
A targeted needs assessment to improve referral patterns for palliative radiation therapy
Introduction
Radiation therapy (RT) can effectively palliate a variety of symptoms in patients with cancer, using relatively low doses of radiation that infrequently cause major side effects (1,2). Common indications may include tumor-induced pain, bleeding, obstruction, or neurologic symptoms (3). Unfortunately, palliative RT is either not utilized at all or administered too late for many patients, in large part because delivering treatment depends upon appropriate referrals to radiation oncologists when a patient is symptomatic but still has sufficient life expectancy to benefit from treatment (4-7). Medical oncologists are the most common source of these referrals, since they are frequently following these patients closely as they give systemic therapy. However, physicians from many other specialties also encounter symptomatic patients with cancer in both the outpatient and inpatient setting, and can make direct referrals to radiation oncology. If these physicians also have a baseline understanding of indications for palliative radiation and feel empowered to refer patients, it would help expedite alleviation of their patients’ symptoms and maximize quality of life (5,8). In this study, we surveyed the Society of Palliative Radiation Oncology (SPRO) membership to identify barriers to appropriate referral for palliative RT that they encounter in their practice, and identify specific groups of physicians who the radiation oncologists believed would benefit most from further education on when to refer patients for this important aspect of supportive care.
Methods
After obtaining ethics approval from the West Virginia University institutional review board (expedited protocol number 1901437100), an electronic survey was sent to all 136 members of SPRO. This convenience sample was selected for participation because the investigators felt that they were likely to be more knowledgeable about palliative RT referral patterns than the average radiation oncologist who has less of an interest in this particular patient population. Research Electronic Data Capture (REDCap), a secure web application used to build and manage online surveys and databases, was used to develop and disseminate the surveys. Two emails were sent to the SPRO membership soliciting participation. All responses were received between November 2018 and January 2019. Participation was anonymous, completely voluntary, and no financial incentive was provided.
The survey consisted of five sections. Section one assessed whether patients with newly diagnosed spinal cord compression, brain metastasis, thoracic airway obstruction, esophageal obstruction, and urinary obstruction were more commonly referred first to radiation oncology, the appropriate surgeon/procedure-oriented subspecialist, or both simultaneously at participants’ institutions. Section two assessed in a multiple choice format the perceived most important and second most important barriers to referral for medical oncologists, surgeons, palliative care physicians, and primary care physicians. Section three assessed the perceived frequency of delays in referrals and potential reasons for those delays. Section four assessed the perceived level of understanding of different types of referring physicians of the risks and benefits of palliative RT on a 9-point Likert-type scale (1= not at all knowledgeable, 9= as knowledgeable as a radiation oncologist). Section five collected demographic information about the participants and their institutions. All survey questions and answer choices are shown in Table S1. Descriptive statistics including mean, standard deviation (STD), median, and interquartile range (IQR) were used to summarize the findings.

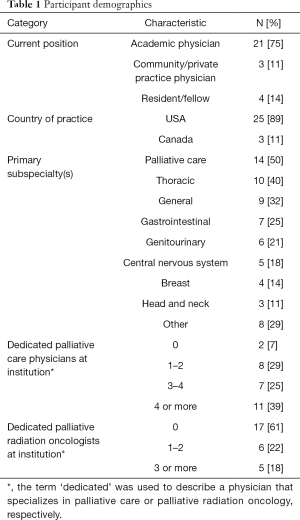
Full table
Results
A total of 28 radiation oncologists responded to the survey (response rate 20.5%). The demographics of these participants are shown in Table 1. Eighty-nine percent of participants had at least one palliative care physician readily available to them at their primary practice location. The majority of participants also had readily available gastroenterology (89%), interventional radiology (86%), pain medicine (82%), spine surgery (82%), thoracic surgery/interventional pulmonology (82%), urology (79%), and neurosurgery (79%).
Full table
Figure 1 shows the perceived order of referrals for five common clinical indications for palliative RT. It was felt that radiation oncology was consulted first or simultaneously with spine surgery or neurosurgery more than 50% of the time for both spinal cord compression and brain metastases, respectively. However, it was felt that radiation oncology was much less likely to be part of the initial consultation for thoracic airway obstruction/bleeding, esophageal obstruction, or urinary obstruction/bleeding, which were more often initially evaluated by thoracic surgery/interventional pulmonology, gastroenterology, and urology, respectively.
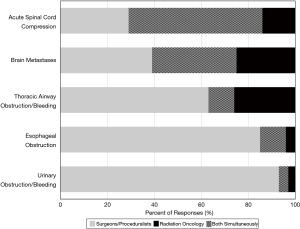
Figure 2 shows participant views of how knowledgeable various medical and surgical subspecialists were about palliative RT. Neurosurgeons, head and neck, thoracic, and gynecologic surgeons were felt to be most knowledgeable among the surgical subspecialists, whereas palliative care and medical oncology were felt to be most knowledgeable among the medical subspecialists. Of note, primary care, geriatric medicine, and emergency medicine were considered to be among the least knowledgeable.
