
| Urban | 20 [80] |
| Region | |
| Midwest | 4 [16] |
| Northeast | 1 [4] |
| South | 13 [52] |
| West | 7 [28] |
| Roleb | |
| Chief executive officer | 9 [36] |
| Other chief-level | 4 [16] |
| Director/manager | 8 [32] |
| Clinician | 4 [16] |
a, metropolitan status as determined by each hospices profile on National Hospice Locator (12); b, characteristic of the respondent, not of the hospice.
Quality of telehealth depends on the function
While there was a consensus across hospice leaders that telehealth could not replace all aspects of care, there were certain functional areas where telehealth was consistently noted as enhancing usual care. This was the case for access to monitoring and support activities such as addressing standard patient and family concerns, explaining lab results, and basic diagnostic activities. These representative quotes describe how telehealth positively supplemented usual care:
Telehealth has shortened wait times tremendously. Usually in person was only available Tuesday or Thursday whereas, with telehealth, a nurse was accessible almost immediately at most times.
We have started going into homes again more often but continue to use telehealth to get more patients in. The access and quickness of care that telehealth has brought us has been amazing.
It was great for sending diagnostic pictures such as sending pictures of rashes.
Bereavement support was another functional area where multiple interviewees explicitly mentioned having positive telehealth experiences, especially when quality video use was implemented. As one leader noted:
It showed us that you can virtually provide support as well, and especially to ameliorate those feelings of isolation and loneliness.
The respondents consistently praised telehealth for enhancing connections with out-of-town family members. One leader described it this way:
We are going to continue to do this. The nurses all carry laptops now so they can hook right up and do that sort of thing for the families. We’ve gotten a lot of positive responses from that, especially from folks serving in the military overseas or for whatever reason cannot get there.
One area where there were mixed opinions in terms of telehealth effectiveness pertained to the roles of social workers and spiritual counselors. A few hospice leaders noted that the time these individuals could save from commuting less would manifest in reaching more individuals. Others highlighted the benefit of fewer people entering a patient’s home. That said, some respondents noted that these particular areas of hospice care were difficult to do well without an in-person connection. Quotes from two hospice leaders show varying opinions about using telehealth for social work and spiritual counseling:
With a small program, you have one social worker covering a huge area and, you know, they are spending hours in the car driving to see patients and now they can see those patients through telehealth much more often and more frequently.
But I think what hospice patients really missed out on is the team aspect from the social worker and spiritual counselor. It’s just not the same when you’re talking to somebody over a phone. And that’s the true distinction with hospice is that we’re interdisciplinary. So I feel like they really missed out on those relationships and that the level of support is not there when it is not face to face.
Confusion and concern for abuse
Hospice leaders expressed some confusion about policies during the pandemic, namely about requirements for recertification, regulations as to what constituted a telehealth visit, what activities were HIPPA compliant, and where to find training about the protocols. As one hospice stated:
We have our target way of serving our customer and there was some hesitation or unknown when the decision came to go because there were no clear guidelines from the CMS at that time.
Telehealth implementation, use of technology, and the way care was provided during the COVID-19 pandemic differed among hospices. Some hospices shared that they continued to see patients face-to-face, while others transitioned completely to telehealth with most patients. Several hospices shared that they were unprepared for this new form of service delivery because they were unaccustomed to providing care in this manner:
[Telehealth] was used very little prior to the pandemic and many hospices weren't even set up with the technology to be able to use telehealth, and they didn't have policies, they didn't have procedures, they didn't have equipment, they didn’t have the staff training in place.
Many hospices expressed concern for telehealth allowing for potential system abuse by hospice and informal caregivers. Respondents said that, although there are benefits of incorporating telehealth into hospice practice, there is fear that organizations may try to cut corners:
There’s great potential for abuse for hospices to just do some telephone calls and not even really make it audio visual telehealth visit and bill for services and provide very shoddy care.
There was also concern that family drug diversion may become more prevalent if informal caregivers are given more control over medications. To prevent this, one hospice specifically mentioned that they must physically go to homes to set out medications for the patient and perform weekly drug counts. Most hospice executives agreed that quality measures and regulations need to be standardized regarding telehealth practice to eliminate existing confusion and potential abuse.
