
Weekend effect on the mortality rate of in-hospital cardiopulmonary resuscitations from 2010 through 2019: a retrospective population-based cohort study
Introduction
In-hospital cardiopulmonary resuscitation (ICPR) is associated with worsening of clinical outcomes, including a lower survival rate (1). Although in-hospital cardiopulmonary arrest (IHCA) tends to be considered an irreversibly poor condition, recently outcomes have improved in the United States. This may be due to improvements in the system of cardiopulmonary resuscitation (CPR), education, and training for higher quality CPR, which can influence the clinical outcome of CPR (2).
This could also be explained by the fact that clinical outcomes after ICPR could be associated with a smaller number of medical staff and professionals, frequent changes in medical staff, lack of monitoring, delayed defibrillation, delayed procedures, and systematic errors. It could be related to the day or time, such as weekends or nights. The “weekend effect” on ICPR implies that the patients who undergo ICPR on the weekend would be associated with worse clinical outcomes after ICPR compared to those who undergo ICPR on weekdays (3-6). We previously analyzed 1195 in-hospital CPR cases and studied CPRs by day of the week, and observed that the occurrence of intra-hospital CPRs varied by Mondays-Wednesdays and Thursdays-Sundays, and that the return of spontaneous circulation (ROSC) rate of ICPRs occurring on Sundays was low even after correction (3). In a study using data from a multicenter or regional ICPR registry, patients who received ICPR on weekends/nights were associated with lower survival to discharge (5,7-9). However, no study on the weekend effect on long-term mortality was conducted from a national scale database in the Republic of Korea, including long-term survival, such as 6-month and 1-year mortality. Because overall improvement of the ICPR system is important for critical care medicine, the weekend effect on long-term survival outcomes up to 1-year after ICPR should be examined using a large population registered in a nationwide database.
Therefore, we aimed to examine the weekend effect on 6-month and 1-year mortality after ICPR using data from the National Health Insurance Service database in the Republic of Korea in 2010–2019, and to evaluate the risk factors that worsen 1-year survival. We present the following article in accordance with the STROBE reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-22-266/rc) (10).
Methods
Study design, setting, and ethical statement
This retrospective population-based cohort study was approved by the institutional review board (IRB) of Seoul National University Bundang Hospital (No. X-2011-651-901), and individual consent for this retrospective analysis was waived, because the data used in this study were anonymized. Permission for data use of the National Health Insurance Service (NHIS) database was obtained after approval of the study protocol (No. NHIS-2021-1-266). The study also conformed to the provisions of the Declaration of Helsinki (as revised in 2013).
Data source: NHIS database
We used a South Korean national registration database that contains information on the diagnosis of diseases and prescription of any procedures and/or drugs. For financial support from the NHIS, which is the only public insurance system in South Korea, all diagnoses of diseases and information on prescription for any procedures and/or drugs should be registered in the NHIS database by physicians. The International Diseases and Related Health Issues 10th edition (ICD-10) codes were used for disease diagnosis (Table S1).
Study population
We conducted a retrospective review of all adult patients who underwent ICPR from January 1, 2010, through December 31, 2019. If a patient received more than one instance of CPR in a row, all ICPR events during the day were considered as one ICPR event. Only the first ICPR event was included in this study if the patient had experienced ICPR events more than once on different days during the study period. For example, if a patient received ICPR two times on 12 March 2010 and 16 March 2010, only the first ICPR event on 12 March 2010 was included in the study, while the ICPR event on 16 March 2010 was excluded. These exclusion criteria enable our study population to be homogeneous because physical condition of patients may be worse at a later ICPR event compared to that at an earlier ICPR event. Pediatric patients whose age were <18 years old were excluded in this study, because the etiology and prognosis of ICPR in pediatric patients differs from those of adult patients.
Exposure variable (ICPR on weekends)
The study population was divided into two groups according to the day of the week on which the ICPR had been performed: the weekend group (ICPR on Saturdays, Sundays, or legal holidays) and the weekday group (ICPR on Monday, Tuesday, Wednesday, Thursday, and Friday).
Information collected as covariates
We extracted and collected covariates that might be related to the prognosis of ICPR. Data on age, sex, job status, residence, and household income level at ICPR were collected. Residence data, such as living in urban areas (Seoul and other metropolitan cities) or rural areas at the time of admission, were collected based on postal codes. The National Health Insurance Corporation collected information on household income levels at each year to determine patients’ insurance premiums and all patients were divided into four groups using quartile ratios.
The main diagnoses of the patients who underwent ICPR were divided into four groups using the ICD-10 codes such as cardiovascular disease group (I00–I99), respiratory disease group (J00–J99), cancer group (C00–D49), and other group. Hospitalization departments at the time of CPR were classified as internal medicine (IM) and non-IM. The ICPR event was classified into one of five groups according to the duration of CPR: <15, 15–30, 30–45, 45–60, and >60 min, respectively.
