
Tapering opioids: a comprehensive qualitative review
Opioid therapy in society
Multiple populations have been started on long-term opioid therapy (LTOT) progressively over the last several decades. Approximately 650,000 opioid prescriptions are dispensed daily in the United States (1,2). In 2015, 4.3 million Americans were on opioids for chronic non cancer pain (CNCP). Among veterans attending medical clinics, 2.5% are on LTOT (3). In 2010, 48,000,000 ambulatory surgical procedures were reported for which 1.6 million were started on LTOT and 160,000 eventually developed an opioid use disorder (OUD) (4-9). In 2014 alone, there were 245 million opioid prescriptions written and between 9.6 and 11.5 million individuals on LTOT (over 3 months on opioid therapy) (10,11). The unused opioids are frequently released into the community and become a primary source of misuse among family members, as well as the community at large (12). Of family members who do became addicted to opioids, 70% were first exposed to opioids by a family member using commercially available opioids. Opioid stewardship has become a growing concern and like antibiotic stewardship attempts are being made to minimize harm and maximizes benefits. An important part of stewardship involves opioid tapering for which most clinicians have little training or education. The purpose of this review is to instruct and educate physicians on the who, when, why, and how to taper and the potential benefits, problems, and pitfalls to tapering.
Long-term opioid therapy, the opponents process, and allostasis
A subgroup of individuals on LTOT develop insensitivity to rewards commonly experienced in the natural environment. The change in hedonic balance in these individuals shift to a negative effect, anhedonia and depression/dysphoria also termed “hyperkatifeia” (13,14). This “shift-right” in the reward set-point occurs also for analgesia, in particular the domain, “pain relief” (15). CPD is a state of persistent reward deficit (16-20). The-is “hyperkatifeia” of a chronic abstinence syndrome (anhedonia, anxiety, irritability, depression/dysphoria and craving) more than physical symptoms of withdrawal is the single important motivator for persistent opioid use and abuse (15,21). Hyperkatifeia is also a motivator in addiction (compulsive use, loss of control and continued use despite harm). Hyperkatifeia more than physical pain leads to dose escalation. The patient will complain of an absence of or diminishing pain relief (15). This occurs in the face of stable unchanging disease, no evidence of recent physical injury or objective radiographic changes in the original injury (22).
Opioids produce reward and the sense of pain relief through activation of mu opioid receptors within the mesolimbic system (mainly nucleus accumbens, ventral tegmentum area and amygdala). The mu/galanin heterodimers within the ventral tegmentum are largely responsible for the release of dopamine in the mesolimbic structures which leads to the rewarding effects experienced by patients. Most potent opioids such as morphine and fentanyl activate these dimers, but methadone does not and hence have analgesic effects but less reward (23,24). Dopamine activity in the nucleus accumbens and amygdala cause rewarding and motivational effects associated with opioids and other substances of abuse. All substances of abuse acutely lower rewarding threshold (25-31). The “liking” affect is mediated through the nucleus accumbens and “wanting” affect mediated by phasic release of dopamine in the nucleus accumbens (31,32).Over time rewarding thresholds to opioids increase and are replaced by negative reinforcement in abstinence resulting in the need to continually take opioids to avoid the negative affect (33).Tapering unmasks brain adaptations within mesolimbic areas that were both created and suppressed by LTOT (34). There is also a recruitment of brain stress neurocircuitry which releases corticotropin releasing factor CRF and activates both N-methyl-D-aspartate receptors (NMDA) and alpha-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid (AMPA) receptors via glutamine released from the prefrontal cortex to amygdala and nucleus accumbens (35-37). Kappa receptors within the ventral tegmental area are also upregulated under stress and bound by dynorphin which results in dysphoria. The kappa opioid receptor then becomes constitutively activated independent of dynorphin causing long term craving. The activated receptor counters dopamine rewarding effects, mediates and the aversive effect of withdrawal (38-41). Activation of kappa opioid receptors reinstate drug seeking behavior in animals while kappa receptor antagonists block stress-induced drug seeking behaviors (40). This is likely the mechanism by which buprenorphine, a kappa receptor inverse antagonist, improves mood and blocks craving (42-46).
The second area where there is an opponent response to morphine is within the locus coeruleus (LC). Over time morphine upregulates adenyl cyclase 8 which in turn activates CAMP-response response -element protein (CREB). This causes an increase in tyrosine hydroxylase, which is the rate limiting enzyme for the synthesis of norepinephrine. Norepinephrine accumulates under the influence of morphine. Upon morphine withdrawal glutamine release depolarizes LC neurons which have superactivated CAMP. This causes massive norepinephrine release resulting in withdrawal symptoms (47). Alpha-2 adrenergic receptors presynaptically act as autoreceptors and when activated prevent the release of norepinephrine.
Groups which may benefit from opioid tapering
Sixty percent of patients prescribed short term opioids abandon them, so chronic opioids are the exception not the rule (48,49). Nearly half discontinue them for reasons of side effects or for the public stigma of addiction (50). Some individuals whose pain resolves on LTOT are motivated to taper their opioids are thus reasonable candidates to do so. Individuals placed on LTOT for work related injuries in general do not benefit from opioids and most should be considered candidates for tapering. Opioid therapy fails to improve function in the majority and does not increase a return to work or employment (51,52). In fact, opioid therapy is associated with non-completion of rehabilitation, reduced rates of returning to work, and higher healthcare costs. Individuals on morphine equivalent daily doses (MEDD) of greater than 50 mg have an 11-fold greater prevalence of being on social security disability income supplement long term. In fact, part of rehabilitation which is vital to success of rehabilitation therapy is tapering pre-rehabilitation opioid therapy (53).
