
Incorporating palliative radiotherapy education into hospice and palliative medicine fellowship training: a feasibility study
Introduction
Radiotherapy is an effective and well-tolerated modality in the palliative management of patients with advanced cancer. Palliative radiotherapy can alleviate pain, improve dyspnea, control bleeding, and relieve tumor-associated obstructive and compressive symptoms, thereby improving patients’ quality of life (1-4). Despite estimates that nearly half of all patients referred to radiation oncology are treated with palliative intent, however, palliative radiotherapy remains underutilized (5-7).
Insufficient knowledge about palliative radiotherapy among hospice and palliative medicine (HPM) specialists is a barrier to optimal radiotherapy utilization and to collaboration between HPM physicians and radiation oncologists (4-6). Since physicians who are knowledgeable about the indications for and expected outcomes of palliative radiotherapy are more likely to appropriately refer advanced cancer patients to their radiation oncology colleagues, it has been recommended that curricular interventions address these educational deficiencies (8-14). Yet, to date, there has been little emphasis on incorporating palliative radiotherapy education into HPM fellowship training. In this preliminary, single-center study we sought to assess the feasibility of implementing a brief didactic palliative radiotherapy course and whether such an intervention impacts HPM fellows’ knowledge about, attitudes toward, or practice behaviors associated with the use of palliative radiotherapy.
Methods
The study was reviewed by the Director of the University of California, San Diego Human Research Protections Program and was certified as exempt from full Institutional Review Board and Ethics review as it was determined to not qualify as human subjects research (#180609QI). All participants gave informed consent prior to taking part in this study.
Course design
We developed and implemented a four-hour palliative radiotherapy course for HPM fellows. The course consisted of three one-hour didactic lectures, a guided tour of the radiation oncology suite, and an informal question and answer session with a senior radiation oncology resident. Course content addressed the aspects of palliative radiotherapy determined to be most relevant to HPM physicians, including: indications and contraindications for treatment; the process of preparing a radiotherapy plan; the process of radiation delivery; expected outcomes including onset and duration of symptom relief; common side effects; potential acute and late toxicities; radiation oncology emergencies; potential psychological, social, and physical burdens of treatment; re-irradiation; and use of hypofractionated radiation schedules. Potential barriers to collaboration between HPM physicians and radiation oncologists were also discussed and current models of integrated palliative radiotherapy services were reviewed. Case-based examples were utilized throughout the lectures to provide additional clinical context. During the guided tour of the radiation oncology suite, the fellows viewed a consultation room, planning room, CT simulator, linear accelerator, and brachytherapy suite. Fellows had the opportunity to examine immobilizing face masks and observe treatment planning and radiation delivery.
Survey design and analysis
We developed and distributed a 23-item, anonymous, electronic survey to the eligible fellows one day prior to the first lecture (supplemental data). Survey questions were loosely based on surveys previously administered to other physician groups and were designed to evaluate the following four domains: (I) objective palliative radiotherapy knowledge; (II) self-reported confidence in palliative radiotherapy knowledge; (III) attitudes toward palliative radiotherapy; and (IV) self-reported practice behaviors (12-16). The objective knowledge assessment consisted of eight multiple choice questions. The remaining 18 questions utilized a 5-point Likert-type scale to assess level of agreement with various statements (1= strongly disagree; 5= strongly agree). Post-course and follow-up surveys were distributed one day and three months following completion of the course, respectively. Participation was voluntary. No identifying information was collected and the pre-post surveys were not matched.
Quantitative data analysis was performed using descriptive statistics. A non-parametric version of unpaired t-test (the Wilcoxon rank-sum test with continuity correction) was used to compare the pre-, post-, and follow-up survey results. A P value of <0.05 was used to determine statistical significance.
Results
All eligible HPM fellows (n=5) participated in this course. One fellow was unable to attend the first didactic lecture but did review the presentation slides independently.
Pre- and post-course survey results
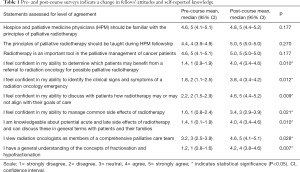
Five fellows (100% response rate) completed the pre- and post-course surveys. On pre-course assessment, all fellows either agreed or strongly agreed that radiotherapy is an important tool in the palliative management of patients with advanced cancer, that HPM physicians should be familiar with the principles of palliative radiotherapy, and that formal didactic training in palliative radiotherapy should be implemented during HPM fellowship. Despite this, prior to the course, all fellows rated their knowledge about palliative radiotherapy as insufficient; this was supported by a mean score of 22% on the pre-course objective knowledge assessment. All respondents lacked confidence in their ability to identify radiation oncology emergencies, to determine which patients might benefit from referral to radiation oncology, and to discuss with patients whether palliative radiotherapy aligns with their goals of care. Further, only two fellows (40%) indicated that they viewed radiation oncologists as members of a comprehensive palliative care team and none of the respondents reported that they were likely to collaborate with the radiation oncologists involved in their patients’ care.