Hospitals in which ICPRs were performed were classified into three categories: tertiary general hospitals, general hospitals, and other hospitals. Additionally, hospitals were divided into two distinct groups according to the number of hospital beds: <1,000 beds and ≥1,000 beds. To reflect the comorbid status of patients, the Charlson comorbidity index scores were calculated using ICD-10 codes, which were registered recently (within 1 year before ICPR) in the NHIS database as shown in Table S1.
Endpoints
The primary endpoints of this study were 6-month and 1-year mortality, which was considered as any death within 6 months or 1 year from the date of ICPR. As the date of death among the study population was extracted up to April 22, 2020, the survival time was calculated from the date of ICPR to death date or to April 22, 2020 for survivors of ICPR.
Statistical analysis
Mean values with standard deviation (SD), and number (percentages) were used to present clinicopathological characteristics of the study population, respectively. First, we used 1:1 propensity score matching (PSM) to adjust for confounding factors between the weekend and weekday groups. The nearest neighbor method without replacement was used for PSM and caliper width was set as 0.15 (11). All covariates were included in the propensity score modelling, and absolute standardized difference (ASD) ≤0.1 was used for determining sufficient covariate balance between the two group. For PSM, we used the MatchIt package of the R program (version 4.0.3; www.r-project.org). After checking for an appropriate balance between the weekend and weekday groups, we performed Cox regression analysis to examine whether the risk of 6-month and 1-year mortality differed between the two groups. In this time-to-event analysis, survival time from the date of CPR to the date of death was used as the time, and death within 6 months and 1 year were used as events. In addition, after PSM, Kaplan-Meier estimation was used to compare the median survival time after ICPR between the two groups, and the log-rank test was used to check for statistical differences in median survival time between the two groups.
Next, we performed sensitivity analyses in the entire cohort using multivariable Cox regression modeling for two reasons. First, we could confirm that our results after PSM are generalizable to the entire cohort. Second, we could examine whether the risk of 6-month and 1-year mortality differed according to the date of the weekday in detail. The 6-month and 1-year mortality risks of patients who underwent ICPR on Mondays, Tuesdays, Thursdays, Fridays, Saturdays, and Sundays were compared to those who underwent ICPR on Wednesday. The results are presented as hazard ratios (HRs) with 95% confidence intervals (CIs), and there was no issue of multicollinearity between variables according to the criterion of variance inflation factor <2.0. A log-log plot was used to confirm that the central assumption of the Cox proportional hazard model was satisfied. All the analyses in this study except for PSM were performed using SPSS software (IBM SPSS Statistics for Windows, Version 25.0, IBM Corp., Armonk, NY, USA). Statistical significance was set at two-sided P<0.05.
Results
Characteristics
