
Follow-up of at least five years after lumbar transforaminal epidural steroid injection for radicular pain due to lumbar disc herniation
Herniation of the lumbar disc (HLD) is the most common cause of sciatica (1). Inflammatory materials surrounding a herniated disc can irritate the nerve root, causing radicular pain. Transforaminal epidural steroid injections (TFESIs) reduce inflammation around the nerve root, thus alleviating lumbar radicular pain (1). Several previous studies have demonstrated positive short-term effects of TFESI in reducing lumbar radicular pain (1,2). However, little is known about its long-term outcomes. We investigated the outcome of TFESI after at least five years in patients with HLD-induced radicular pain.
We investigated the outcomes of patients with HLD who underwent lumbar TFESI at our university hospital from September 2013 to September 2014. The inclusion criteria were (I) age ≥20 years; (II) history of a single-level unilateral lumbar TFESI to treat single-level HLD demonstrated by magnetic resonance imaging; (III) numeric rating scale (NRS) score ≥3 before TFESI; and (IV) pain for less than six months before receiving TFESI. The exclusion criteria were (I) lumbar spinal stenosis; (II) back pain more severe than radicular pain; and (III) spinal surgery before TFESI.
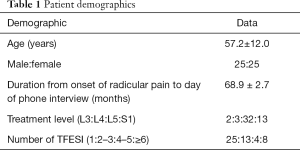
In total, 82 patients were recruited, and one investigator conducted phone interviews. Fifty-four patients answered their phones, among whom four patients refused to answer the questions. Finally, 50 patients were included (Table 1). For the investigation, we asked the following questions: (I) “Rate the degree of your current pain on a scale of 0–10, with 0 being no pain and 10 being the worst pain imaginable”; (II) “Are you taking pain medications prescribed by a medical doctor?”; (III) “Did you receive additional TFESIs after the first TFESI?”; (IV) “How many times did you receive additional TFESIs after the first TFESI?”; (V) “Are you currently receiving TFESIs when radicular pain is unbearable? If so, what was the interval between the two recent TFESIs?”; (VI) “Did you undergo spine surgery for uncontrolled pain despite receiving TFESIs?”; (VII) “Are you currently unemployed because of pain caused by HLD?”
Full table
The average NRS score before the first TFESI was 5.1±1.6. At the follow-up at least five years after TFESI, the average NPRS score was 2.4±2.2. Twelve patients (24%) reported no pain (NRS =0). Twenty-nine patients (58%) reported an NRS score of less than 3. Eight patients (16%) were taking oral pain medications prescribed by a medical doctor. Furthermore, half the patients (50%) received additional TFESIs after the first TFESI, and three patients (6%) were currently receiving repetitive TFESIs every two to six months. Four (8%) patients had undergone spine surgery for persisting unbearable pain. Nobody was unemployed because of pain caused by HLD.
Five to seven years after the onset of pain, NRS score had reduced from 5.1 to 2.4 in patients who received TFESI to treat HLD-induced radicular pain. Approximately 25% of the included patients reported complete resolution of the initial pain, and approximately 60% of the patients reported an NRS score ≤2 (i.e., approximately 40% of the patients had an NRS score ≥3). Half of the included patients received additional TFESIs. Thirty percent of the patients were taking oral pain medications, receiving repetitive TFESIs currently, or had undergone spinal surgery for uncontrolled pain. Considering that the effects of corticosteroids last for days to weeks, the results of our study reflect the natural course of HLD under conservative treatment.
Several previous studies have demonstrated excellent short-term outcomes of TFESI in patients with HLD. Kennedy et al. reported that over 70% of 78 patients with radicular pain due to HLD showed ≥80% reduction from the initial pain level six months after TFESI (2). However, most previous studies on the long-term outcomes have been focused on the results of surgical intervention. Recently, Burkhardt et al. reported long-term outcomes after microsurgical subtotal discectomy (3). They interviewed 158 patients over the phone and reported a mean postoperative follow-up period of 32 years. Of all the patients, approximately 69.9% were pain-free, while 13.9% took pain medications. Reoperations were conducted in 29.7% of the patients, among whom 8.2% had undergone surgery at the same level as the previous one. Kim et al. performed a retrospective cohort study recruiting 1,856 patients from the nationwide sample database and reported a reoperation rate of 16% ten years after spine surgery for managing HLD-induced pain (4). This suggests that the recurrence rate is relatively high after spine surgery for HLD.
Only one study has been published on the long-term outcomes of TFESI in patients with radicular pain due to HLD. In 2018, through phone interviews, Kennedy et al. evaluated the outcome five years after the initial TFESI in 39 patients with HLD (5). In their study, nine patients (23%) had current pain, nine patients (23%) received additional TFESIs after the initial TFESI, and 19 patients (49%) underwent spine surgery. Comparing their results with those of our study, we found that the rates of patients who had current pain and who received additional TFESIs were lower; however, the rate of spine surgery was much higher in their study. These differences may have resulted from different treatment methods preferred by clinicians or patients across countries or hospitals. Considering the results of Kennedy et al.’s and our studies, the recurrence rate or probability of pain persisting after TFESI seems to be as high as that after spine surgery.
Although the average NRS score reduced from 5.1 to 2.4, 40% of the patients who received TFESI for radicular pain secondary to HLD reported an NRS score ≥3 at five to seven years after the onset of pain. Furthermore, 30% of the total patients were taking pain medications, were receiving repetitive TFESIs every two to six months, or had undergone spine surgery. Accordingly, regardless of the surgical or non-surgical treatments, the long-term outcomes (or natural course) of HLD do not seem good. Our study is limited in that there is a possibility of bias because approximately 40% of the patients did not answer the phone or refused to be interviewed.
Acknowledgments
Funding: The present study was supported by a National Research foundation of Korea grant funded by the Korean government (grant no. NRF-2019R1F1A1061348).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Tak HJ, Jones R, Cho YW, et al. Clinical evaluation of transforaminal epidural steroid injection in patients with gadolinium enhancing spinal nerves associated with disc herniation. Pain Physician 2015;18:E177-85. [PubMed]
- Kennedy DJ, Levin J, Rosenquist R, et al. Epidural steroid injections are safe and effective: multisociety letter in support of the safely and effectiveness of epidural steroid injections. Pain Med 2015;16:833-8. [Crossref] [PubMed]
- Burkhardt BW, Grimm M, Schwerdtfeger K, et al. The microsurgical treatment of lumbar disc herniation: A report of 158 patients with a mean follow-up of more than 32 years. Spine (Phila Pa 1976) 2019;44:1426-34. [Crossref] [PubMed]
- Kim CH, Chung CK, Choi Y, et al. The Long-term Reoperation Rate Following Surgery for Lumbar Herniated Intervertebral Disc Disease: A Nationwide Sample Cohort Study With a 10-year Follow-up. Spine (Phila Pa 1976) 2019;44:1382-9. [Crossref] [PubMed]
- Kennedy DJ, Zheng PZ, Smuck M, et al. A minimum of 5-year follow-up after lumbar transforaminal epidural steroid injections in patients with lumbar radicular pain due to intervertebral disc herniation. Spine J 2018;18:29-35. [Crossref] [PubMed]