Post-course surveys revealed a significant increase in fellows’ knowledge about palliative radiotherapy, with a mean score on the post-course objective knowledge assessment of 86% (P=0.010). The course was also associated with a significant increase in fellow-reported confidence in identifying radiation oncology emergencies (P=0.012), determining which patients might benefit from referral to radiation oncology (P=0.010), and discussing with patients whether palliative radiotherapy aligns with their goals of care (P=0.009) (Table 1). Following the course, 100% of fellows viewed radiation oncologists as members of a comprehensive palliative care team (P=0.028).
Full table
Longitudinal assessment results
Five fellows completed a follow-up survey three months after completion of the course (100% response rate). The mean score of the objective knowledge assessment was 80%, suggesting that knowledge obtained through the course was effectively retained (P=0.010). All five respondents either agreed or strongly agreed that they had been more likely to refer patients with painful bone metastases, tumor-related bleeding, or tumor-related compressive/obstructive symptoms for palliative radiotherapy in the three months since participating in the course compared to the three months prior to the course (P=0.009). Four fellows (80%) either agreed or strongly agreed that they were more likely to collaborate with the radiation oncologists involved in their patients’ care (P=0.014). Four fellows (80%) indicated that they were more likely to advocate for shorter fractionation regimens and to discuss their concerns regarding initiation of palliative radiotherapy in patients at end-of-life with their radiation oncology colleagues, although this did not meet statistical significance (P=0.083) (Figure 1).

Discussion
The results of this single-institution feasibility study suggest that a brief curricular intervention may significantly impact HPM fellows’ knowledge about, attitudes towards, and practice behaviors associated with the use of radiotherapy in the palliative management of patients with advanced cancer. The four-hour course was associated with a significant increase in fellows’ palliative radiotherapy knowledge with retention of this knowledge observed on longitudinal assessment at three months. The course was also associated with a statistically significant change in fellows’ perception of radiation oncologists as members of a comprehensive palliative care team and with fellows’ self-reported clinical practice behaviors. Specifically, fellows reported that they were significantly more likely to refer advanced cancer patients for palliative radiotherapy and to collaborate with their radiation oncology colleagues in the three months following the course compared to the three months prior to their participation in the course. There was a trend toward being more likely to advocate for shorter fractionation regimens and to discuss concerns about initiating palliative radiotherapy for patients with a prognosis of days to weeks, although these did not meet statistical significance.
Our study builds on existing data indicating that lack of knowledge about palliative radiotherapy among referring providers is a significant barrier to optimal use of palliative radiotherapy for advanced cancer patients and that addressing these educational deficiencies has the potential to improve the quality of palliative oncology care (11,17). In a national survey of members of the American Academy of Hospice and Palliative Medicine (AAHPM) and the American Society for Radiation Oncology (ASTRO), over 40% of respondents indicated that lack of knowledge about radiotherapy was a key barrier to palliative radiotherapy referral (8). The same survey revealed that, compared to their medical oncology and radiation oncology colleagues, HPM physicians were the least likely to be familiar with common indications for palliative radiotherapy (8). In another national survey of HPM professionals, nearly half of the respondents rated themselves as insufficiently trained to know when to consider referral for palliative radiotherapy (6). This lack of familiarity with common indications for treatment contributes, in part, to the infrequent use of palliative radiotherapy for hospice patients. Accordingly, while approximately half of all patients enrolled in hospice carry a diagnosis of incurable malignancy, many of whom are acutely symptomatic, less than 1% of hospice patients are referred to radiation oncology (6,18,19).
A recently published systematic review of the barriers to palliative radiotherapy calls for dedicated efforts to increase in-person interprofessional palliative radiotherapy education for referring physicians (11). A national education program designed to improve primary care providers’ knowledge of radiotherapy was recently implemented in Australia with improvement in providers’ knowledge on post-course assessment (13). To our knowledge, however, the impact of a palliative radiotherapy curricular intervention for HPM physicians has not previously been evaluated.
There are several significant limitations to this study. First, the pre- and post-course surveys were unmatched, limiting the statistical power in analysis. In addition, the generalizability of our results is limited due to the fact that this was a single-center study with a very small sample size of only five fellows. Further, the survey questions relied on fellows’ self-report and are therefore subject to bias. As a preliminary feasibility study, however, we found that the structure of our brief course, including lectures addressing the aspects of palliative radiotherapy most relevant to HPM specialists, a tour of the radiation oncology suite, and a question-and-answer session, was well-received and easily implemented with statistically significant changes in knowledge, attitudes, and reported clinical practice behaviors a three-month follow-up (20).