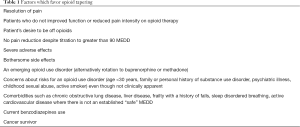
Another group of patients who should be considered for tapering are those surviving cancer, those with pain processing disorders such as fibromyalgia and those with migraines (Table 1) (54). Increasing numbers of cancer survivors may be on opioids for years related to various pain syndromes and face long term risks with opioid therapy (55). Of note, neuropathic pain from chemotherapy and radiation is poorly responsive to opioids (56-65). Many patients are cured but enter survivorship opioid dependent. Cancer survivors are not immune to the long-term risks of opioid therapy including OUD and addiction as well as osteoporosis, hypogonadism, infections, and sleep disordered breathing to name a few (66-68). The care of this population is often divided between family practitioner, palliative specialist who participated in their care during active anti-tumor therapy, and the oncologist. Who is responsible for opioid therapy in survivorship remains a question. The CDC guidelines exclude cancer patients such that guidelines for survivors need to be established (2,59,69,70). The need to escalate doses due to increasing pain in survivorship is complicated and may be due to opioid induced analgesic tolerance, opioid induced hyperalgesia, an emerging OUD, or recurrent cancer (71-74). It is likely that the risk of OUD is underestimated. It is likely to occur at the same frequency as in the general population, which would be approximately 7–10% of those on LTOT (71). Hence, opioid tapering would benefit this population hopefully reducing the risk of an OUD as well as other long-term complications. However, few palliative services have policies in regard to screening for opioid misuse (75). Yet 50% of the palliative care population who are questionnaire screen positive for abuse risk have unexplained urine toxicology findings (76,77). Interestingly, hospice patients without pain are often prescribed opioids for “just in case they have pain” even though they are comfortable. Opioid prescriptions for hospice patients are seen as usual care though a significant minority do not have pain and will die comfortably at home without pain (78).
Full table
Primary care physicians provide most of the LTOT for patients. Though the number of prescriptions has been declining, larger practices, rural practices, and patients in a lower social economic classis have greater high-dose prescription rates (79). Interestingly, opioid prescriptions increase 33% as the primary care physician’s work-day progresses. If a physician falls behind in schedule, opioid prescriptions increase by 17%. In contrast, the use of NSAIDs or physical therapy do not follow the same pattern (80).
Opioids are often continued after a surgical procedure whether surgery takes place in an operating room or in a non-operating room. Between 9–13% of patients undergoing surgical procedures are maintained on opioids greater than 90 days. This continuation from the postoperative setting to home is related to the perioperative opioid prescription dose, the days of supply provided by the surgeon during hospitalization, the preoperative receipt of opioids, and the patient’s polypharmacy (81). Many are continued on opioids without the consideration of tapering. Patients may be given a prescription of opioids even though they have not taken an opioid the day before discharge and are without pain. The responsibility for managing postoperative analgesia may change hands over time from the surgeon to primary care without exploring the reasons for ongoing opioid therapy.
Patient and clinical characteristics which facilitate or are barriers to tapering
Individuals on short term opioid therapy (less than 2 weeks) or as needed opioids and not daily may not require tapering. Individuals on long-acting (LA) rather than short-acting (SA) opioids can be tapered using either form of opioid, but those on LA opioids will usually take longer to taper (82). Certain patients are more suitable or more easily tapered from opioids than others. Those motivated, younger, dissatisfied with opioid therapy, or who have noted reduced function, lack a response, or have bothersome side effects are likely to want to be tapered off opioids (83). Seventy-five percent of individuals with CNCP will agreed to tapering there opioid if offered (84).
Individuals with certain personality types will find it difficult to wean from LTOT. Individuals with a borderline personality have difficulty with interpersonal relationships, boundaries, and have self-destructive behaviors. They tend to be reluctant or resistant to changing treatment and have problems trusting physicians. Individuals with a borderline personality have an increased lifetime risk for pharmaceutical opioid dependence [odds ratio (OR) 2.49; 95% confidence interval (95% CI), 1.42–4.38]. They also have an increased benzodiazepine use, suicidal thoughts, and lifetime suicide attempts (85). Patients with the emerging OUD while tapering from LTOT will also be resistant to tapering their opioids. These individuals are 3–4 times more likely to relapse from opioid abstinence than someone without pain but with an OUD (86). Tapering may still be successful in this subgroup of patients, but it will be in a minority. Approximately one quarter of individuals (27.6%) will be successfully tapered and remain abstinent at 1 year (87).