There were a total of 478,836 CPR cases between January 1, 2010, and December 31, 2019, in South Korea. After excluding 140,046 cases due to out-of-hospital cardiac arrest (OHCA), 338,970 ICPR cases were initially screened. Next, 31,122 cases in which a patient received ICPR more than once on different days during the study period and 8,992 pediatric cases (patients under 18 years of age) were excluded from the final analysis. Finally, 298,676 adult patients were included in the study. Among them, 84,154 (28.2%) patients were in the weekend group, while 214,522 (71.8%) patients were in the weekday group. After PSM, 168,308 patients (84,154 patients in each group) were included in the analysis (Figure 1). Table 1 shows the results of the comparison of clinicopathological characteristics between the weekend and weekday groups before and after PSM. After PSM, the two groups were appropriately balanced, as all ASDs were <0.1. There were no missing data in this study, except for those for household income level at ICPR. The missing value for household income level was considered as an “unknown group” and included in the analysis.
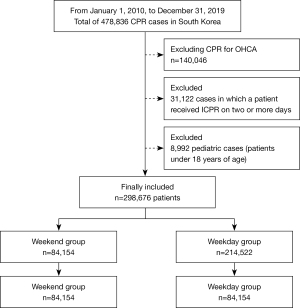
Table 1
| Variables | Before PSM (n=298,676) | ASD | After PSM (n=168,308) | ASD | ||
|---|---|---|---|---|---|---|
| Weekend group (n=84,154) | Weekday group (n=214,522) | Weekend group (n=84,154 | Weekday group (n=84,154) | |||
| Age (years) | 69.5 (15.3) | 70.0 (15.1) | 0.029 | 69.5 (15.3) | 69.6 (15.3) | 0.008 |
| Sex (male), n (%) | 51,105 (60.7) | 129,289 (60.3) | 0.009 | 51.105 (60.7) | 51,184 (60.8) | 0.002 |
| Have a job at ICPR, n (%) | 43,511 (51.7) | 109,542 (51.1) | 0.013 | 43,511 (51.7) | 43,392 (51.6) | 0.003 |
| Residence at ICPR, n (%) | ||||||
| Urban area | 36,356 (43.2) | 92,701 (43.2) | 36,356 (43.2) | 40,762 (48.4) | ||
| Rural area | 47,798 (56.8) | 121,821 (56.8) | <0.001 | 47,798 (56.8) | 43,392 (51.6) | 0.002 |
| Household income level at ICPR, n (%) | ||||||
| Q1 (lowest) | 26,072 (31.0) | 67,706 (31.6) | 26,072 (31.0) | 26,113 (31.0) | ||
| Q2 | 12,982 (15.4) | 33,244 (15.5) | 0.002 | 12,982 (15.4) | 13,126 (15.6) | 0.005 |
| Q3 | 16,666 (19.8) | 41,962 (19.6) | 0.006 | 16,666 (19.8) | 16,519 (19.6) | 0.004 |
| Q4 (highest) | 26.825 (31.9) | 67,599 (19.6) | 0.008 | 26.825 (31.9) | 26,815 (31.9) | <0.001 |
| Unknown | 1,609 (1.9) | 4,011 (1.9) | 0.003 | 1,609 (1.9) | 1,581 (1.9) | 0.002 |
| Main diagnosis at ICPR, n (%) | ||||||
| Cardiovascular disease | 34,289 (40.7) | 80,870 (37.7) | 34,289 (40.7) | 33,877 (40.3) | ||
| Respiratory disease | 11,322 (13.5) | 30,627 (14.3) | 0.024 | 11,322 (13.5) | 11,478 (13.6) | 0.005 |
| Cancer | 8,410 (10.0) | 25,088 (11.7) | 0.057 | 8,410 (10.0) | 8,605 (10.2) | 0.008 |
| Other | 30,123 (35.8) | 77,937 (36.3) | 0.011 | 30,123 (35.8) | 30,194 (35.9) | 0.002 |
| Admitting department, n (%) | ||||||
| IM | 45,274 (53.8) | 121,505 (56.6) | 45,274 (53.8) | 46,005 (54.7) | ||
| Non-IM | 38,880 (46.2) | 93,017 (43.4) | 0.057 | 38,880 (46.2) | 38,149 (45.3) | 0.017 |
| Duration of ICPR, n (%) | ||||||
| <15 min | 38,871 (46.2) | 96,794 (45.1) | 38,871 (46.2) | 38,503 (45.8) | ||
| 15–30 min | 62,080 (28.9) | 62,080 (28.9) | 0.003 | 62,080 (28.9) | 24,512 (29.1) | 0.002 |
| >30–45 min | 11,249 (13.4) | 29,599 (13.8) | 0.013 | 11,249 (13.4) | 11,363 (13.5) | 0.004 |
| >45–60 min | 5,121 (6.1) | 14,106 (6.6) | 0.021 | 5,121 (6.1) | 5,275 (6.3) | 0.008 |
| >60 min | 4,459 (5.3) | 11,943 (5.6) | 0.012 | 4,459 (5.3) | 4,501 (5.3) | 0.002 |
| Type of hospital, n (%) | ||||||
| Tertiary general hospital | 32,686 (38.8) | 79,604 (37.1) | 32,686 (38.8) | 32,493 (38.6) | ||
| General hospital | 43,352 (51.5) | 109,968 (51.3) | 0.005 | 43,352 (51.5) | 43,493 (51.7) | 0.003 |
| Other hospital | 8,116 (9.6) | 24,950 (11.6) | 0.067 | 8,116 (9.6) | 8,168 (9.7) | 0.002 |
| Total hospital bed number, n (%) | ||||||
| <1,000 | 71,006 (84.4) | 182,178 (84.9) | 71,006 (84.4) | 71,079 (84.5) | ||
| ≥1,000 | 13,148 (15.6) | 32,344 (15.1) | 0.015 | 13,148 (15.6) | 13,075 (15.5) | 0.002 |
| Annual case volume of ICPR, n (%) | ||||||