Innovation and cautious optimism going forward
Nearly half of the hospices plan on continuing telehealth as an additional form of service delivery beyond the pandemic. One respondent described how a large hospital system had recently started selling medical equipment to homebound patients to use during telehealth visits. This respondent connected this example to what they saw as an industry trend:
There’s really a new wave of tools and technology being planned and implemented to help really change the future of how we deliver medicine.
Despite the hope offered by some for new innovations and telehealth enhancing care, there was a cautious tone prevalent across respondents. One concern centered around the lack of overall context when telehealth is the only form of service delivery:
I think there’s just a huge social infrastructure gap…we see the biggest need for care to be in-person, at least early on. You’ve got to understand the patient’s housing situation, the social dynamic. Are there food insecurity issues? Do they have utility insecurity issues?...
Most respondents stressed the important influence CMS has in the future of telehealth for hospice patients. One respondent expressed concern over CMS scaling back reimbursement for telehealth:
The way CMS can really negatively affect the continued utilization, I think, is to overregulate it or pull back some of the payment funding…to me we should be investing in this technology. We should be supporting it.
Discussion
To the best of our knowledge, this study is the first to evaluate telehealth for hospice and palliative care from the perspective of informal caregivers and hospice leaders. We found that access to the internet and electronic devices, telehealth training, and video use capabilities are critical aspects of quality telehealth care. While concern for abuse and telehealth replacing essential in-person care exists, the general outlook from hospice industry leaders about the potential of telehealth improving access and supplementing in-person hospice and palliative care services is positive and hopeful.
Offering telehealth is just the first step in providing virtual services. As seen in this study, patients being able to access and correctly use an electronic device is critical to effective telehealth. One strategy for helping to ensure that patients can effectively use telehealth is to have an administrative staff person conduct a mock visit with the patient a day or two before the first telehealth visit with the provider (16,17). This step can be especially helpful for older patients who often do not have as much experience as their younger counterparts in using electronic devices and applications. Another strategy is for community health workers to meet in advance with the patient at their home to help them set up the application, provide training, and conduct test video visits (17). The latter option helps address the strong desire for “in-person instructions” seen in our caregiver survey responses.
Training alone will not enable telehealth capabilities for all hospice and palliative care patients and their families. Electronic devices and internet connectivity are components found herein and by other researchers as essential to conducting telehealth (18,19). The rise in telehealth during the COVID-19 pandemic has highlighted the gulf between those who have access to devices and the internet and those who do not. This “digital divide” is being called the newest social determinant of health (20-22). Unfortunately, traditionally underserved groups such as individuals from racial and ethnic minority groups and rural residents are more likely to be on the access-lacking side of the digital divide (20). Programs to improve internet access and affordability, such as the United States Department of Agriculture’s ReConnect Loan and Grant Program (23) are often highlighted as crucial to helping close US education and economic gaps. Such electronic connectivity programs could also be instrumental in helping telehealth improve health disparities.
Telehealth implementation within hospice and palliative care must be mindful of the disparities (e.g., racial/ethnic, rural, income) that exist, not only in technology access but in health care, in general (24,25), and aim to address them intentionally. One item to consider is that findings suggest lower-income patients and families often benefit from social services stemming from in-person hospice care (26). Originally rooted in the idea of providing “hospitality” (27), hospice helps patients and families feel comfortable and rest. This may sometimes involve hospice and palliative care workers addressing broader social needs such as poor living conditions or family food shortages to improve quality of life (28). Without in-person visits, it may be difficult to assess social needs beyond traditional health-focused areas like pain management, but viewing a patient’s environment and intervening can significantly improve the overall quality of life. A potential solution that would help enable this holistic approach is offering hybrid care where telehealth may be a part of care but not the sole mode of service delivery for a patient. Offering telehealth as a supplement to traditional in-person care is consistent with the interview responses in this study. If equipment and connectivity are sound and pressing needs are assessed and addressed during in-person visits, then telehealth could more effectively augment care by providing increased access to patients within their own homes. Our survey results found no significant differences in patient or caregiver telehealth satisfaction levels across race suggesting that this type of care has the potential to reduce the racial disparities experienced within palliative care (29,30). By focusing on electronic access and social determinants of health upfront, providers can help ensure that telehealth serves to help reduce existing disparities in access and quality care.
