
Hypnosis, anesthesia, pain management, and preparation for medical procedures
History
Hypnosis has long had a role in anesthesiology and pain management. James Esdaile, a Scottish surgeon, utilized hypnosis (then known as “Mesmerism”) in hospitals in India, and performed 261 painless surgeries using hypnosis, described in his book, Mesmerism in India, and its Practical Application in Surgery and Medicine (1). The introduction of chloroform and ether into medical practice in India in 1848 reduced the impact of Esdaile’s discoveries. Nevertheless, hypnosis continued to be used as sole anesthetic and in combination with ether and chloroform. In 1906, Magaw reported on 14,000 surgeries completed at the Mayo Clinic, utilizing a combination of hypnosis and chemical anesthesia (2).
Since the time of Esdaile, hypnosis has been applied widely for pain relief and to facilitate patient cooperation in medical procedures.
Hypnosis in obstetrics
Ralph August applied clinical hypnosis to facilitate delivery of 295 babies, in a clinical series from 1957 to 1958. In 94% of the cases, hypnosis was the sole form of anesthesia. In the remaining 6% of cases, hypnotic anesthesia was not adequate, and was supplemented with local or general anesthesia. August reported on his methods and the results, emphasizing the decreased anesthetic hazard to mother and infant, and the enhanced rapport between patient and physician (3,4). More recently, Werner et al. (5,6) conducted a randomized controlled trial (RCT) with 1,222 first time mothers, and those women in the group receiving brief self-hypnosis training reported a better experience of childbirth. There were no differences across groups in duration of labor, but the women in the hypnosis required fewer emergency C-sections.
Hypnosis in dentistry
The first documented application of hypnosis in dentistry was a dental extraction under hypnotic anesthesia, reported in 1829 (7). By 1900, hypnosis was commonly used by dentists for managing dental patients’ fears and pain. Today, hypnosis is widely used by dentists to effectively moderate fears of dental procedures, excessive gag reflex, treatment of orofacial pain conditions, moderating bleeding and salivary flow, and managing procedural pain (8,9). Hypnotic strategies such as distraction, re-framing, and imagery are also useful in managing pediatric patients (10).
Hypnosis for acute pain
In 2010, The American Psychological Association published Clinical Hypnosis for Pain Control by David Patterson (11). In this book Patterson presented a table of 21 controlled hypnosis studies (18 randomized) with acute pain disorders. These studies included the treatment of burn wounds and debridement pain, bone marrow aspiration pain, labor pain, pain following chemotherapy for cancer, pain during angioplasty, pain during plastic surgery, pain related to large core needle biopsies of the breast and multiple other surgical pain situations. The outcome of these studies showed that in all cases hypnosis was at least equal to the existing standard of care and in the majority of studies hypnosis proved more beneficial than the standard of care or other treatment controls which included attention control, relaxation, emotional support, medication (Lorazepam), cognitive behavioral therapy (CBT), deep breathing and non-directed play (for children).
Kendrick et al. (12) completed a similar review of RCTs related to surgical procedural pain. Their results were consistent with the Patterson findings. The authors observed that: “Results from the 29 RCTs meeting inclusion criteria suggest that hypnosis decreases pain compared to standard care and attention control groups and that it is at least as effective as comparable adjunct psychological or behavioral therapies” (p. 75).
While the use of hypnosis or trance-like states for pain relief has been documented for hundreds of years (13), the modern era of hypnosis for pain management was energized by a statement from the NIH Consensus Development Program (14) that “The evidence supporting the effectiveness of hypnosis in alleviating chronic pain associated with cancer seems strong” and by books such as Hypnosis in the Relief of Pain by Ernest Hilgard and Josephine Hilgard (15) and Hypnosis and Suggestion in the Treatment of Pain by Joseph Barber (16). More recently this focus has been maintained by Mark Jensen’s Hypnosis for Chronic Pain Management (17).