| 0–56 | 19,022 (22.6) | 55,789 (26.0) | 19,022 (22.6) | 19,179 (22.8) | ||
| 57–194 | 21,763 (25.9) | 54,444 (25.4) | 0.011 | 21,763 (25.9) | 21,912 (26.0) | 0.004 |
| 195–276 | 21,449 (25.5) | 51,464 (24.0) | 0.034 | 21,449 (25.5) | 21,256 (25.3) | 0.005 |
| 277 | 21,920 (26.0) | 52,825 (24.6) | 0.032 | 21,920 (26.0) | 21,807 (25.9) | 0.003 |
| Underlying disability | ||||||
| Mild to moderate, n (%) | 9,781 (11.6) | 25,515 (11.9) | 0.009 | 9,781 (11.6) | 9,862 (11.7) | 0.003 |
| Severe, n (%) | 12,426 (16.9) | 37,442 (17.5) | 0.014 | 12,426 (16.9) | 14,285 (17.0) | 0.001 |
| CCI at ICPR, mean (SD) | 5.9 (3.8) | 6.1 (3.9) | 0.056 | 5.9 (3.8) | 5.9 (3.8) | 0.012 |
| Myocardial infarction, n (%) | 15,405 (18.3) | 38,752 (18.1) | 0.006 | 15,405 (18.3) | 15,282 (18.2) | 0.004 |
| Congestive heart failure, n (%) | 32,643 (38.8) | 84,954 (39.6) | 0.017 | 32,643 (38.8) | 32,775 (38.9) | 0.003 |
| Peripheral vascular disease, n (%) | 19,488 (23.2) | 51,067 (23.8) | 0.015 | 19,488 (23.2) | 19,744 (23.5) | 0.007 |
| Cerebrovascular disease, n (%) | 31,871 (37.9) | 80,886 (37.7) | 0.003 | 31,871 (37.9) | 34,695 (37.7) | 0.004 |
| Dementia, n (%) | 18,736 (22.3) | 49,021 (22.9) | 0.014 | 18,736 (22.3) | 18,700 (22.2) | 0.001 |
| Chronic pulmonary disease, n (%) | 45,912 (54.6) | 120,136 (56.0) | 0.029 | 45,912 (54.6) | 46,321 (55.0) | 0.009 |
| Rheumatic disease, n (%) | 5,245 (6.2) | 14,288 (6.7) | 0.018 | 5,245 (6.2) | 5,373 (6.4) | 0.006 |
| Peptic ulcer disease, n (%) | 32,081 (38.1) | 84,438 (39.4) | 0.026 | 32,081 (38.1) | 32,134 (38.2) | 0.001 |
| Mild liver disease, n (%) | 40,414 (48.0) | 104,525 (48.7) | 0.014 | 40,414 (48.0) | 40,615 (48.3) | 0.005 |
| Diabetes without chronic complication, n (%) | 48,2588 (57.7) | 125,706 (58.6) | 0.017 | 48,2588 (57.7) | 49,056 (58.3) | 0.011 |
| Diabetes with chronic complication, n (%) | 19,261 (22.9) | 50,629 (23.6) | 0.017 | 19,261 (22.9) | 19,521 (23.2) | 0.007 |
| Hemiplegia or paraplegia, n (%) | 22,345 (26.6) | 58,742 (27.4) | 0.019 | 22,345 (26.6) | 22,585 (26.8) | 0.007 |
| Renal disease, n (%) | 13,981 (16.6) | 37,593 (17.5) | 0.025 | 13,981 (16.6) | 25,266 (16.8) | 0.006 |
| Cancer, n (%) | 22,214 (26.4) | 60,919 (28.4) | 0.045 | 22,214 (26.4) | 22,474 (26.7) | 0.007 |
| Moderate or severe liver disease, n (%) | 5,503 (6.5) | 14,006 (6.5) | <0.001 | 5,503 (6.5) | 5,479 (6.5) | 0.001 |
| Metastatic cancer, n (%) | 6,152 (7.3) | 18,307 (8.5) | 0.047 | 6,152 (7.3) | 6,281 (7.5) | 0.006 |
| AIDS/HIV, n (%) | 152 (0.2) | 434 (0.2) | 0.005 | 152 (0.2) | 158 (0.2) | 0.002 |
| Year of ICPR, n (%) | ||||||
| 2010 | 6,541 (7.8) | 17,945 (8.4) | 6,541 (7.8) | 6,571 (7.8) | ||
| 2011 | 6,696 (8.0) | 17,473 (8.1) | 0.007 | 6,696 (8.0) | 6,858 (8.1) | 0.007 |
| 2012 | 6,855 (8.1) | 17,751 (8.3) | 0.005 | 6,855 (8.1) | 6,829 (8.1) | 0.001 |
| 2013 | 6,681 (7.9) | 17,411 (8.1) | 0.007 | 6,681 (7.9) | 6,800 (8.1) | 0.005 |
| 2014 | 6,365 (7.6) | 17,331 (8.1) | 0.020 | 6,365 (7.6) | 6,498 (7.7) | 0.06 |
| 2015 | 6,434 (7.6) | 17,377 (8.1) | 0.017 | 6,434 (7.6) | 6,539 (7.8) | 0.005 |
| 2016 | 10,327 (12.3) | 25,553 (11.9) | 0.011 | 10,327 (12.3) | 10,348 (12.3) | <0.001 |
| 2017 | 10,340 (12.3) | 25,554 (11.9) | 0.011 | 10,340 (12.3) | 10,207 (12.1) | 0.005 |
| 2018 | 12,085 (14.4) | 29,524 (13.8) | 0.017 | 12,085 (14.4) | 11,950 (14.2) | 0.005 |
| 2019 | 11,830 (14.1) | 28,603 (13.3) | 0.021 | 11,830 (14.1) | 11,554 (13.7) | 0.009 |
PSM, propensity score matching, ASD, absolute value of standardized mean difference; ICPR, in-hospital cardiopulmonary resuscitation; IM, internal medicine; CCI, Charlson comorbidity index; AIDS, Acquired immunodeficiency syndrome; HIV, human immunodeficiency virus.