Other psychiatric disorders include depression, general anxiety, and posttraumatic stress disorder (PTSD), all of which are associated with resistance to tapering. PTSD patients and those experiencing sexual abuse as a child are susceptible to developing an OUD on LTOT (88-91). Childhood sexual abuse child increases the risk of an OUD 3-fold (92). First degree relatives of individuals with an OUD or addiction have an 8-fold risk of developing an OUD (93) Opioid withdrawal symptoms mimic the hypervigilance and startle responses of PTSD, which if experienced by patients with PTSD will discourage them from considering a tapering approach (94). Patients admitted with opioid dependence and/or abuse have a statistically significant higher prevalence of depression, PTSD, and anxiety compared with those hospitalized for opioid overdose (95). Physicians who attempt to taper opioids in these groups of patients will have an increased burden of calls, patient inquiries, concerns, and visits relative to the general population which will tend to wear clinicians out mentally (96). Thirty-four percent of patients with depression on opioids abandon tapering and 32% will resume LTOT frequently by seeing another physician who is willing to prescribe (97). Patients with depression require additional help if they are to be successfully tapered. The provision and adherence to antidepressants leads to a greater success in tapering and abstinence (OR 1.24; 95% CI, 1.05–1.46) (98). Individuals with psychiatric disorders and OUD require interdisciplinary support for successful tapering.
Individuals on high opioid doses and high pain intensity on LTOT are more difficult to taper and are less likely to remain abstinent (97,99-103).
Individuals with other substance use disorders, such as alcohol or tobacco, have a greater risk of developing an OUD and more difficult to taper from LTOT. Overall, individuals who used tobacco have a 3-fold risk for an OUD. Daily smokers will have a 5-fold risk for an emerging OUD on LTOT while intermittent smokers have a 3-fold risk (104).
The need to increase doses for CNCP over time is not a reliable predictor of an OUD but does make it more difficult to taper opioids. Analgesic tolerance leads to increased healthcare utilization and persistent anxiety, insomnia, fatigue, depression, and craving while tapered from opioids. This may be the result of an evolving neuroplastic opponents process and developing allostasis from long term opioid exposure, clinically labeled as complex persistent opioid dependence (CPD) (105). Certainly, patients who experience acute withdrawal are motivated to stay on opioids. Acute withdrawal which occurs for 7–14 days is managed by multiple medications and will be discussed later in this review. Most will not have increased pain, dysphoria, or depression once stably off opioids. However, a subset develops opioid aberrant behaviors, persistent craving, dysphoria, fatigue, and insomnia. This opponents process to long term opioid exposure counters acute opioid rewarding experiences and mood elevating effects. The opponents process can stubbornly persist (allostasis) as a new “normal” and does not return to the pre-opioid affect despite tapering opioids and abstinence (105,106). Many of the symptoms and signs of CPD resemble OUD and addiction. “Pseudoaddiction”, which is a term falling out of favor, is a form of CPD (106). Individuals before tapering who have been stable for years on modest opioid doses may manifest CPD characteristics with withdrawal (105,106). Patients may even “self-medicate” for the persistent affective symptoms and be labeled as having an OUD or addiction (107).
Tapering opioids clinically
How patients view conversations about opioid tapering and how to manage barriers
If one has pain on LTOT than one would assume pain and function should worsen when opioids are tapered. However, most patients tapered off opioids do not experience increased pain and, in fact, may experience a reduction in pain intensity over time. Reductions in pain severity off LTOT are more likely to occur in those who have mild to moderate rather than severe pain (108). Eighty percent have some reduction in pain, 15% have stable pain intensity, and only 3% have an increase in pain intensity with tapering (82,99,109-113). Even individuals with high pain intensity on high doses of opioids can have opioids tapered to lower and safer dose without causing increased pain intensity. In one study, codeine use was significantly reduced from mean of 237 mg [standard deviation (SD) 65] pre-treatment to 45 mg (SD 66) at 3 months and to 48 mg (SD 65) at follow-up without significant increase in pain (110). In a second study patients on an average MEDD of 288 were able to be tapered to 150 MEDD over 4 months without worsening pain (114).
It is tempting to use the opioid epidemic and opioid overdose deaths as a means of introducing the topic of tapering to patients. However, the patient's perceptive of risk of overdose relative to the true risk is quite low. The public stigma of addiction associated with LTOT is more likely to be a motivating factor for patients (115). A better way to introduce the subject of tapering is with the positive benefits of abstinence rather than on the negative note of addiction. Patients are not motivated by public reasons for limiting opioids such as an opioid crisis (96). Most are motivated to taper opioids based on personal reasons (economic benefits, less pills to swallow, fewer side effects, improved sense of well-being, and function and quality of life). However, a subset will be motivated by the long-term potential detriment to opioids such as the risks of falls, hypogonadism, fracture risks, sarcopenia, sexual dysfunction, wound dehiscence, and the risk of infections (66). The potential for improved quality of life off opioids without increasing pain, and even some improvement in pain will be attractive many individuals (116). Though physicians should not use the stigma of “opioid dependence”, the public opinion and its confusion with addiction though motivating some is the wrong approach (117). Patient education about the differences between opioid dependence and addiction is important so that patients are comfortable about making decisions based on accurate information. The risk of misinformation is that patients will simply stop their opioid at once and sustain a withdrawal syndrome. Without tapering particularly at high doses (greater than 120 MEDD) there is a great risk of increasing healthcare resource utilization including emergency department visits and hospitalization, harming patients, and making it more difficult to have patients want to taper out of fear of severe withdrawal (118).
Patients may have the perception that non-opioid analgesics are relatively ineffective in managing their pain compared with opioids (115). There is no data to suggest that opioids are superior to non-opioid analgesics in managing chronic pain, opioids are not inferior but are associated with greater risks (119). Patients may have a misunderstanding that opioids are the only option they have to control their pain. Another motivating factor to tapering opioids preoperatively is to improve perioperative pain management. Postsurgical pain is much more difficult to manage in patients highly tolerant to opioids. Poorly controlled post-surgical pain is a feared experience and a motivating factor to tapering opioids before elective procedures (120).