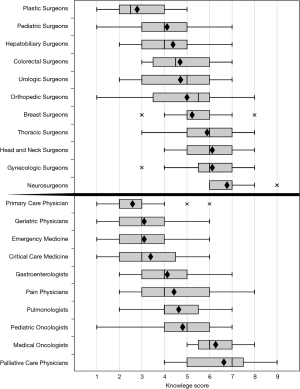
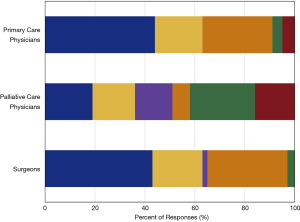
Figure 3 summarizes participants’ perceptions of the two most common barriers to referrals for surgeons, palliative care physicians, and primary care physicians. The most common barriers to referral for primary care physicians and surgeons was thought to be a lack of knowledge about the benefit of palliative RT, and that it was the responsibility of the medical oncologist to do it. The palliative care physicians were thought to be more concerned with patient convenience, performance status, and other factors like cost, delay in hospice enrollment, and reimbursement concerns if a patient is on hospice. For medical oncologists (not pictured in the figure), participants felt that the greatest barriers were potential interference with systemic therapy (33%), lack of knowledge about the benefit of palliative RT (28%), and toxicity concerns (22%).
On average, participants felt that referrals for palliative RT were inappropriately delayed 46.5% (STD 20.2%) of the time. Similarly, waiting for tissue confirmation of malignancy was perceived to delay radiation oncology consultation for symptom palliation on average 51.5% (STD 27.8%) of the time when no prior biopsy had been obtained. Additional reasons for delayed referrals cited by participants included a cumbersome triage system between the different oncologists, other interventional services getting the referral first, referring physicians lacking an understanding of how imaging findings correlate with symptoms, concern that RT will delay systemic therapy by taking too long to start or finish, and an over-optimism that systemic therapy will work quickly enough or sufficiently enough to obviate the need for RT.
Discussion
In this study we have collected information from a group of radiation oncologists with an interest in palliative care, to identify perceived barriers hindering their ability to deliver timely and effective palliative RT at their institution. We found that nearly half of referrals for palliative RT were thought to be inappropriately delayed, radiation oncology is often a secondary consultation for certain conditions that are common indications for palliative RT, and the most important barriers to referral may vary considerably for different subspecialists. Overall, our data presents a number of hypothesis-generating observations that may help guide approaches to improve referral patterns for palliative RT.
Lack of knowledge about the benefits of palliative radiation was cited by 51% of participants as the most important barrier to referral across all categories of physicians that were asked about in this study. As such, education should be at the forefront of interventions to improve referral patterns. Targeting educational efforts towards physicians at the initial triage point in the outpatient and inpatient settings may be most effective, particularly as primary care, geriatric medicine, and emergency medicine, who are highly likely to see patients with cancer in some capacity, were considered to be among the least knowledgeable about palliative RT in our survey. An important message to these groups, as well as medical oncologists, may be that a referral is only a request for an opinion rather than an order for treatment, that early referral is encouraged, and ultimately the decision if, and when, to offer RT would involve shared decision-making between all of the oncologists involved. Hopefully this approach would also decrease reliance on medical oncologists to make all cancer-oriented referrals. Educational initiatives among primary care providers are likely to increase referrals for palliative RT in the USA, as has been demonstrated in two prior Canadian studies (4,9). Finally, another important aspect of education is to accurately and realistically describe short- and long-term toxicities of radiation, so that other physicians can understand that although curative-intent radiation can cause late toxicities like bleeding, obstruction, or pain, radiation is also very good at alleviating these same symptoms in the palliative setting.
Educational initiatives would probably translate not only into more referrals, but perhaps more importantly earlier referrals. Ideally, patients would be treated before symptoms are so severe that they cannot tolerate the procedural aspects of delivering radiation (e.g., lying flat or wearing a head mask), and when patients still have sufficient lifespan to fully benefit from the radiation. Murphy et al. showed that in the USA approximately one-fifth of cancer patients died within 2 weeks of receiving palliative RT, and one-third within one month of it, whereas Gripp et al. showed that among patients who died within 2 weeks of receiving palliative RT, only 26% had stable or improved symptoms from the radiation (5,7). Physicians are notorious for overestimating survival towards the end of life, but regardless, the earlier that radiation is delivered, the increased likelihood patients are alive long enough to benefit from it (10). Earlier referral has the additional benefit of potentially sparing patients invasive procedures that may be less effective or have more potential for complications than RT (11-13).