Comparison of 6-month and 1-year mortality rates of patients who underwent ICPR on weekends and weekdays
Table 2 shows the survival analyses before and after PSM. After PSM, the 6-month mortality rate in the weekend group was 90.1% (75,805/84,154), while that in the weekday group was 90.0% (75,771/84,154). In the Cox regression analysis, the weekend group showed a 2% increased 6-month mortality risk compared to the weekday group (HR =1.02, 95% CI: 1.01–1.03; P<0.001). After PSM, the 1-year mortality rate in the weekend group was 91.2% (76,776/84,154), while that in the weekday group was 91.2% (76,768/84,154). In the Cox regression analysis, the weekend group showed a 2% increase in the 1-year mortality risk compared to the weekday group (HR =1.02, 95% CI: 1.01–1.03; P<0.001). Table 3 shows the median survival times after ICPR between the weekend and weekday groups. The median survival time after ICPR in the weekend group was 3 days (95% CI: 2.9–3.1), which was significantly shorter than the median survival time of 4 days (95% CI: 3.9–4.1) in the weekday group (P<0.001).
Table 2
| Variables | Event | Cox regression analysis, HR (95% CI) | P value |
|---|---|---|---|
| 6-month mortality before PSM | |||
| Weekday | 193,568/214,522 (90.2%) | 1 | |
| Weekend | 75,805/84,154 (90.1%) | 1.04 (1.03–1.04) | <0.001 |
| 1-year mortality before PSM | |||
| Weekday | 196,050/214,522 (91.4%) | 1 | |
| Weekend | 76,775/84,154 (91.2%) | 1.03 (1.03–1.04) | <0.001 |
| 6-month mortality after PSM | |||
| Weekday | 75,771/84,154 (90.0%) | 1 | |
| Weekend | 75,805/84,154 (90.1%) | 1.02 (1.01–1.03) | <0.001 |
| 1-year mortality after PSM | |||
| Weekday | 76,768/84,154 (91.2%) | 1 | |
| Weekend | 76,776/84,154 (91.2%) | 1.02 (1.01–1.03) | <0.001 |
PSM, propensity score matching; HR, hazard ratio; CI, confidence interval.
Table 3
| Group | Median survival time (95% CI) |
|---|---|
| Weekday | 3 days (2.9–3.1) |
| Weekend | 4 days (3.9–4.1) |
| P value | <0.001 |
ICPR, in-hospital cardiopulmonary resuscitation; CI, confidence interval.
Associated factors for 1-year mortality
Table 4 shows the results of the multivariable Cox regression model for 1-year mortality among the entire cohort as a sensitivity analysis. In model 1, the weekend group showed a 4% increase in 1-year mortality risk compared to the weekday group (HR =1.04, 95% CI: 1.03–1.05; P<0.001). In model 2, compared with the patients who received ICPR on Wednesday, the 1-year mortality risk in patients who received ICPR on Saturday and Sunday was increased by 5% (HR =1.05, 95% CI: 1.04–1.07; P<0.001) and 4% (HR =1.04, 95% CI: 1.03–1.06; P<0.001) respectively. However, the 1-year mortality risk in patients who received ICPR on Thursday (P=0.911), Friday (P=0.502), Monday (P=0.194), and Tuesday (P=0.371) were not significantly different from that of patients who received ICPR on Wednesday.
Table 4
| Variables | HR (95% CI) | P value |
|---|---|---|
| Weekend (vs. weekday; model 1) | 1.04 (1.03–1.05) | <0.001 |
| Weekday in detail (model 2) | ||
| Wednesday (n=43,113) | 1 | |
| Thursday (n=42,717) | 1.00 (0.99–1.01) | 0.911 |
| Friday (n=44,212) | 1.00 (0.98–1.01) | 0.502 |
| Saturday (n=36,441) | 1.05 (1.04–1.07) | <0.001 |
| Sunday (n=35,485) | 1.04 (1.03–1.06) | <0.001 |
| Monday (n=51,651) | 0.99 (0.98–1.01) | 0.194 |
| Tuesday (n=45,057) | 0.99 (0.98–1.01) | 0.371 |
| Other covariates in model 1 | ||
| Age, year | 1.01 (1.01–1.01) | <0.001 |
| Sex, male | 1.03 (1.03–1.04) | <0.001 |
| Have a job at ICPR | 1.00 (0.99–1.00) | 0.179 |
| Residence at ICPR | ||
| Urban area | 1 | |
| Rural area | 1.02 (1.01–1.03) | <0.001 |
| Household income level at ICPR | ||
| Q1 (lowest) | 1 | |
| Q2 | 0.99 (0.98–1.00) | 0.185 |
| Q3 | 0.98 (0.97–0.99) | 0.001 |
| Q4 | 0.98 (0.97–0.99) | <0.001 |
| Unknown | 0.99 (0.97–1.00) | 0.179 |
| Main diagnosis at ICPR | ||
| Cardiovascular disease | 1 | |
| Respiratory disease | 0.91 (0.89–0.92) | <0.001 |
| Cancer | 0.82 (0.81–0.84) | <0.001 |