There is no doubt that a subset of patients will become psychologically resistant to tapering or lack motivation. Some will develop “pseudo-opioid resistant “pain. This subgroup of patients will complain of poorly controlled pain despite in reality having well controlled pain in order to stay on opioid therapy (121). This will be true particularly if patients are subject to a unilateral physician approach to tapering rather than a consensus approach between patient and physician. Some will resist tapering out of fear of withdrawal symptoms, others out of fear of uncontrolled pain and still others out of fear of loss of the rewarding affect associated with opioids confused for analgesia or out of loss of “pain relief” (122). Individuals on high opioid doses, those experiencing severe pain on high doses, those who have a distrust of the medical profession, those with an anxiety disorder, depression, PTSD, personality disorder, hyperalgesia or an evolving OUD or CPD will put up resistance to reducing their opioid dose (96,115,123,124). In these groups of patients, if the topic of opioid tapering is brought up for discussion, it may be met with anger, hostility and threats to leave the medical practice, even threats of physical harm (115). Such a response should be met with empathy, negotiation of goals, ongoing conversations if first resisted and non-abandonment (125). A compromised goal may be to reduce the opioid dose to a safer level (perhaps less than 90 MEDD for example). Forced, unilateral tapering can easily destabilize these groups of patients who a appear to be quite stable on stable opioids doses (105). Only if opioid diversion occurs, are physicians forced to take a more unilateral approach to stopping LTOT rather than contribute to a felony (Drug Enforcement Administration. Issuance of Multiple Prescriptions for Schedule II Controlled Substances Docket No. DEA-287N; pages 52724-6; September 6, 2006). Adherence and non-adherence to opioid tapering and opioid therapy is a spectrum and not an “all or nothing” phenomena (126). Physicians need to manage patient expectations. Conversations should be centered on the individual and clinical circumstances.
Tapering: the physician’s point of view and how to manage
A subset of physician, probably less so at the present time, feel that LTOT poses a minimum risk (127). Much more at the present time are giving up their DEA license and are not prescribing opioids out of fear of medicolegal entanglements or due to the increasing burden of prescribing opioids and prescription authorizations required by insurance companies (128). Although patients in general on opioids report favorable perceptions of their doctor-patient trust in managing opioids, implementation of opioid risk reduction initiatives reduce this level of trust for a minority of patients (129). Physicians face the demand by patients for relief of their pain quickly (130). Patients are often unwilling to change their lifestyle which contributes to pain or opioid risks and may have unrealistic expectations of responses to opioids (130). Physicians often do not consider opioids as a “trial” over a limited period with objective outcomes (reduced pain severity and improved function) but as a chronic therapy with limited options for other approaches nor do they outline an exit strategy prior to initiating opioids (130). For most have been educated in an opioid-centric curriculum to pain management (World Health Organization 3-step analgesic ladder) though this has changed (131). Pain is often marginalized in a disease centered approach to health care which often fragments pain management or leaves the prescribing to trainees (131). Physicians tend to be reluctant to use universal precautions during opioid therapy due to the increased time involved and the necessity of looking prescription drug monitoring sites with each opioid prescription and while tapering is reasonable even more time, office visits and effort is needed than maintaining patients on opioids. There are few guidelines that provide directions to tapering. Many have not tapered patients off LTOT. Most physicians are confident in prescribing opioids for chronic pain but have high levels of dissatisfaction doing so. Physicians have a high awareness of the potential for opioid misuse and are concerned about inadequate training in pain management relative to the frequency of pain in practice (131). The majority have major concerns about regulatory scrutiny (132). Tapering may be seen as a welcome relief to a dissatisfying practice of LTOT. However, tapering risks rupture the patient-physician relationship. Tapering is associated with a 4-fold risk of termination of care either by the patient or physician (133). In general, education about opioids and long-term risks have not changed the practice of the physician prescribing (134). The publication of CDC chronic pain guidelines may influence opioid prescribing (135).
Primary care physicians manage the bulk of patients on opioids for chronic pain. In a qualitative study four groups of patients were recognize for which primary care physician’s would consider tapering opioids; those with high risk behaviors, those experiencing serious side effects, those with bothersome but not serious side effects, and patients who wished to taper (124). Primary care physicians face the demand or request for opioids more frequently than other physician specialties. At the same time primary care physicians are more likely than any group of physicians to understand the social and emotional dynamics of patients and families which are likely to impact patients’ tapering, and are in a position to address patient fears, focus on patients’ best interests, provide anticipatory guidance about tapering, and develop an individualized tapering plan (136). The use of diagnostic procedures beyond physical examination has been demonstrated to change the way pain is managed in 30–60% of individuals (137). However, the cost in office time, approval from insurance companies, and procedure scheduling are barriers. It is much easier to simply prescribe an analgesic to treat the pain particularly in a busy office practice (137). Barriers are the limited options outside of opioids. Pain specialists are not easy to find. Pain management practices are often interventional in nature and do not provide continuity or analgesics. Pain rehabilitation programs are even more scarce, and reimbursement limited. Insurance coverage for pain rehabilitation, non-pharmacologic interventions and pain specialists is marginal at best (138). Physicians who are not licensed to use buprenorphine for addiction are relatively uncomfortable in tapering as are physicians in large healthcare systems (139). Insurances are more likely to pay for an opioid prescription than pain rehabilitation. Licensing of certain commercial opioids for CNCP may provide a sense of safety for clinicians and reinforce on going practices (140). Many of the publications which justify the use of opioids for chronic pain were of a limited timeframe, usually 12 weeks. Patients were highly screened for addiction though many of the studies did not use universal precautions or urinary toxicology while patients were on study. Few were long-term (a year or greater) in duration as safety studies and hence one cannot determine long-term safety with accuracy.