An ethos of hospice is showing compassion. Providing compassion as well as good customer service emerged as important telehealth components in the surveys and interviews. Although telehealth allowed hospices to reach more people, a few hospice leaders expressed concern over providing quality social work and spiritual counseling services through telehealth. In addition, our survey results suggested that caregivers were less satisfied with spiritual support delivered using telehealth compared to their satisfaction with other hospice services delivered using telehealth. We recommend that providers focus on these patient-centered elements when developing and delivering services via telehealth. The Academy of Communication in Healthcare provides free resources for helping to deliver person-centered telehealth, including tips to better connect with patients and guidance to develop relationship-centered communication skills (31).
Hospice industry leaders found the temporary telehealth regulations enacted during the pandemic confusing. Industry organizations such as the American Medical Association and the National Hospice and Palliative Care Organization provided clarification and tutorials on their websites to help providers navigate the changing landscape amidst the crisis (32,33). While this guidance may have been helpful as a response, relying on such tutorials isn’t sufficient as more permanent telehealth regulations are put in place. Keeping in mind that providers must consider various policies at the national, state, and private insurance level, policymakers should encourage consistency across payers and provide clear communication about regulations and payment for telehealth.
Looking forward, the hospice leaders in our study expressed concern that reduced telehealth restrictions will allow for system abuse by providers. While telehealth may present new opportunities for fraudulent activities such as over-treating or under-treating patients and improper billing for virtual care, the US Department of Health and Human Services is aware of these risks and has already conducted significant oversight work regarding telehealth and charged guilty parties (34). Similar heavy supervision by the government as well as private payers, health care companies, and industry associations must accompany the shift to telehealth. While almost all policies have the potential to be taken advantage of, understanding where the potential issues exist and implementing appropriate monitoring can help in holding parties accountable during telehealth use.
Along with concern among hospice leaders came a sense of hope that telehealth could improve care and access for patients and families. Vendors and health systems offering connected health devices (e.g., wearable heart monitors and at-home stethoscopes) to use at the advice of the telehealth provider are proliferating across the healthcare industry, including for hospice and palliative care. Such home instruments are especially useful for patients living in remote areas where providers can monitor them in some way from afar and assist during emergencies when a nurse or physician may have to drive hours before arriving in person. Hitherto, Medicare beneficiaries living in rural areas have been less likely to use hospice and palliative care services than their more urban counterparts (35). Care delivery using effective telehealth strategies could help close that gap.
The pandemic experience highlighted that telehealth can effectively work for certain hospice services, as indicated herein. Our study also shows that telehealth is particularly useful in locations with limited hospice resources. Given the US projected shortages for social workers and physicians in the near future (36,37) and the projected increase in the older adult population (38) and Americans with chronic disease (39), telehealth may become important across even more regions in the US that have increasingly limited access to care. In addition, the survey results reporting relatively high telehealth satisfaction levels for caregivers who used telehealth pre-pandemic suggests that there is a place for telehealth for hospice and palliative care in a post-pandemic world. The challenge now is for states and the federal government to continue telehealth’s best practices and help the industry overcome the challenges (e.g., internet access) to sustain increased access in the future. When implemented in a sound, thoughtful manner with the patient largely in mind, telehealth has the potential to improve end-of-life quality while reducing the health disparities experienced during this time.
Strengths and limitations
This study provides access to multiple stakeholder perspectives about the experiences of telehealth for palliative care. Another strength is that the participants from across the United States were included in the study, allowing for representation across regions of the country. Lastly, by collecting usage date data, we were able to compare responses about telehealth before the pandemic to telehealth during the pandemic.