Another initiative that is likely to improve referral patterns for palliative RT is for radiation oncologists to be more enthusiastic about using shorter courses of radiation when possible in order to minimize time off systemic therapy and any inconvenience for patients coming for daily treatment. Guadagnolo et al. demonstrated that in the USA fewer than 10% of patients received single fraction palliative RT for any indication near the end of life, despite its comparable efficacy in many cases (14-16). Considering institutional improvements for how patients are triaged, and engaging in multidisciplinary clinics whenever possible, is also likely to streamline the referral process.
The primary limitation of this study is selection bias, which may have affected our findings due to the relatively low response rate and convenience sample of potential participants who had a baseline interest in palliative care. On the other hand, because this population of physicians is actively engaged in providing palliative RT in their practice, our data is probably more accurate than if we were to have surveyed the general radiation oncology community at large. It is likely that our participants have somewhat more robust palliative radiation oncology programs than the average community radiation oncologist, and our findings may actually underestimate the extent of the problems with palliative RT referral identified. Another potential limitation is that we did not survey the other specialists themselves about their perspective on palliative radiotherapy, which may have provided some difference in outcomes compared to the radiation oncologists’ perceptions of their colleagues. Despite these flaws, we believe that our findings do support greater attention to initiatives to improve palliative RT referral patterns in the future. Ideally such initiatives would be investigated in clinical trials to assess the clinical benefit of earlier radiation oncology referral for palliative RT.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. After obtaining ethics approval from the West Virginia University institutional review board (expedited protocol number 1901437100).
References
- Lutz S, Korytko T, Nguyen J, et al. Palliative radiotherapy: when is it worth it and when is it not? Cancer J 2010;16:473-82. [Crossref] [PubMed]
- Jones JA, Lutz ST, Chow E, et al. Palliative radiotherapy at the end of life: a critical review. CA Cancer J Clin 2014;64:296-310. [Crossref] [PubMed]
- Ashby M. The role of radiotherapy in palliative care. J Pain Symptom Manage 1991;6:380-8. [Crossref] [PubMed]
- Fairchild A, Ghosh S, Baker J. Patterns of referral and knowledge of palliative radiotherapy in Alberta. Can Fam Physician 2012;58:e113-22. [PubMed]
- Murphy JD, Nelson LM, Chang DT, et al. Patterns of care in palliative radiotherapy: a population-based study. J Oncol Pract 2013;9:e220-7. [Crossref] [PubMed]
- Wong J, Xu B, Yeung HN, et al. Age disparity in palliative radiation therapy among patients with advanced cancer. Int J Radiat Oncol Biol Phys 2014;90:224-30. [Crossref] [PubMed]
- Gripp S, Mjartan S, Boelke E, et al. Palliative radiotherapy tailored to life expectancy in end-stage cancer patients: reality or myth? Cancer 2010;116:3251-6. [Crossref] [PubMed]
- Lloyd S, Dosoretz AP, Yu JB, et al. Academic and Resident Radiation Oncologists' Attitudes and Intentions Regarding Radiation Therapy near the End of Life. Am J Clin Oncol 2016;39:85-9. [Crossref] [PubMed]
- Olson RA, Lengoc S, Tyldesley S, et al. Relationships between family physicians' referral for palliative radiotherapy, knowledge of indications for radiotherapy, and prior training: a survey of rural and urban family physicians. Radiat Oncol 2012;7:73. [Crossref] [PubMed]
- Glare P, Virik K, Jones M, et al. A systematic review of physicians' survival predictions in terminally ill cancer patients. BMJ 2003;327:195-8. [Crossref] [PubMed]
- Francis SR, Orton A, Thorpe C, et al. Toxicity and Outcomes in Patients With and Without Esophageal Stents in Locally Advanced Esophageal Cancer. Int J Radiat Oncol Biol Phys 2017;99:884-94. [Crossref] [PubMed]
- Moeller B, Balagamwala EH, Chen A, et al. Palliative thoracic radiation therapy for non-small cell lung cancer: 2018 Update of an American Society for Radiation Oncology (ASTRO) Evidence-Based Guideline. Pract Radiat Oncol 2018;8:245-50. [Crossref] [PubMed]
- Tsao MN, Rades D, Wirth A, et al. Radiotherapeutic and surgical management for newly diagnosed brain metastasis(es): An American Society for Radiation Oncology evidence-based guideline. Pract Radiat Oncol 2012;2:210-25. [Crossref] [PubMed]
- Guadagnolo BA, Liao KP, Elting L, et al. Use of radiation therapy in the last 30 days of life among a large population-based cohort of elderly patients in the United States. J Clin Oncol 2013;31:80-7. [Crossref] [PubMed]
- Lutz S, Berk L, Chang E, et al. Palliative radiotherapy for bone metastases: an ASTRO evidence-based guideline. Int J Radiat Oncol Biol Phys 2011;79:965-76. [Crossref] [PubMed]
- Maranzano E, Trippa F, Casale M, et al. 8Gy single-dose radiotherapy is effective in metastatic spinal cord compression: results of a phase III randomized multicentre Italian trial. Radiother Oncol 2009;93:174-9. [Crossref] [PubMed]


