Analysis of risk factors for implantable venous access port catheter fracture with internal jugular vein
Introduction
By providing a safe and reliable reserved venous access for patients undergoing breast cancer surgery and requiring long-term chemotherapy, given its safety, simplicity, economy and low impact on daily life, implantable venous access port (IVAP) technique has been gradually recognized by patients and clinicians. However, the complications induced by in vivo IVAP catheter fracture limit the use of this technique (1), since the fractured catheter may travel to the vena cava, right atrium, right ventricle or pulmonary artery along with the blood flow, leading to pulmonary artery embolism, thrombosis, vascular tear, arrhythmia, other serious complications, or even death in severe cases (2). In vivo IVAP catheter fracture is affected by various factors. Long-term stress, neck movement, and compression by backpacks and necklaces are considered potential causes of totally implantable venous access port (TIVAP) catheter fracture (3), which have been examined by few large-scale studies. Dynamic observation and monitoring of the image data during follow-up are critical for predicting the risk of breaking port, and some cases were first discovered in the chest, thereby avoiding serious consequences. Based on the follow-up of the 3,102 patients who underwent IVAP implantation via the internal jugular vein (IJV), this study aimed to explore the factors associated with in vivo IVAP catheter fracture, establish the importance of imaging in the safe use of venous port, and thereby provide a basis and precautionary measures for the safe clinical use of IVAP.
Methods
A retrospective analysis was performed on 3,102 female breast cancer patients, who were admitted to the hospital between November 2013 and March 2016 for IVAP implantation via IJV. All patients had undergone modified radical mastectomy or breast-conserving surgery plus full axillary lymph node dissection. In these cases, 1,634 cases suffered from left breast cancer, while 1,468 cases suffered from right breast cancer. Their clinical data was well documented, and all patients had accepted routine review at our hospital to regularly check the IVAP condition. The age of the patients ranged from 20 to 85 years, with the average age of 53.2. All subjects have undergone IVAP catheter implantation via the contralateral IJV, including 1,468 cases of left implantation and 1,634 cases of right implantation.
All IVAP implantation surgeries were conducted in the sterile operating room using 7 or 8 F IVAP equipped with three-way valve-type catheter (C. R. Bard, Inc., USA). All patients had signed informed consent form before surgery. Under local infiltration anesthesia, the puncture needle was inserted into the IJV, followed by IVAP implantation. If venous blood return was observed pumping back, bedside radiography was performed to confirm whether the catheter tip was located at the junction of superior vena cava and right atrium. The port cave was established in the lateral part below the clavicle and tunnel guide was used to build a subcutaneous tunnel from the port cave to the puncture point for catheter traveling. The catheter was connected to IVAP exit and then locked, followed by incision suturing and bandaging fixation using aseptic auxiliary materials. After the IVAP implantation completed, chest X-ray plain film was used to re-confirm the location of catheter tip. Swelling, errhysis, hematoma, infection and other complications were closely monitored at the implantation site. The stitches were removed after a week and the skin healing progress at incision site was assessed. Patients with implanted IVAP regularly visited the hospital for chest radiograph review to assess the catheter condition.
All patients were followed-up via outpatient visit or telephone until November 2016, for 8–37 months. The chest radiographs were reviewed every 3 months. Their posteroanterior chest radiographs and related clinical information were acquired via the hospital PACS network. Three senior physicians experienced in imaging diagnosis summarized the imaging information after IVAP implantation. The study protocol and consent form were approved by the hospital institutional review board.
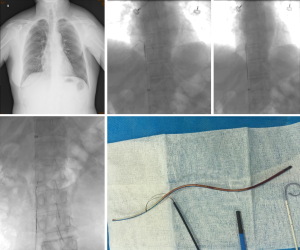
There are four observation indicators: (I) IVAP implantation site and location of catheter tip; (II) intravascular outer catheter angle, which was formed by the catheter turnover at the inlet of jugular vessel because IVAP was implanted under the skin of the upper chest wall based on the IJV puncture approach (Figure 1A). This angle is created by the trajectory of the needle to puncture the IJV and the course of the subcutaneous tunnel. PACS software was used to analyze and record the degree of angle, and multiple measurements were represented by the mean; (III) the detailed clinical data and port characteristics of patients reporting in vivo IVAP catheter fracture; (IV) patient’s age, occupation, living habits, IVAP duration and other clinical data.