Hypnosis for chronic pain
Similar to his table related to acute pain, Patterson (11) presented a table related to chronic pain that included 14 controlled studies of hypnosis (12 randomized), in chronic conditions including fibromyalgia, headaches, cancer-related pain, back pain, and irritable bowel syndrome (IBS)-related pain. Again, all studies found that hypnosis was equal to or better than standard care treatments which included group support, biofeedback, medication, relaxation, Autogenic training, attention control and CBT. In a video interview (18), Michael Yapko pointed out that the salient question isn’t whether hypnosis is better than other treatments, but rather whether the addition of hypnosis to existing treatment enhanced the treatment effects. In his understanding of the literature, “the answer is clearly yes!” This approach is described by Willmarth, Davis, and Fitzgerald (19) who for over 30 years have combined traditional medical interventions offered by anesthesiologists with the treatment of physical therapists, social workers, and psychologists who offer group therapy, hypnosis, biofeedback, and individual psychotherapy for patients suffering from chronic pain conditions.
Hypnosis for pre-surgical preparation
The use of hypnosis for anesthesia during surgery has already been mentioned. Hypnosis has proven to be one of the most powerful tools in enhancing surgical recovery. Montgomery et al. (20) reviewed the evidence on hypnosis as an adjunctive approach for surgery patients: “Patients receive standard surgical and anesthesia care according to protocol but with hypnosis added to the treatment package” (p. 1,639). Montgomery et al. reviewed 20 well-controlled research studies, using meta-analytic techniques, and concluded that hypnosis is an effective adjunctive treatment for patients undergoing surgery.
The meta-analysis showed a broad beneficial impact of hypnosis with surgical patients, across outcome categories. Subjective measures such as anxiety and pain, objective measures such as analgesia use, physiological measures, recovery time, and treatment time, all showed comparable beneficial outcomes for patients in the groups receiving hypnosis. The patients in the hypnosis groups showed better medical and psychological outcomes than 89% of the patients who did not receive hypnosis. Later research by Montgomery et al. (21) showed that not only could hypnosis reduce patients suffering, enhance healing, and optimize recovery time, but that the savings to the hospital were substantial, mainly in reduced time in surgery.
Hypnotic ability or hypnotizability
Not all human beings respond equally well to hypnotic intervention. The researcher Ernest Hilgard (22) defined hypnotic susceptibility as an “ability in which men differ, just as they differ in intelligence or athletic skill” (p. 65). Hypnotic ability is a relatively stable and measurable trait over the human lifetime, somewhat normally distributed. One landmark study administered a standard test of hypnotic susceptibility at baseline and after 10, 15, and 25 years. The test/re-test correlations were 0.64, 0.82, and 0.71 over these extended time periods (23). Morgan (24) conducted a study of hypnotic susceptibility in monozygotic and dizygotic twins and calculated a heritability index of 0.64.
The original tests of hypnotic susceptibility included the Stanford Hypnotic Susceptibility Scale and the Harvard Group Scale of Hypnotic Susceptibility and typically required a full hour for administration. More recently the Elkins Hypnotizability Scale (25) was developed for brief, efficient administration in clinical and research settings, with relatively strong correlations with the older and longer measures.
For medical applications of hypnosis, it is important to remember that some patients (approximately 20%) may respond poorly to hypnosis and may therefore require alternative interventions. Some authors claim that with a well-trained practitioner, adequate preparations to enhance hypnotic ability, and an individualized hypnotic approach, almost all human beings can benefit from hypnosis. However, Lynn, Laurence, and Kirsch (26) concluded that even after credible interventions to enhance suggestibility, a sizable minority of individuals remain who do not respond to hypnosis or suggestion. They hypothesized that these “low-suggestible individuals lack key hard-wired abilities compared with highly suggestible participants” (p. 323).
Fortunately, the majority of patients display medium to high hypnotic ability, and for this larger population therapeutic outcomes for hypnosis are comparable to traditional medical interventions. Since increasing numbers of patients are inquiring about non-pharmacological approaches to healthcare, hypnosis provides a practical alternative.
The place of hypnosis in clinical medicine and dentistry
The patient seeking medical or dental care for a broad range of conditions may benefit best from an integrative healthcare program that includes adjunctive hypnosis as an integral component within the total treatment package.
Evidence-based hypnotic interventions
For this to happen, it is critical that the patient’s complaint be one for which there is a strong research base supporting the value of hypnotic treatment. There is good research support for the application of hypnosis for anxiety disorders, depression (including major depression), post-traumatic stress disorder, stress management, sleep disorders, smoking cessation, weight management and eating disorders, and the addictions. There is also strong research support for the use of hypnosis for acute and chronic pain, IBS, colitis, diabetes mellitus, hypertension, skin conditions including psoriasis, chemotherapy induced nausea, and pediatric problems such as anxiety, school phobia, and recurrent abdominal pain (27,28).