| Other | 0.92 (0.91–0.93) | <0.001 |
| Admitting department | ||
| IM | 1 | |
| Non-IM | 0.70 (0.69–0.70) | <0.001 |
| Duration of ICPR | ||
| <15 min | 1 | |
| >15–30 min | 1.63 (1.62–1.65) | <0.001 |
| >30–45 min | 1.70 (1.68–1.72) | <0.001 |
| >45–60 min | 1.67 (1.65–1.70) | <0.001 |
| >60 min | 1.65 (1.63–1.68) | <0.001 |
| Type of hospital | ||
| Tertiary general hospital | 1 | |
| General hospital | 1.14 (1.13–1.15) | <0.001 |
| Other hospital | 1.08 (1.06–1.10) | <0.001 |
| Total hospital bed number | ||
| <1,000 | 1 | |
| ≥1,000 | 1.02 (1.01–1.03) | 0.001 |
| Annual case volume of ICPR | ||
| 0–56 | 1 | |
| 57–194 | 1.07 (1.06–1.09) | <0.001 |
| 195–276 | 1.06 (1.05–1.08) | <0.001 |
| 277 | 1.18 (1.16–1.19) | <0.001 |
| Underlying disability | ||
| Mild to moderate | 1.01 (1.00–1.02) | 0.048 |
| Severe | 1.00 (0.99–1.01) | 0.873 |
| Myocardial infarction | 0.86 (0.85–0.86) | <0.001 |
| Congestive heart failure | 0.93 (0.92–0.94) | <0.001 |
| Peripheral vascular disease | 0.96 (0.95–0.97) | <0.001 |
| Cerebrovascular disease | 0.88 (0.87–0.89) | <0.001 |
| Dementia | 1.01 (1.00–1.02) | 0.096 |
| Chronic pulmonary disease | 0.77 (0.76–0.77) | <0.001 |
| Rheumatic disease | 1.00 (0.99–1.02) | 0.856 |
| Peptic ulcer disease | 0.90 (0.90–0.91) | <0.001 |
| Mild liver disease | 0.93 (0.92–0.94) | <0.001 |
| Diabetes without chronic complication | 0.89 (0.89–0.90) | <0.001 |
| Diabetes with chronic complication | 1.13 (1.12–1.15) | <0.001 |
| Hemiplegia or paraplegia | 0.86 (0.85–0.87) | <0.001 |
| Renal disease | 0.96 (0.95–0.97) | <0.001 |
| Cancer | 1.01 (1.00–1.02) | 0.048 |
| Moderate or severe liver disease | 1.29 (1.27–1.31) | <0.001 |
| Metastatic cancer | 1.13 (1.11–1.14) | <0.001 |
| AIDS/HIV | 1.00 (0.92–1.09) | 0.982 |
| Year of ICPR | ||
| 2010 | 1 | |
| 2011 | 0.99 (0.97–1.01) | 0.216 |
| 2012 | 0.99 (0.97–1.301) | 0.281 |
| 2013 | 1.01 (0.99–1.03) | 0.379 |
| 2014 | 1.00 (0.99–1.02) | 0.700 |
| 2015 | 1.02 (1.00–1.04) | 0.067 |
| 2016 | 1.32 (1.29–1.34) | <0.001 |
| 2017 | 1.33 (1.31–1.36) | <0.001 |
| 2018 | 1.31 (1.29–1.33) | <0.001 |
| 2019 | 1.30 (1.28–1.33) | <0.001 |
ICPR, in-hospital cardiopulmonary resuscitation; IM, internal medicine; HR, hazard ratio; CI, confidence interval; AIDS, acquired immunodeficiency syndrome; HIV, human immunodeficiency virus.
Discussion
The “weekend effect” on post-ICPR 6-month and 1-year mortality was demonstrated even after adjusting for patient factors such as underlying disease, employment status, financial status, residence, hospital factors, and duration of ICPR using data (n=298,676) that were extracted from the National Health Insurance Service database in Republic of Korea in 2010–2019.
A few studies based on data from the CPR registry (n=8,000–60,000 patients) in other countries have suggested a weekend effect on survival to discharge in patients who underwent IHCA (5,7-9). However, no studies using a national database in South Korea have been conducted to investigate the weekend effect on post-ICPR mortality including long-term survival, such as 6-month and 1-year mortality. In this study, the results showed that the “weekend effect” might be maintained for 1 year after CPR even after adjusting for risk factors.
“Weekend effect” in CPR has different meanings in OHCA and IHCA. Studies on OHCA or out-of-hospital CPR at night or on weekends have been conducted, and the results have been mixed (12-15). A study conducted in Paris found that the “weekend/night effect” on outcomes of out-of-hospital CPR can be due to the fact that bystander CPR was less frequently performed and automatic external defibrillator (AED) application was delayed even if there were more bystanders on weekends or nights than during the day (13). This result differs from the results of studies in other countries. This may be related to the educational level and participation tendency of local residents on bystander CPR or usage of AEDs, security, and population distribution at night and on weekends (13,14).