The data was analyzed by SPSS 21.0 statistics software. The difference between the venous port catheter fracture group and the patient’s clinical feature group was analyzed by variance analysis, and the risk factors of catheter rupture were analyzed by multivariate logistics regression analysis, with P<0.05 being identified as statistically significant.
Results
The influence of age, occupation and duration of IVAP on the rupture of IVAP catheter
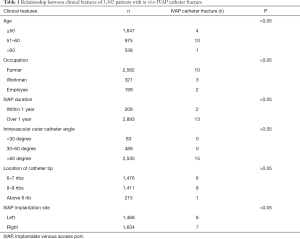
According to the 3,102 patients included in this study, in vivo IVAP catheter fracture was observed in 15 females (0.48%). Fracture site showed on the inlet of IJV (n=12), the junction of IVAP (n=2) and the catheter tip (n=1). IVAP implantation site on the left side (n=8) and seven cases on the right side. The 15 cases were farmers (n=10), workers (n=3) and employees (n=2). All intravascular outer catheter angle showed more than 65 degrees and IVAP duration of 13 cases was over 1 year. Among the 15 patients, 13 cases with intravascular catheter fracture underwent DSA-guided interventional capture to remove the catheter (Table 1).
Full table
Statistical analyses showed that the difference in cases suffering from in vivo IVAP catheter fracture was statistically significant between the different groups in terms of clinical features including age, occupation and IVAP duration (P<0.05), but not significant in intravascular outer catheter angle, location of catheter tip and IVAP implantation site (P>0.05).
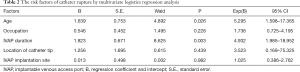
Logistics multivariate analysis showed that age (P=0.026, OR: 5.295) and IVAP duration (P=0.003, OR: 4.932) was an independent risk factor for IVAP catheter fracture (Table 2).
Full table
The clinical symptoms of patients with catheter fracture
There are distending pain surrounding the IVAP injection in three cases, poor blood return in five cases including one case of pumping back pale red blood, and no obvious clinical symptoms in the remaining seven cases that were identified upon review.
Imaging characteristics of fractured catheter
Angiography showed (I) local overflow of contrast agent through the fracture site in two cases with fracture at the junction of IVAP base (Figure 1B); (II) local exosmosis of contrast agent to neck subcutaneous tissue in two cases with incomplete fracture around the intravascular outer angle, where the distal end of the catheter was disconnected and entered the superior vena cava during the catheter removal in vitro; and the chest plain film review of 11 cases showed (III) fractured catheter was disconnected from the IVAP and travelled to the superior vena cava, inferior vena cava, right atrium or partial pulmonary artery along with the blood flow (Figure 1C).
Discussion
As a closed venous access device that can be completely implanted in the body, IVAP has been gradually recognized by patients requiring multiple chemotherapy sessions due to breast cancer, lymphoma or other tumors, with the advantages of free activities during the intermission of chemotherapy, no impact on patient’s self-image, and significant improvement in quality of life (4). However, this device still not easy to guarantee every patient without risk. Some complications may occur, such as intra-catheter thrombosis, formation of fibrin sheath, and in vivo catheter fracture (5,6). Among the 3,102 patients included in this study, in vivo IVAP catheter fracture was observed in 15 cases with the incidence of about 0.48%, which was consistent with previous reports (1). The fractured IVAP catheter may induce serious complications. The fractured catheter in 13 cases was captured by our DSA (Figure 2) with the success rate of 100% (7), and the subsequent follow-up confirmed its safety and effectiveness. However, this disorder led to adverse economic and psychological effects on the patients. Therefore, it is critical to analyze the factors associated with IVAP catheter fracture and ensure early prevention.