In conclusion, radiotherapy plays an essential role in the palliative management of many patients with advanced cancer. HPM physicians should possess a working knowledge of palliative radiotherapy including its indications and common toxicities so that they can best provide high-quality palliative cancer care. Currently there are no standards for incorporating palliative radiotherapy education into HPM fellowship training; as a result, focused efforts to increase HPM physicians’ familiarity with key palliative radiotherapy concepts are necessary. This single-center, preliminary feasibility study suggests that a brief curricular intervention may be effective at addressing the existing knowledge gap. Further studies to evaluate the generalizability of these preliminary results are needed.
Supplementary
Palliative radiotherapy education for hospice and palliative medicine fellows
- The median time to pain relief after palliative radiotherapy for painful bone metastases is ___ weeks.
- <2
- 2–4
- 4–8
- 8–12
- ≥12
- The median duration of pain relief after palliative radiotherapy for painful bone metastases is ___ weeks.
- <6
- 6–10
- 10–14
- 14–18
- ≥18
- Acute side effects of radiotherapy typically resolve within ____ weeks of completing treatment.
- 0–2
- 2–4
- 4–6
- 6–8
- For patients with relapsed or non-responsive bone pain, re-irradiation of a bone metastasis is typically contraindicated.
- True
- False
- Palliative radiotherapy can effectively treat tumor-associated hemoptysis.
- True
- False
- Palliative radiotherapy should typically not be considered for patients with a life expectancy of less than 3 months.
- True
- False
- What percentage of patients treated with palliative radiotherapy for painful bone metastases will achieve pain relief (partial or complete)?
- 0–19%
- 20–39%
- 40–59%
- 60–79%
- 80–100%
- Short- and long-course treatment schedules are equally effective in treating painful, uncomplicated bone metastases.
- True
- False
- Hospice and palliative medicine physicians should be familiar with the principles of palliative radiotherapy.
- Strongly agree
- Somewhat agree
- Neither agree nor disagree
- Somewhat disagree
- Strongly disagree
- I routinely consider radiotherapy as an option for the palliation of symptoms associated with advanced cancer.
- Strongly agree
- Somewhat agree
- Neither agree nor disagree
- Somewhat disagree
- Strongly disagree
- Radiotherapy is an integral component of comprehensive palliative care for many advanced cancer patients.
- Strongly agree
- Somewhat agree
- Neither agree nor disagree
- Somewhat disagree
- Strongly disagree
- I view radiation oncologists as members of a comprehensive palliative care team.
- Strongly agree
- Somewhat agree
- Neither agree nor disagree
- Somewhat disagree
- Strongly disagree
- The principles of palliative radiotherapy should be taught during hospice and palliative medicine fellowship.
- Strongly agree
- Somewhat agree
- Neither agree nor disagree
- Somewhat disagree
- Strongly disagree
- I feel confident in my ability to determine which patients may benefit from a referral to radiation oncology for possible palliative radiotherapy.
- Strongly agree
- Somewhat agree
- Neither agree nor disagree
- Somewhat disagree
- Strongly disagree
- I feel confident in my ability to discuss with patients how radiotherapy may or may not align with their goals of care.
- Strongly agree
- Somewhat agree
- Neither agree nor disagree
- Somewhat disagree
- Strongly disagree
- I feel confident in my ability to identify the clinical signs and symptoms of a radiation oncology emergency.
- Strongly agree
- Somewhat agree
- Neither agree nor disagree
- Somewhat disagree
- Strongly disagree
- I have a general understanding of the concepts of fractionation and hypofractionation.
- Strongly agree
- Somewhat agree
- Neither agree nor disagree
- Somewhat disagree
- Strongly disagree
- I am knowledgeable about potential acute and late side effects of radiotherapy.
- Strongly agree
- Somewhat agree
- Neither agree nor disagree
- Somewhat disagree
- Strongly disagree
- I am likely to refer patients with painful bone metastases, tumor-related bleeding, or tumor-related compressive/obstructive symptoms to radiation oncology for possible palliative radiotherapy.
- Strongly agree
- Somewhat agree
- Neither agree nor disagree
- Somewhat disagree
- Strongly disagree
- I am likely to collaborate with the radiation oncologists involved in my patients’ care.
- Strongly agree
- Somewhat agree
- Neither agree nor disagree
- Somewhat disagree
- Strongly disagree
- I am likely to advocate for shorter fractionation schedules or possible omission of radiotherapy altogether based on a patient’s prognosis or goals of care.
- Strongly agree
- Somewhat agree
- Neither agree nor disagree
- Somewhat disagree
- Strongly disagree
- In the past 3 months, I have been involved in the care of approximately this many patients with painful bone metastases, tumor-related bleeding, or tumor-related compressive/obstructive symptoms.