In a qualitative study, only half of primary care physicians (54%), believed opioids should be limited to acute pain, cancer pain or those with life-limiting illnesses in palliative care (140). Nearly 1/3 (32%) did not believe that opioids have a very limited benefits in improving function and quality of life. There is an overestimation of the benefits of opioids by physicians which dampens the desire to taper. Over 2/3 (77%) believe that there are no effective alternatives to LTOT. Physicians more often prescribe opioids when faced with a demanding patient than a patient who do not appear to benefit from opioids (140).
Physicians feel that discussions centered on tapering opioids are burdensome and are often dreaded. Encounters are usually long and emotionally exhausting (124). It is often easier to maintain opioid therapy than to fall behind in an office schedule. This may be the reason why opioids are more frequently prescribed later in the day as previously mentioned. Physicians face a lack of trust and patients often project the feelings that they are being labeled as addicts when the prescription is brought up in a discussion by the physician with the purpose of tapering (124). Education about the personal benefits of tapering, empathy, engaging family members and correcting myths about increasing pain, and reduced function in abstinence are important and helpful measures but requires education. Gaining consent, individualizing tapering, and allowing” plateaus” during a tapering protocol helps patients maintain some control over the process. Using expert guidelines would be helpful though there are few evidence-based guidelines available. As mentioned before reassuring patients that they will not be abandoned is important (141).
Principles of tapering opioids
Gaps and questions
The mechanics of tapering are complex and unfortunately not well studied or established by high quality randomized studies. Practice is based more on experience than evidence (Table 2) (142). The rate of tapering is divided into ultrarapid (within 7 days), rapid (within 3–4 weeks), and slow (over months) (142,143). Patients are frequently on multiple opioids or a LA with a SA opioid. Whether to consolidate multiple opioids into a single opioid using MEDD as a guide or individually taper the SA and LA opioid sequentially is not established. Likewise, whether to taper the SA opioid first or the LA opioid first in sequence is not known nor has been compared. Does one include medications for withdrawal symptoms or wait until withdrawal symptoms occur? How does one taper transdermal opioids? Should an interdisciplinary program be routinely used during tapering which would include cognitive behavioral therapy, physical therapy, adjuvant analgesics? How does one manage a patient with chronic pain and an OUD during tapering, and should this be different than managing addiction? Are there differences between those with pain and OUD and those with an OUD alone? The mortality rate for individuals is almost double if on 50–99 MEDD (1.92) and is 2.04 for those on 100–199 MEDD (144). Should patients be completely tapered off opioids or tapered to a safe level (below 50–90 MEDD). Who should be rotated to an opioid such as methadone or buprenorphine which produces less craving? What should be done if pain worsens during the tapering process? How does one manage CPD? What about substituting cannabis for an opioid or using cannabis as an adjuvant during tapering, to treat withdrawal or maintain abstinence? What about hormone replacement for men who are testosterone deficient on opioids? Will this help control pain and facilitate tapering? What are the medicolegal risks to tapering opioids?

Full table
Tapering rate and speed of dose reduction
There is scant evidence about the optimal tapering rate. In general, using 25% of the previous days opioid does will prevent overt withdrawal symptoms (145). A fixed standard dose application based on the patients total daily dose rather than individualized starting doses reduces withdrawal symptoms particularly at high doses (>180 MEDD). Fixed standard doses should be based on the mean daily dose to start (146). Ultra-rapid tapering usually requires hospitalization and frequently sedation. Alpha-2 adrenergic agonists (clonidine and lofexidine) will be needed to manage withdrawal symptoms (147). It is important that physicians use the term “ultra-rapid tapering” when documenting care in the hospital rather than use the term “detoxification” which is associated with addiction (143,148,149). The main reasons for an ultra-rapid taper are life-threatening cardiac side effects or an emerging psychiatric disorder related to opioids or made worse by opioid therapy (150,151). A Cochrane of 26 randomized clinical trials involving 1728 participants reported safe withdrawal from opioids which took 1 to 2 weeks in most studies. Clinicians can decrease opioid doses up to 50% per day (152-154). Ultra-rapid tapering has also been performed when a peripheral block has producing a dramatic reduction in pain and the patient is experiencing significant serious opioid toxicity after the block or procedure (155). The experience of withdrawal symptoms with ultra- rapid tapering can vary significantly between patients (155). Fortunately, ultra-rapid tapering is rarely needed, the majority can be tapered over a month or longer and not require hospitalization. Some have questioned the value of ultra-rapid tapering from LTOT (148). There can be some unique and life-threatening toxicities that occur with ultra-rapid tapering. These include sudden cardiac death, aspiration pneumonia, pulmonary edema, and diabetic ketoacidosis from a rapid release of norepinephrine (147).