Competent, well-trained hypnotic practitioners with competence in the area of patient’s complaint
It is essential that the hypnotic practitioner is a licensed healthcare or mental healthcare professional, with state-of-the-art training in clinical hypnosis, and adequate knowledge and experience in the areas of the patient’s presenting problems and diagnoses. Licensed psychologists, physicians, physical therapists, and dentists all are eligible for training in clinical hypnosis and must apply hypnosis in the areas of their licensure and expertise.
Interprofessional and collaborative care
Integrative medicine is increasingly interprofessional and collaborative in nature. The interprofessional model suggests that coordination, communication, and a team approach enhance the quality and safety of patient care (29). The hypnotically trained social worker may then provide therapeutic support and hypnotic pain management while the oncologist provides medical supervision, chemotherapy and radiation. Hypnotically trained nurses and health coaches can master and provide the protocol for pre-surgical hypnotic training for patients, working under supervision and in close communication with surgical and anesthesia teams, and must refer any serious mental health symptoms to consulting psychologists or physicians.
Certification by a professional hypnosis organization for licensed healthcare providers is the gold standard for trustworthy professionals
Determining which “certified hypnotherapists” should be trusted is often confusing. There are many lay hypnosis organizations providing “certificates” and certification based on minimal training to lay persons without regard to education or licensure in healthcare. Steve Eichel demonstrated the danger of such lay hypnosis certifications by applying for and receiving hypnosis certification for his cat, Zoe D. Katze, from three lay hypnotherapy programs, and gained membership for Zoe in a fourth such organization (30).
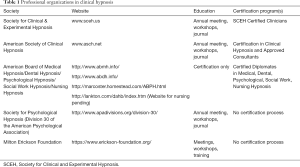
Certification by one of the recognized professional hypnosis associations, limited to licensed healthcare professionals in clinical hypnosis, provides assurance for the patient and the referring physician that the provider has a foundation of training and knowledge. At present, there are five national professional organizations providing reliable education and training in hypnosis for licensed healthcare professionals. The Society for Clinical and Experimental Hypnosis (SCEH) is dedicated to the promotion of evidence-based hypnotic applications, integrating research and clinical practice for physicians, dentists, and mental health professionals. The American Society for Clinical Hypnosis (ASCH) focuses on providing training to licensed healthcare providers. The Society for Psychological Hypnosis is a Division of the American Psychological Association (APA, Div. 30) and provides training and education in hypnosis for psychologists. The American Boards of Hypnosis concentrate on a high-quality certification in hypnosis for physicians, dentists, psychologists, social workers, and most recently nurses. The Milton Erickson Foundation promotes the approach of the gifted hypnotherapist Milton Erickson and provides hypnosis training and education to both medical and mental health professionals. Table 1 shows these professional organizations, their websites, and whether they sponsor certification programs.
Full table
Conclusions
In summary, hypnosis is most helpful and effective for patients in healthcare, dentistry, and mental healthcare, when evidence-based hypnosis protocols are followed, based on current research. Referrals are best made to licensed healthcare professionals, who practice in close communication and coordination with other involved healthcare professionals, and whose training and competence are demonstrated by certification through one of the professional hypnosis organizations shown in Table 1.
Acknowledgments
The authors would like to acknowledge Saybrook University for its ongoing support for education and training in clinical and experimental hypnosis.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Esdaile J. Mesmerism in India, and its Practical Application in Surgery and Medicine. Silus Andrus, Hartford, CT, 1850. (Original publication date 1846).
- Magaw A. A review of over 14 thousand surgical anesthesias. Surg Gynecol Obstet 1906;3:795-7.
- August RV. The obstetrician and hypnosis. Am J Clin Hypn 1959;1:151-4. [Crossref] [PubMed]
- August RV. Hypnosis in obstetrics: Obstetric hypnoanesthesia. New York: McGraw-Hill, 1961.