Our mixed-methods analysis of surveys and interviews relied on the perceptions of informal caregivers and hospice leaders. While the patient’s perceptions would have been helpful, obtaining such data is difficult for a seriously ill, many of whom are dying, population. For this reason, CMS relies on a national survey of family or friends to collect its Consumer Assessment of Healthcare Providers and Systems CAHPS® Hospice Survey data (8).
Sequential explanatory design studies typically use quantitative findings to inform the interviews conducted within the same population. In this instance, researchers chose to interview hospice leaders in-depth instead of the surveyed caregivers. The researchers determined that the hospice leaders’ unique perspective of observing care with and without telehealth combined with the caregivers’ surveyed experiences provided the most holistic overview of this type of care.
Non-response bias is a possible limitation of this study. People less interested in telehealth may have been less likely to complete the survey or agree to be interviewed. Furthermore, individuals most affected by COVID (e.g., overwhelmed) may have been less inclined to respond due to limited time or energy. Given our exploratory focus on learning about challenges, policies, and practices, having an interested participant group seems appropriate. Nonetheless, the study data should not be used to determine more quantitative measures such as telehealth uptake.
Some of our survey respondents may have been caring for patients who were receiving curative treatments. We surveyed caregivers of seriously ill patients for recruiting purposes to obtain a large enough sample for analysis. However, we were encouraged by finding significant concordance between the large subset who explicitly indicated that their patients received palliative care or hospice care and the sample of seriously ill patients overall. Another limitation is the possibility that patients who received palliative care or hospice care may have received telehealth before they started receiving palliative care or hospice care.
Conclusions
Telehealth has experienced widespread implementation across the health care system since the start of COVID-19. As legislators and industry leaders look to continue some form of telehealth beyond the pandemic, special attention must be paid to the hospice and palliative care industry and data related to patient and family experience and overall effectiveness of using telehealth in this setting. Our study presents novel survey and interview data that show concerns and priorities when implementing telehealth. With quality of life of paramount importance when considering the final weeks and days of one’s life, perspectives of those closest to the care experience offer insights that traditional health outcome measures cannot fully tap. As CMS determines its rules and regulations regarding telehealth, addressing telehealth’s shortcomings and risks upfront will help virtual care realize its potential of increasing access, lowering costs, and improving care effectiveness for patients, including those facing serious illness and imminent death.
Acknowledgments
The authors thank Allison Hainstock for her assistance in this research and Beverly Henry and Yujun Liu for their helpful suggestions. The authors also thank the caregiver survey respondents and hospice leader interviewees who took the time to provide their perspectives on this topic. Part of this study was presented at the 2022 Annual Assembly of Hospice and Palliative Care.
Funding: This work was supported by the Borchard Foundation Center for Law & Aging (to MCH, EV, & MK).
Footnote
Reporting Checklist: The authors have completed the Journal Article Reporting Standards (JARS) Mixed Methods Article Reporting Standards checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-21-3899/rc
Data Sharing Statement: Available at https://apm.amegroups.com/article/view/10.21037/apm-21-3899/dss