- None
- 1–5
- 6–10
- 11–15
- >16
- In the past 3 months, I have referred approximately this many patients to radiation oncology for possible palliative radiotherapy.
- None
- 1–5
- 6–10
- 11–15
- >16
Acknowledgments
We thank Drs. Daniel Seible, Andrew Bruggeman, and Kyle Edmonds for their contributions to the course.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was certified as except from full Institutional Review Board and Ethics review as it was determined to not qualify as human subjects research (#180609QI). All participants gave informed consent prior to taking part in this study.
References
- Jones JA, Lutz ST, Chow E, et al. Palliative radiotherapy at the end of life: a critical review. CA Cancer J Clin 2014;64:296-310. [Crossref] [PubMed]
- McDonald R, Chow E, Rowbottom L, et al. Quality of life after palliative radiotherapy in bone metastases: a literature review. J Bone Oncol 2014;4:24-31. [Crossref] [PubMed]
- Spencer K, Parrish R, Barton R, et al. Palliative radiotherapy. BMJ 2018;360:k821. [Crossref] [PubMed]
- Lutz ST, Jones J, Chow E. Role of radiation therapy in palliative care of the patient with cancer. J Clin Oncol 2014;32:2913-9. [Crossref] [PubMed]
- Murphy JD, Nelson LM, Chang DT, et al. Patterns of care in palliative radiotherapy: a population-based study. J Oncol Pract 2013;9:e220-7. [Crossref] [PubMed]
- Lutz S, Spence C, Chow E, et al. Survey on use of palliative radiotherapy in hospice care. J Clin Oncol 2004;22:3581-6. [Crossref] [PubMed]
- Mackillop WJ, Kong W. Estimating the need for palliative radiation therapy: a benchmarking approach. Int J Radiat Oncol Biol Phys 2016;94:51-9. [Crossref] [PubMed]
- McCloskey SA, Tao ML, Rose CM, et al. National Survey of Perspectives of Palliative Radiation Therapy: Role, Barriers, and Needs. Cancer J 2007;13:130-7. [Crossref] [PubMed]
- Samant RS, Fitzgibbon E, Meng J, et al. Family physicians’ perspectives regarding palliative radiotherapy. Radiother Oncol 2006;78:101-6. [Crossref] [PubMed]
- Samant RS, Fitzgibbon E, Meng J, et al. Barriers to palliative radiotherapy referral: a Canadian perspective. Acta Oncol 2007;46:659-63. [Crossref] [PubMed]
- Livergant J, Howard M, Klein J. Barriers to referral for palliative radiotherapy by physicians: a systematic review. Clin Oncol (R Coll Radiol) 2019;31:e75-84. [Crossref] [PubMed]
- Olson RA, Lengoc S, Tyldesley S, et al. Relationships between family physicians' referral for palliative radiotherapy, knowledge of indications for radiotherapy, and prior training: a survey of rural and urban family physicians. Radiat Oncol 2012;7:73. [Crossref] [PubMed]
- Morris L, Gorayski R, Turner S. Targeting general practitioners: prospective outcomes of a national education program in radiation oncology. J Med Imaging Radiat Oncol 2018;62:270-5. [Crossref] [PubMed]
- Shaverdian N, Yoo SM, Cook R, et al. Gaps in radiation therapy awareness: results from an educational multi-institutional survey of US internal medicine residents. Int J Radiat Oncol Biol Phys 2017;98:1153-61. [Crossref] [PubMed]
- Tucker TL, Samant RS, Fitzgibbon EJ. Knowledge and utilization of palliative radiotherapy by pediatric oncologists. Curr Oncol 2010;17:48-55. [Crossref] [PubMed]
- Barnes EA, Parliament M, Hanson J, et al. Palliative radiotherapy for patients with bone metastases: survey of primary care physicians. Radiother Oncol 2003;67:221-223. [Crossref] [PubMed]
- Lutz S, Korytko T, Nguyen J, et al. Palliative radiotherapy: when is it worth it and when is it not? Cancer J 2010;16:473-82. [Crossref] [PubMed]
- Jarosek SL, Virnig BA, Feldman R. Palliative radiotherapy in Medicare-certified freestanding hospices. J Pain Symptom Manage 2009;37:780-7. [Crossref] [PubMed]
- Connor SR, Tecca M. Measuring hospice care: the national hospice and palliative care organization national hospice data set. J Pain Symptom Manage 2004;28:316-28. [Crossref] [PubMed]
- Dharmarajan KV, Rich SE, Johnstone CA, et al. Top 10 tips palliative care clinicians should know about radiation oncology. J Palliat Med 2018;21:383-8. [Crossref] [PubMed]