Rapid and slow opioid tapering
Rapid and slow opioid tapering are done in most individuals. These approaches do not require hospitalization and are unlikely to require medications to treat withdrawal symptoms. However, a monitoring questionnaire for withdrawal symptoms is helpful during tapering and universal precautions should continue through the tapering process (70,156-158). Rapid tapering has been done either as “masked” (patient unaware of the dose schedule during tapering) or “open” without much difference in outcomes (111). Eighty-nine patients in the masked group in one study were initially abstinent compared with 68% in the open patient-controlled group (P<0.05), but by 1-month follow-up, the advantages disappeared. Other studies have demonstrated a high success rate with an open rapid taper (82,102,159,160). Different schedules have been used for which comparison is impossible. One schedule involved reducing the dose 20–50% each week to 30–45 mg daily then decrease by the same percentage every 2–5 days. Alternatively, the opioid dose can be reduced 10% every 3–7 days until 30% of the original dose is achieved then a 10% dose reduction per week (142). The second schedule slows the tapering process at lower doses. Tapering is a bit tricky at lower doses particularly when using LA opioids. One may have to rotate to a SA opioid to finish tapering. For example, once LA oxycodone 10 mg twice daily is reached than one would need to switch to SA oxycodone 5 mg to taper further. The dose would be 2.5 mg every 4 hours as the next step. Once the patient is taking an opioid only intermittently and not daily, the prescription can be stopped (83). In one study, 50% of patients on LA morphine or methadone could be successfully tapered over 16 days with no difference between opioids (161). In a second study, the best outcomes occurred when methadone was tapered at a rate of 3% per week which would fall into a slow taper strategy (162). This demonstrates the wide differences in tapering schedules.
For slow tapers, the general rule is that the duration of the taper should be proportional to the duration of the opioid therapy (163). In general, a 10% (5–20%) dose reduction monthly seems to work. The rate of tapering should be slowed when reaching lower doses (142). The CDC guidelines recommend a 10% reduction in dose per week as an intermediate schedule which is between a rapid and slow taper (2).
Tapering multiple opioids
Tapering opioids in individuals on both LA and SA opioids is a challenge. Those on SA opioids can be tapered more quickly than those on LA opioids. Patients are less resistant to tapering SA opioids but there is also a greater risk for abuse and illicit route conversion with SA opioids because many are not tamper-resistant. For those without an OUD, tapering the SA opioid is quicker than converting to a LA opioid equivalent then tapering. For those with an OUD or CPD rotating to a LA opioid or buprenorphine or methadone may be preferred (164). If tapering both a SA and LA opioid (which should be rare in CNCP), one should taper the SA opioid first or adjust the LA opioid to include the daily SA dose, otherwise patients may increase the use of SA doses during the LA taper. On the other hand, one is limited by the pharmaceutical availability of LA opioids such that dose reductions will not follow the 10% reduction rule of a slow taper. As an example, if the patient is on LA morphine 30 mg every 12 hours, the next practical increment is a 25% reduction in does (LA morphine 15 mg every 8 hours) rather than a 10% reduction in dose and requires a new prescription and perhaps drug approval from the insurance company. SA opioids may sometimes be used to treat transient pain flares for the week after a dose reduction that may come with a tapered opioid dose (83). However, this actually may forestall further tapering or actually lead to a dose increase when adding LA and SA opioids.
When consolidating 2 different opioids into a single opioid or rotating to buprenorphine or methadone realize that MEDD determinations by equianalgesic tables are inaccurate (165,166). There is no universally accepted equianalgesic table. In a study that involved MEDD calculations by nurse practitioners, physicians and pharmacists (75 micrograms/hour fentanyl, methadone 40 mg per day, oxycodone 120 mg per day, hydromorphone 48 mg per day and hydrocodone 80 mg per day) the variations between and within specialties were quite marked; fentanyl 176 MEDD +/− 117, methadone 193 MEDD +/− 20, oxycodone 173 MEDD +/− 39, hydromorphone 192 MEDD +/− 55, hydrocodone 88 MEDD +/− 42 (166). Rotations from methadone or fentanyl to morphine have scant clinical evidence (167,168). In one study, the methadone to morphine ratio was 1 to 4.7 but involved only 16 patients (169). There is an increasing risk of opioid induced respiratory depression in those with organ failure if ignored by rote use of equianalgesic tables (170). In general, rotations should be at 50–75% of the equianalgesic dose (83). Equianalgesic tables do not consider patient characteristics, polypharmacy and comorbidities (96,142,171). The choice of rotation should also be dictated by co-morbidities and polypharmacy. As an example, if the patient is on LA morphine and SA oxycodone, consolidation of opioids should be to LA morphine since morphine pharmacokinetics are less influenced by liver disease (172,173). The published “safer” MEDD varies from <90–200 MEDD in guidelines. But co-morbidities like COPD reduce the acceptable” safer” MEDD level (174).
Tapering transdermal fentanyl
Transdermal fentanyl has unique problems when attempting to taper. There are limitations related to pharmaceutical dose availability which may be particularly problematic at lower doses. The options are to rotate to an oral LA opioid before tapering or reduce transdermal fentanyl using different patch strengths to the lowest strength then use SA opioids. For example, to rotation from 37 micrograms/hour of transdermal fentanyl one would use oxycodone 6o mg a day which would be 100 MEDD as a starting point with a 25–50% reduction in the LA opioid dose. Predicting the right dose is fraught with hazards not only due to the low level of evidence for equianalgesia but also because of the highly variable absorption to transdermal fentanyl (175,176). Reducing patch strengths incrementally limited by a pharmaceutical availability, requires multiple prescriptions over time (83). Dose reductions near the end of the taper will be incrementally large and could potentially cause withdrawal symptoms. This may occur with a change from 25 to 12 µg/h patches. Rotations at the lowest patch strength can be illustrated in the following. To switch from a 12 µg/h patch to oral morphine one would use 30 mg as an equivalent. So, with the next step from the patch use 2.5 mg of SA morphine every 4 hours (dose reduction included).