On the other hand, weekend IHCA is usually predicted to have a lower survival rate due to a decrease in the number of medical staff, change of medical staff, shortage of a limited accessibility to specialists, and decrease in monitoring personnel (16). As the most common cause of pediatric cardiopulmonary arrest is respiratory problems, the clinical outcome of ICPR at a time when personnel skilled in managing the airway and intubation is not available may be worse than that of ICPR performed during the day (6,17-19). This also applies to adult CPR. The latest American Heart Association guidelines recommend minimizing interruption to chest compression, but it is difficult to intubate without interruption of CPR (20,21). Kim et al. found that they could improve the success rate of intubation and shorten the time to successful intubation with training. A total of 243 endotracheal intubation experiences (1,973 days of training) were necessary to achieve a 90% success rate at <30 s (20,21). However, rescuers highly skilled in airway management and monitoring and maintaining the quality of CPR may not be available on weekends and nights, particularly in smaller hospitals. In this study, the type of hospital, general hospitals, or others (vs. tertiary general hospital), total hospital bed number, and annual case volume of ICPR were associated with 1-year mortality after ICPR. This may be due not only to better hospital systems, including CPR systems, but also to the availability of highly skilled staff 24 h a day.
The study by Thorén et al. demonstrated an association between electrocardiogram (EKG) monitoring and reduction in mortality in IHCA (22), suggesting that the lack of monitors, such as those used for EKG monitoring, may increase the mortality at night because early detection of a shockable rhythm and rapid defibrillation or cardiac catheterization is important in the ROSC and survival in adults (23). According to an analysis of 6,789 cases from 369 hospitals participating in the National Registry of Cardiopulmonary Resuscitation, delayed defibrillation was significantly associated with a lower survival rate in cases of in-hospital cardiac arrest (5). This is closely related to problems such as the availability of monitoring equipment, monitoring personnel, and professionals (5).
Furthermore, according to an analysis of 118,387 consecutive, adult, index IHCA cases in the National Registry of Cardiopulmonary Resuscitation database conducted by Ornato et al., the errors in the in-hospital CPR system were more frequent during weekends (30.7% vs. 31.6%, error group vs. no error group, P=0.003), and this was significantly associated with in-hospital mortality (24).
In our study, cardiovascular disease, such as myocardial infarction, was the main diagnosis in cases of cardiopulmonary arrest, and CPR was associated with a lower 1-year mortality. Patients with myocardial infarction admitted to the hospital on weekdays may be associated with lower in-hospital mortality. A study by Kostis et al., who enrolled 241,164 cases from 1987 to 2002 in New Jersey, showed that patients with myocardial infarction hospitalized on weekends had increased mortality; lower use of invasive cardiac procedures was also observed in these patients (25). A lower rate of invasive cardiac intervention might cause higher mortality in patients with myocardial infarction admitted to the hospital on weekends (25). In a recent study on the weekend effect of myocardial infarction based on data from 2000 to 2016, there were no differences in the in-hospital mortality of acute myocardial infarction according to admission on weekdays vs. weekends in the United States (26). This implies that the weekend effect is not permanent and fixed, and might be improved by fast-tracking development of a system for rapid cardiac procedures and increasing professional staff for this on weekends. In our study, the year in which ICPR occurred was adjusted for; however, the weekend effect was maintained.
This study has some limitations. First, we could not access data for ROSC after ICPR because there is no ICD-10 code for this in the NHIS database. Second, it was not possible to extract important information such as the habits of the patients and their body mass index, other than the data registered in the National Health Insurance database. Third, missing data could not be obtained because attending physicians at individual hospitals did not enter the codes. Fourth, the patients’ disease severity at ICPR was not included in the analysis, which might affect the results of this study. For example, Acute Physiology and Chronic Health Evaluation II scores at ICPR were not included in this study as this information was unavailable in the NHIS database. Finally, although the data in this study include all ICPR cases across the country, these data were collected only from South Korea. It may be difficult to generalize the results of the study to different medical systems and cultures.
Conclusions
The consistent weekend effect before and after adjustment for confounders in this study may be due to the complex reasons listed above: the decrease in monitoring due to shortage and change of medical staff and professionals, delay in defibrillation and cardiac procedures, delay in diagnosis and treatment of major cardiopulmonary problems, quality of CPR, and decrease in the success rate of airway intubation. The fact that the “weekend effect” was consistently demonstrated even after adjusting for the type, size, and ICPR case volume of the hospitals may suggest that overall improvement of the system of ICPR is needed. The fact that the weekend effect on mortality after ICPR lasts as long as a year also suggests that efforts are needed to address the weekend effect.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting Checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-22-266/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-22-266/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This retrospective population-based cohort study was approved by the institutional review board (IRB) of Seoul National University Bundang Hospital (No. X-2011-651-901) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Andersen LW, Holmberg MJ, Berg KM, et al. In-Hospital Cardiac Arrest: A Review. JAMA 2019;321:1200-10. [Crossref] [PubMed]
- Benjamin EJ, Virani SS, Callaway CW, et al. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation 2018;137:e67-e492. Erratum in: Circulation 2018;137:e493. [Crossref] [PubMed]
- Oh TK, Park YM, Do SH, et al. A comparative study of the incidence of in-hospital cardiopulmonary resuscitation on Monday-Wednesday and Thursday-Sunday: Retrospective analysis in a tertiary care hospital. Medicine (Baltimore) 2018;97:e9741. [Crossref] [PubMed]
- Gaieski DF, Abella BS, Goyal M. CPR and postarrest care: overview, documentation, and databases. Chest 2012;141:1082-9. [Crossref] [PubMed]
- Chan PS, Krumholz HM, Nichol G, et al. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med 2008;358:9-17. [Crossref] [PubMed]
- Oh TK, Park YM, Do SH, et al. ROSC rates and live discharge rates after cardiopulmonary resuscitation by different CPR teams - a retrospective cohort study. BMC Anesthesiol 2017;17:166. [Crossref] [PubMed]
- Herlitz J, Bång A, Alsén B, et al. Characteristics and outcome among patients suffering from in hospital cardiac arrest in relation to whether the arrest took place during office hours. Resuscitation 2002;53:127-33. [Crossref] [PubMed]
- Ofoma UR, Basnet S, Berger A, et al. Trends in Survival From In-hospital Cardiac Arrests During Nights and Weekends. Circulation 2016;134:A13260.