Peer Review File: Available at https://apm.amegroups.com/article/view/10.21037/apm-21-3899/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-21-3899/coif). MCH reports that the Borchard Foundation Center for Law & Aging provided funding for salary support for her and data collection. EV reports that the Borchard Foundation Center for Law & Aging provided funding for data collection. MK reports that the Borchard Foundation Center for Law & Aging provided funding for stipend support for her and data collection. HZ has no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional review boards of Seattle University and Northern Illinois University (No. HS21-0421) and informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yamey G, Pai M. How covid-19 is revolutionizing health care around the world. Time USA [Internet]. 2021 Jun 3 [cited 2021 Aug 12];Ideas:[about 2 p.]. Available online: https://time.com/6052677/covid-19-health-care-innovations/
- Verma S. Early impact of CMS expansion of Medicare telehealth during COVID-19. 2020 Jul 15 [cited 2021 Jul 28]. In: Health Affairs Blog [Internet]. Bethesda (MD): Health Affairs. C2020-. [About 3 screens]. Available online: https://www.healthaffairs.org/do/10.1377/hblog20200715.454789/full/
- Centers for Medicare & Medicaid Services. Medicare telemedicine health care provider fact sheet [Internet]. Baltimore (MD): CMS; 2020 Mar 17 [cited 2021 July 27]. Available online: https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet
- Jercich K. Senators introduce bipartisan bill aimed at safeguarding rural telehealth access [Internet]. Portland (ME): HealthcareITNews; 2020 June 15 [cited 2021 July 27]. Available online: https://www.healthcareitnews.com/news/senators-introduce-bipartisan-bill-aimed-safeguarding-rural-telehealth-access
- National Hospice and Palliative Care Organization. 2020 edition: hospice facts and figures [Internet]. Alexandria (VA): National Hospice and Palliative Care Organization; 2020 Aug 20 [cited 2021 Jul 27]. 26 p. Available online: https://www.nhpco.org/factsfigures/
- Center to Advance Palliative Care. America’s care of serious illness: A state-by-state report card on access to palliative care in our nation’s hospitals. Center to Advance Palliative Care and the National Palliative Care Research Center; 2019 Sep. Available online: https://reportcard.capc.org
- American Psychological Association [Internet]. Washington D.C.: c2020 [cited 2022 Feb 5]. Available online: https://apastyle.apa.org/jars/mixed-table-1.pdf
- Centers for Medicare & Medicaid Services. CAHPS Hospice Survey [Internet]. Baltimore (MD): CMS; c2020 [cited 2021 July 27]. Available online: https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/CAHPS/CAHPS-Hospice-Survey
- Parmanto B, Lewis AN, Graham KM, et al. Development of the telehealth usability questionnaire (TUQ). Int J Telerehabil 2016;8:3-10. [Crossref] [PubMed]
- Kutner MH, Nachtsheim CJ, Neter J. Applied linear regression models. 5th ed. New York: McGraw-Hill Irwin, 2005:406-410.
- National Hospice Locator [Internet]. Colorado Springs (CO): Hospice Analytics. c2021 - [cited 2021 Aug 3]. Available online: http://www.nationalhospiceanalytics.com
- Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika 1951;16:297-334. [Crossref]
- Braun V, Clarke V. Conceptual and design thinking for thematic analysis. Qualitative Psychology 2021 May 13. Available online:
10.1037/qup0000196 10.1037/qup0000196 - Charmaz K. Constructing grounded theory: A practical guide through qualitative analysis. Sage 2006;
- Glaser BG, Strauss AL. The discovery of grounded theory: Strategies for qualitative research. Routledge; 2017 Jul 5.
- Health Resources & Services Administration. Getting patients set up with telehealth technology [Internet]. Rockville (MD): Telehealth.HHS.gov; c2020 [updated 2021 Jan 13; cited 2021 Jul 27]. Available online: https://telehealth.hhs.gov/providers/preparing-patients-for-telehealth/getting-patients-set-up-with-new-technology/
- Ikram U, Gallani S, Figueroa JF, et al. 4 strategies to make telehealth work for elderly patients. Harv Bus Rev 2020. Available online: https://hbr.org/2020/11/4-strategies-to-make-telehealth-work-for-elderly-patients
- Velasquez D. Ensuring the growth of telehealth during covid-19 does not exacerbate disparities in care [Internet]. 2020 May 8 [cited 2021 Jul 27]. In: Health Affairs Blog [Internet]. Bethesda (MD): Health Affairs Blog. c2020-.[about 2 screens]. Available online: https://www-healthaffairs-org.auth.lib.niu.edu/do/10.1377/hblog20200505.591306/full/