Alternatives to tapering in the stable and unstable patient
Patients can be divided into those who are psychologically stable during tapering and those who become unstable (177). Emerging opioid misuse, dysphoria and craving may arise during tapering. This is described in 3–17% of individuals (178,179). For those individuals who are stable and functional on stable low doses during LTOT, there is no evidence that forced tapering has benefits and may be harmful so as mentioned above consensus is key to tapering. No study has addressed the outcomes to mandatory tapering in stable patients and there are risks. The risk of mandatory tapering is destabilization which can lead to suicide (180-183). On the other hand, simply tapering someone with pain and an OUD without appropriate psychosocial and clinical support or consideration of maintenance analgesia is highly inappropriate (71). The CDC guidelines neither recommend forced tapering or tapering stable patients to a certain threshold MEDD (184).
The option of analgesic maintenance or rotation to buprenorphine or methadone should be considered in those patients who are developing craving, dysphoria, CPD or opioid misuse such as self-titration and running out of their prescription earlier than expected because of extra doses and not for reasons of opioid diversion (100,101). Analgesic maintenance focuses on pain, and symptoms of withdrawal whereas maintenance therapy primarily focuses on addiction behaviors rather than pain. There is obviously an overlap which can be confusing. However, if buprenorphine is provided primarily for analgesia, a special license is not required whereas if provided for maintenance therapy for addiction, a special license is required. It would therefore be important to document the reason for a rotation to buprenorphine or methadone. Methadone 60 mg or buprenorphine 16mg daily can stabilize someone who is demonstrating opioid abuse (185,186).
One third of individuals drop out of a tapering program and approximately the same resume LTOT which is likely to be under the care of another provider (97). Patients on high doses of opioids are more likely to dropout and more likely to resume analgesic maintenance (102). Patients with an OUD who are tapered from buprenorphine will have an increased incidence of positive urine toxicology for illicit substances and less abstinence than patients maintained on buprenorphine (187).
Analgesic maintenance may be with the original opioid or by rotation to methadone or buprenorphine. The latter 2 opioids may be preferred in those demonstrating opioid misuse (188). Methadone has less “drug liking” effects compared to other potent opioids and is inexpensive. However, methadone has more drug-drug interactions and risks for a prolonged QTC interval and Torsades de Pointe (189). On the other hand, buprenorphine can cause withdrawal if a “stop-start” approach to rotation is done with individuals on high doses of potent opioids (190). In general, a 12 to 24-hour time between stopping the high dose opioid (morphine ≥120 mg, methadone ≥45 mg/d) is needed to avoid precipitating withdrawal. Recently an overlap rotation with dose titration of buprenorphine and tapering the potent opioid has been done in a small group of patients without precipitating withdrawal (191). In those with pain and an OUD, buprenorphine should be combined with naloxone. Both methadone and buprenorphine should be given in divided doses for analgesia and not as a single daily dose as used for addiction maintenance therapy. One can add immediate release potent opioids to each and both buprenorphine and methadone can be used as sustained release opioids. However, if patients are on significant doses of immediate release opioids around the clock, adding buprenorphine may cause a withdrawal response due to receptor affinity. There are no randomized trials which compare outcomes to rotations to methadone or buprenorphine versus maintaining patients on their sustained release opioid (192). Such decisions need to be individualized and rotation determined based on patient and clinical factors (192).
Chronic persistent opioid dependence
CPD is further discussed as an important factor that influences tapering. Most clinicians who treat pain focus on pain intensity but what drives suffering and opioid misuse is not pain intensity, it is the unpleasantness of pain and opioid deficit “anti-rewarding” effects. This is an affective not cognitive response with the affective response derived from memory, appraisals, and perceptions about prospects of relief and the balance of risks versus rewards when weighing relief in light of present suffering (105). Those with CPD have a prolonged abstinence syndrome largely consisting of dysphoria, depressed mood, irritability, frustration, craving. Anger with behaviors are often described as “pseudoaddiction” (105). The allostasis which generates CPD is a persistent neuroplastic opponent response to long-term opioid exposure which occurs largely within the mesolimbic matrix (193-195). Clinically patients with CPD will have worsening function and “pain” and emerging insomnia. Patients will become emotionally unstable (105). If the clinician focuses only on the peripheral symptom of pain without addressing the other symptoms, tapering will fail. Individuals with CPD are often treated with benzodiazepines for sleep, sedatives, and antidepressants which leads to an increased risk for drug-drug interactions and adverse outcomes. Rotation to buprenorphine rather than polypharmacy would be a more reasonable approach since buprenorphine has analgesic effects, antidepressant activity, and blocks craving but does have a ceiling on adverse effects such as respiratory depression and constipation (196,197). Patients can be stabilized on 4–16 mg of buprenorphine (with naloxone) in divided doses prior to consideration of tapering (198). The American Society of Addiction recommends 4–16 mg be given initially, starting with the lower dose and repeating the dose if withdrawal symptoms persist (199). Recently an “overlap” rotation strategy has been published as mentioned above (191). Patients on 80 to 220 mg oral morphine daily were transitioned to buccal buprenorphine using 50% of the equianalgesic dose while the other opioid dose was reduced in half without inducing opioid withdrawal or diminishing analgesia (191). Alternatively, methadone starting at 40mg or less could be done to stabilize the patient in a “stop-start” rotation. Sublingual buprenorphine can be illicitly converted for intranasal and IV self-administration and although the drug-liking effects are substantially less than heroin, there is a subjective high at high doses more for IV than intranasal administration (200) The buprenorphine/naloxone combination has much less abuse potential than buprenorphine and produces aversion effects particularly at higher doses which contains more naloxone (201,202). Once the psychological symptoms are stabilized and protracted abstinence symptoms resolve, other therapies could be used for treatment resistant pain (105). For patients with pain and high dose opioid requirements (≥100 MEDD) and significant psychological symptoms or an OUD, analgesic maintenance would be the best approach. Patients on lower doses of opioids and few psychological symptoms and without an OUD could be tapered from buprenorphine or methadone (105). Tapering someone with an OUD on buprenorphine should be done slowly. In one study a 4-week taper was 4 times more successful than a 1–2-week taper (203). Individuals with CPD will have a high dropout rate with tapering. Success should not be measured in abstinence or the lowest opioid dose that can be achieved but should be patient-centered which includes improved function, affect, socialization and resolved opioid abuse behaviors (101,142). Randomized trials comparing maintenance opioid analgesia versus slow tapering in this population does not exist such that physicians will need to individualize treatment based upon patient-centered outcomes.