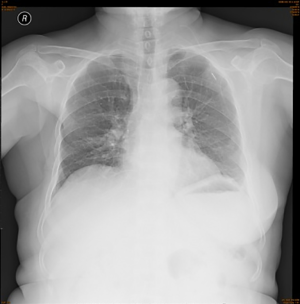
The association of IVAP duration with catheter fracture
According to the involved subjects, two cases of in vivo catheter fracture were reported in 2016, nine cases in 2016, including five cases with IVAP duration of more than 2 years. Statistical analysis demonstrated that the in vivo IVAP catheter fracture was associated with IVAP duration. Although the service span of IVAP may be up to 4.5 years according to the operation guidelines and instructions of C. R. Bard, Inc., the extension of IVAP duration may accelerate catheter aging and lead to stabilizer precipitation from the catheter body. Consequently, the aged catheter and reduced pull-resistant capacity contribute to the risk of catheter fracture (Figure 3). This suggests that clinicians should establish a database of IVAP patients in order to guide and monitor them thoroughly.
The association of IVAP patient’s age and living habits with catheter fracture
IVAP catheter fracture mainly occurs in patients aged 51–60 years, who serve as the core member of the family and are exposed to intensive daily physical activities. Through follow-up and detailed inquiry of daily routine in nine patients with IVAP catheter fracture, eight cases reported the burden of major household duties, such as holding the baby for long time, washing clothes with a washboard and caring for family’s diet, while one case reported a passion for sports like badminton, which often involved the upper limb on the side carrying IVAP. Four cases were keen on square dancing and often did sweeping actions with the neck and upper limbs. Since both the IVAP injection base and intravenous outer catheter were buried in the subcutaneous tissue, the patient's unawareness of IVAP during the intermission and intensive constant repetitions of a single action would squeeze and bend the same part of the catheter, which increase the incidence of catheter damage or fracture. Therefore, in order to prevent catheter fracture at the bending or folding stage, it is necessary to provide health education to patients undergoing IVAP implantation and inform them that violent and frequent movements should be avoided in the ipsilateral neck and shoulder. Moreover, regular chest X-ray should be reviewed to identify abnormal signs at the earliest clinical stage and thus ensure the safety of IVAP.
The association of intravascular outer catheter angle with catheter fracture
It is reported that placing a TIVAP catheter in the IJV has fewer complications than placing it in the subclavian vein (8). Pinch-off syndrome is a complication specific to catheter implantation via the subclavian vein. With the advancement of knowledge about the pinch-off syndrome (9-12) and improvements in surgical procedures, related reports have demonstrated that puncture via IJV is associated with significantly fewer complications than the traditional puncture via subclavian vein (13). Since we have completely replaced the traditional puncture via subclavian vein by puncture via IJV in the past 3 years, pinch-off syndrome is no longer the primary cause of IVAP catheter fracture in our patients. However, we found that the catheter was fractured at the turnover in the inlet of jugular vessel in 12 cases (12/15), accompanied by cervical soft tissue swelling and limited mobility. Therefore, we thought that after intravenous catheter implantation and port cave establishment, the intravascular outer angle, which was formed due to the turnover in IJV of catheter traveling along the subcutaneous tunnel, might be associated with catheter fracture. In the case of insufficient angle, such as less than 30 degrees, the frequent neck and shoulder activities might contribute to the risk of fracture as a result of repeated bending and friction. By dividing these subjects into different groups according to their degree of angle, a statistical analysis was conducted, which indicated that IVAP catheter fracture was not significantly correlated with the degree of angle. Smaller angles did not cause more fractures. On the contrary, the angle of all 15 cases with catheter fracture was more than 65 degrees. Nevertheless, patients with insufficient angle suffered daily discomfort in cervical activities, so insufficient angles can affect patient’s life quality and may potentially lead to catheter fracture. Although the data from our group exhibited no significant correlation between fracture and catheter turnover angle, the patients who were followed-up with chest X-ray examination were carefully monitored. Our IVAP implantation physicians have modified the procedure upon puncturing through the subcutaneous tunnel, that is, making an incision at 1 cm to the venous puncture point and cutting into the subcutaneous tissue, from which the tunnel guide was pulled out and connected to the IVAP so as to prevent complications induced by insufficient angles.
The association of patient’s occupation with catheter fracture
These 15 patients included 10 farmers, three workers, and two employees. Statistical analysis showed that the fracture probability in farmers was higher than the other two occupations. In addition to housework, female farmers also have to perform heavy farm work, and may repeat a single action within a short time and thereby exert a large load on the neck and upper limbs. Consequently, the same part of in vivo IVAP catheter may be repeatedly bent or folded, which increases the risk of fracture.