- Peberdy MA, Ornato JP, Larkin GL, et al. Survival from in-hospital cardiac arrest during nights and weekends. JAMA 2008;299:785-92. [Crossref] [PubMed]
- Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med 2007;4:e297. [Crossref] [PubMed]
- Rosenbaum PR, Rubin DB. Reducing bias in observational studies using subclassification on the propensity score. Journal of the American Statistical Association 1984;79:516-24. [Crossref]
- El Asmar A, Dakessian A, Bachir R, et al. Out of hospital cardiac arrest outcomes: Impact of weekdays vs weekends admission on survival to hospital discharge. Resuscitation 2019;143:29-34. [Crossref] [PubMed]
- Koike S, Tanabe S, Ogawa T, et al. Effect of time and day of admission on 1-month survival and neurologically favourable 1-month survival in out-of-hospital cardiopulmonary arrest patients. Resuscitation 2011;82:863-8. [Crossref] [PubMed]
- Schriefl C, Mayr FB, Poppe M, et al. Time of out-of-hospital cardiac arrest is not associated with outcome in a metropolitan area: A multicenter cohort study. Resuscitation 2019;142:61-8. [Crossref] [PubMed]
- Karam N, Marijon E, Dumas F, et al. Characteristics and outcomes of out-of-hospital sudden cardiac arrest according to the time of occurrence. Resuscitation 2017;116:16-21. [Crossref] [PubMed]
- Lauridsen KG, Schmidt AS, Adelborg K, et al. Organisation of in-hospital cardiac arrest teams - a nationwide study. Resuscitation 2015;89:123-8. [Crossref] [PubMed]
- Goto Y, Maeda T, Goto Y. Impact of dispatcher-assisted bystander cardiopulmonary resuscitation on neurological outcomes in children with out-of-hospital cardiac arrests: a prospective, nationwide, population-based cohort study. J Am Heart Assoc 2014;3:e000499. [Crossref] [PubMed]
- McInnes AD, Sutton RM, Orioles A, et al. The first quantitative report of ventilation rate during in-hospital resuscitation of older children and adolescents. Resuscitation 2011;82:1025-9. [Crossref] [PubMed]
- Mogayzel C, Quan L, Graves JR, et al. Out-of-hospital ventricular fibrillation in children and adolescents: causes and outcomes. Ann Emerg Med 1995;25:484-91. [Crossref] [PubMed]
- Panchal AR, Bartos JA, Cabañas JG, et al. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020;142:S366-468. [Crossref] [PubMed]
- Kim SY, Park SO, Kim JW, et al. How much experience do rescuers require to achieve successful tracheal intubation during cardiopulmonary resuscitation? Resuscitation 2018;133:187-92. [Crossref] [PubMed]
- Thorén A, Rawshani A, Herlitz J, et al. ECG-monitoring of in-hospital cardiac arrest and factors associated with survival. Resuscitation 2020;150:130-8. [Crossref] [PubMed]
- Garcia S, Drexel T, Bekwelem W, et al. Early Access to the Cardiac Catheterization Laboratory for Patients Resuscitated From Cardiac Arrest Due to a Shockable Rhythm: The Minnesota Resuscitation Consortium Twin Cities Unified Protocol. J Am Heart Assoc 2016;5:002670. [Crossref] [PubMed]
- Ornato JP, Peberdy MA, Reid RD, et al. Impact of resuscitation system errors on survival from in-hospital cardiac arrest. Resuscitation 2012;83:63-9. [Crossref] [PubMed]
- Kostis WJ, Demissie K, Marcella SW, et al. Weekend versus weekday admission and mortality from myocardial infarction. N Engl J Med 2007;356:1099-109. [Crossref] [PubMed]
- Vallabhajosyula S, Patlolla SH, Miller PE, et al. Weekend Effect in the Management and Outcomes of Acute Myocardial Infarction in the United States, 2000-2016. Mayo Clin Proc Innov Qual Outcomes 2020;4:362-72. [Crossref] [PubMed]