- Sieck CJ, Sheon A, Ancker JS, et al. Digital inclusion as a social determinant of health. NPJ Digit Med 2021;4:52. [Crossref] [PubMed]
- Early J, Hernandez A. Digital Disenfranchisement and COVID-19: Broadband Internet Access as a Social Determinant of Health. Health Promot Pract 2021;22:605-10. [Crossref] [PubMed]
- Clare CA. Telehealth and the digital divide as a social determinant of health during the COVID-19 pandemic. Netw Model Anal Health Inform Bioinform 2021;10:26. [Crossref] [PubMed]
- Pew Research Center. Internet/broadband fact sheet [Internet]. Washington (DC): The Pew Charitable Trusts; 2021 Apr 7 [cited 2021 Jul 27]. Available online: https://www.pewresearch.org/internet/fact-sheet/internet-broadband/?menuItem=89fe9877-d6d0-42c5-bca0-8e6034e300aa
- U.S. Department of Agriculture. Program Overview [Internet]. USDA; 2021[cited 2021 Jul 27]. Available online: https://www.usda.gov/reconnect/program-overview
- Phelan JC, Link BG. Is racism a fundamental cause of inequalities in health? Annu Rev Sociol 2015;41:311-30. [Crossref]
- Loccoh E, Joynt Maddox KE, Xu J, et al. Rural-Urban Disparities In All-Cause Mortality Among Low-Income Medicare Beneficiaries, 2004-17. Health Aff (Millwood) 2021;40:289-96. [Crossref] [PubMed]
- Carlson MD, Morrison RS, Holford TR, et al. Hospice care: what services do patients and their families receive? Health Serv Res 2007;42:1672-1690. [Internet]. [Crossref] [PubMed]
- Marshall K, Hale D. Understanding hospice. Home Healthc Now 2017;35:396-7. [Crossref] [PubMed]
- Hughes MC, Vernon E, Kowalczyk M, et al. US hospices' approach to racial/ethnic minority inclusion: a qualitative study. BMJ Support Palliat Care 2021; Epub ahead of print. [Crossref] [PubMed]
- Johnson KS. Racial and ethnic disparities in palliative care. J Palliat Med 2013;16:1329-34. [Crossref] [PubMed]
- Hughes MC, Vernon E. Closing the gap in hospice utilization for the minority Medicare population. Gerontol Geriatr Med 2019;5:2333721419855667. [Crossref] [PubMed]
- Academy of Communication in Healthcare. Covid-19: telehealth communication [Internet]. Lexington (KY): ACH; 2020 [cited 2021 July 27]. Available online: https://www.achonline.org/COVID-19/Telemedicine
- American Medical Association. Covid-19 state policy guidance on telemedicine [Internet]. Chicago: AMA; 2020 [cited 2021 July 27]. Available online: https://www.ama-assn.org/system/files/2020-04/covid-19-state-policy-guidance-on-telemedicine.pdf
- National Hospice and Palliative Care Organization. Emergency preparedness: covid-19 information [Internet]. Alexandria (VA): NHPCO; [cited 2021 Jul 27]. Available online: https://www.nhpco.org/coronavirus/
- United States Department of Justice. National health care fraud and opioid takedown results in charges against 345 defendants responsible for more than $6 billion in alleged fraud losses: largest health care fraud and opioid enforcement action in department of justice history [Internet]. Washington (DC): U.S. Department of Justice; 2020 Sep 30 [cited 2021 Jul 27]. Available online: https://www.justice.gov/opa/pr/national-health-care-fraud-and-opioid-takedown-results-charges-against-345-defendants
- MedPAC. Report to the congress: Medicare payment policy [Internet]. Washington, D.C.: MedPac; 2021 Mar. Chapter 11, Hospice services: Assessing payment adequacy and updating payments; p. 307-349. Available online: https://www.medpac.gov/wp-content/uploads/import_data/scrape_files/docs/default-source/reports/Mar11_Ch11.pdf
- Kirch DG, Petelle K. Addressing the Physician Shortage: The Peril of Ignoring Demography. JAMA 2017;317:1947-8. [Crossref] [PubMed]
- Lin VW, Lin J, Zhang X U.S.. Social Worker Workforce Report Card: Forecasting Nationwide Shortages. Soc Work 2016;61:7-15. [Crossref] [PubMed]
- United States Census Bureau. Older people projected to outnumber children for first time in U.S. history. 2018[cited 2021 Jul 30]. Available online: https://www.census.gov/newsroom/press-releases/2018/cb18-41-population-projections.html
- Centers for Disease Control and Prevention. Health and economic costs of chronic diseases [Internet]. 2021 [cited 2021 Jul 30]. Available online: https://www.cdc.gov/chronicdisease/about/costs/index.htm