The association of IVAP implantation site with catheter fracture
Our group consisted of 1,468 cases of left IVAP implantation (47%) and 1,634 cases of right IVAP implantation (53%). Within the 15 cases in the group reporting catheter fracture, eight cases underwent left implantation and seven cases underwent right implantation. Catheter fracture was not significantly correlated with either IVAP implantation site or the location of the catheter tip.
Our study demonstrated that age and IVAP duration was an independent risk factor for IVAP catheter fracture. In fact, a retrospective study of 34 cases found out that predictive factors of catheter fracture were implantation method, duration of implantation, brand of device, and port-clavicle distance (14). Implantation more than 200 days and a port-clavicle distance <2.5 cm were independent factors for fracture of TIVAP on multivariate analysis, and were associated with a significantly higher risk of catheter fracture on stratified analysis. More details should be studied about the causes of catheter fracture.
Conclusions
In summary, IVAP implantation via IJV is a safe, effective and economical central venous catheterization technique. Our retrospective analysis found that IVAP catheter fracture was significantly correlated with patient’s occupation, age, living habits and IVAP duration, but not with IVAP implantation site, catheter traveling pattern and intravascular outer angle. Therefore, proper education should be provided to patients with high-risk factors for early prevention, and a long-term regular follow-up and monitoring system should be established to control the risk of catheter fracture.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by ethics board of the 4th Hospital of Hebei Medical University (No. 2019MEC113).
References
- Yildizeli B, Laçin T, Baltacioğlu F, et al. Approach to fragmented central venous catheters. Vascular 2005;13:120-3. [Crossref] [PubMed]
- Gabelmann A, Kramer S, Gorich J. Percutaneous retrieval of lost or misplaced intravascular objects. AJR Am J Roentgenol 2001;176:1509-13. [Crossref] [PubMed]
- Ko SY, Park SC, Hwang JK, et al. Spontaneous fracture and migration of catheter of a totally implantable venous access port via internal jugular vein--a case report. J Cardiothorac Surg 2016;11:50. [Crossref] [PubMed]
- Johansson E, Engervall P, Björvell H, et al. Patients’ perceptions of having a central venous catheter or a totally implantable subcutaneous port system-results from a randomised study in acute leukaemia. Support Care Cancer 2009;17:137-43. [Crossref] [PubMed]
- Lokich JJ, Bothe A Jr, Benotti P, et al. Complications and management of implanted venous access catheters. J Clin Oncol 1985;3:710-7. [Crossref] [PubMed]
- Liu X, Guo P, Zhang J, et al. Treatment of iatrogenic intravascular foreign body: Experience of 15 cases. Chin J Interv Imaging Ther 2012;9:508-11.
- Wu ZL, Li ZG, Li SZ, et al. Interventional retrieval of fractured catheter originated from implanted central venous port access system: its clinical application. Chi J Clin Radio 2015;34:271-5.
- Wu CY, Fu JY, Feng PH, et al. Catheter fracture of intravenous ports and its management. World J Surg 2011;35:2403-10. [Crossref] [PubMed]
- Lin CH, Wu HS, Chan DC, et al. The mechanisms of failure of totally implantable central venous access system: analysis of 73 cases with fracture of catheter. Eur J Surg Oncol 2010;36:100-3. [Crossref] [PubMed]
- Surov A, Wienke A, Carter JM, et al. Intravascular embolization of venous catheter--causes, clinical signs, and management: a systematic review. JPEN J Parenter Enteral Nutr 2009;33:677-85. [Crossref] [PubMed]
- Aitken DR, Minton JP. The "pinch-off sign": a warning of impending problems with permanent subclavian catheters. Am J Surg 1984;148:633-6. [Crossref] [PubMed]
- Mirza B, Vanek VW, Kupensky DT. Pinch-off syndrome: case report and collective review of the literature. Am Surg 2004;70:635-44. [PubMed]
- Zhou T, Tang TT, Li YT, et al. Comparative study on two different implantable vascular access devices: an analysis of 2897 cases. Chin J Prac Surg 2015;35:753-5.
- Chang HM, Chou YC, Hsu SD, et al. Predictive risk factors for fracture at catheter of totally implantable venous access devices via subclavian vein insertion. J Med Sci 2014;34:161-5. [Crossref]