- Werner A, Uldbjerg N, Zachariae R, et al. Antenatal hypnosis training and childbirth experience: a randomized controlled trial. Birth 2013;40:272-80. [Crossref] [PubMed]
- Werner A, Uldbjerg N, Zachariae R, et al. Effect of self-hypnosis on duration of labor and maternal and neonatal outcomes: a randomized controlled trial. Acta Obstet Gynecol Scand 2013;92:816-23. [Crossref] [PubMed]
- Allison N. Hypnosis in modern dentistry: Challenging misconceptions. FDJ 2015;6:172-5. [Crossref]
- Armfield JM, Heaton LJ. Management of fear and anxiety in the dental clinic: a review. Aust Dent J 2013;58:390-407. [Crossref] [PubMed]
- Facco E, Zanette G, Casiglia E. The role of hypnotherapy in dentistry. SAAD Dig 2014;30:3-6. [PubMed]
- Peretz B, Bercovich R, Blumer S. Using elements of hypnosis prior to or during pediatric dental treatment. Pediatr Dent 2013;35:33-6. [PubMed]
- Patterson DR. Clinical Hypnosis for Pain Control. Washington, DC: American Psychological Association, 2010.
- Kendrick C, Sliwinski J, Yu Y, et al. Hypnosis for Acute Procedural Pain: A Critical Review. Int J Clin Exp Hypn 2016;64:75-115. [Crossref] [PubMed]
- Tinterow MM. Foundations of Hypnosis: From Mesmer to Freud. Springfield, IL: Charles C. Thomas Publisher, 1970.
- National Institutes Health. Integration of behavioral and relaxation approaches into the treatment of chronic pain and insomnia. NIH Technology Assessment Statement 1995, 1-34. Available online: https://consensus.nih.gov/1995/1995behaviorrelaxpaininsomniata017html.htm
- Hilgard ER, Hilgard JR. Hypnosis in the Relief of Pain. Los Altos, CA: William Kaufmann, 1975.
- Barber J. Hypnosis and Suggestion in the Treatment of Pain. New York: W.W. Norton and Company, 1996.
- Jensen M. Hypnosis for Chronic Pain Management. New York: Oxford, 2011.
- Willmarth E. The Willmarth Hypnosis Interviews: Michael Yapko, PhD, 2012. Available online: https://www.youtube.com/watch?v=I6wMjKWHakg
- Willmarth E, Davis F, Fitzgerald K. Biofeedback and integrative medicine in the pain clinic setting. Biofeedback 2014;42:111-4. [Crossref]
- Montgomery GH, David D, Winkel G, et al. The effectiveness of adjunctive hypnosis with surgical patients: a meta-analysis. Anesth Analg 2002;94:1639-45. table of contents. [PubMed]
- Montgomery GH, Bovbjerg DH, Schnur JB, et al. A randomized clinical trial of a brief hypnosis intervention to control side effects in breast surgery patients. J Natl Cancer Inst 2007;99:1304-12. [Crossref] [PubMed]
- Hilgard ER. Hypnotic Susceptibility. New York: Harcourt, Brace, Jovanovich, 1965.
- Piccione C, Hilgard ER, Zimbardo PG. On the degree of stability of measured hypnotizability over a 25-year period. J Pers Soc Psychol 1989;56:289-95. [Crossref] [PubMed]
- Morgan AH. The heritability of hypnotic susceptibility in twins. J Abnorm Psychol 1973;82:55-61. [Crossref] [PubMed]
- Kekecs Z, Bowers J, Johnson A, et al. The Elkins Hypnotizability Scale: Assessment of Reliability and Validity. Int J Clin Exp Hypn 2016;64:285-304. [Crossref] [PubMed]
- Lynn SJ, Laurence JR, Kirsch I. Hypnosis, suggestion, and suggestibility: an integrative model. Am J Clin Hypn 2015;57:314-29. [Crossref] [PubMed]
- Elkins GR. Handbook of Medical and Psychological Hypnosis. New York: Springer, 2017.
- Nash MR, Barnier AJ. The Oxford Handbook of Hypnosis. New York: Oxford University Press, 2008.
- Robert Wood Johnson Foundation. What can be done to encourage more interprofessional collaboration in health care? Health Policy Snapshot Series, 2011. Available online: https://www.rwjf.org/en/library/research/2011/09/what-can-be-done-to-encourage-more-interprofessional-collaborati.html
- Eichel SKD. Credentialing: It may not be the cat’s meow, 2011. Available online: http://www.dreichel.com/articles/dr_zoe.htm