Managing withdrawal symptoms
Medications to treat opioid withdrawal symptoms can provide a gateway to tapering and abstinence. The main cause of most but not all withdrawal symptoms is norepinephrine hyperactivity (204). Withdrawal symptoms can occur even with a slow taper and even when the tapering doses are appropriate (83). Acutely, norepinephrine hyperactivity may cause patients to demand an increase in their opioid dose or return to opioid therapy (205). Withdrawal symptoms will begin after 2–3 drug half-life periods of time after reducing or stopping an opioid and will be manifested by anxiety, hypertension, tachycardia, restlessness, mydriasis, diaphoresis, tremors, piloerection, nausea, cramps, diarrhea, shivering, myalgias and arthralgias, lacrimation, yawning and insomnia (206). Patients may not have all the symptoms, some will have more severe symptoms than others. Symptoms are not specific to opioid withdrawal and can be easily missed by physicians. Withdrawal, though dreaded, is not life-threatening in the great majority unless there are significant underlying comorbidities (150,207). Acute symptoms generally resolve in 7–14 days (145). Pre-withdrawal anxiety will worsen symptoms, symptoms may be masked by a placebo (208). A second abstinence syndrome can occur after acute symptoms have resolved. The second abstinence symptoms include general malaise, fatigue, a decreased sense of well-being, poor tolerance to distress and craving of various intensities. Patients may have reduced body temperature and bradycardia (83,209). Transient and time-limited hyperalgesia occurs with appropriate dose reductions. For most, there is improved function and an improved sense of wellbeing at lower doses which outweighs the temporary increase in pain. Reassurance and a care and temporary use of SA opioids may all that will be necessary. Tapering can be plateaued if necessary, at the patients request until the hyperalgesia resolves (210-213).
Meticulous management of withdrawal symptoms is important for successful tapering. If withdrawal symptoms are severe or poorly controlled, it may be better to stabilize the patient on buprenorphine than to use clonidine or lofexidine alone (two alpha-2 adrenergic receptor agonists which block norepinephrine release by binding to presynaptic autoreceptors in the locus coeruleus) (214). Buprenorphine increases the relative risk (benefit) of completing a taper by 1.59 with a number needed to treat of 4 versus alpha-2 adrenergic agonist therapy alone (214).
Clonidine is given in small doses of 0.1 to 0.2 mg and repeated based on response. The average daily does is 0.3–0.6 mg with a ceiling dose of 1.2 mg (215). Lofexidine which is the only FDA medication approved for opioid withdrawal symptoms, should be started at 0.6 to 0.8 mg three to four times daily up to 3.2 mg/d (216). Sixty percent of patients will be successfully tapered with an ultra-rapid protocol if lofexidine is administered (217). Lofexidine can prolong the QTc interval and may require ECG monitoring if patients have bradycardia, liver or kidney or heart disease or are on methadone (218). Because lofexidine can cause bradycardia and orthostatic hypotension, patients on beta blockers or calcium channel blockers are at increased risk for side effects. It is cleared by the mixed function oxidase CYP 2D6 and so drugs like paroxetine which blocks this enzyme can reduce lofexidine clearance and increase the risk for side effects (218). Both alpha-2 adrenergic receptor agonists can cause orthostatic hypotension. Clonidine and lofexidine are relatively ineffective in managing tremors, emesis and drug craving (216,219).
There are other medications used to reduce withdrawal symptoms. Baclofen 5 mg 3 times a day titrated to 40 mg as needed for 2 weeks, gabapentin 100–300 mg daily titrated to 2,100 mg or tizanidine 4 mg 3 times a day in lieu of clonidine have been used (220). Valproic acid and olanzapine are used for the irritability, dysphoria and depression associated with withdrawal (221,222). In a study of 53 individuals on methadone, both medications (olanzapine and valproic acid) reduced overt aggression, irritability and suicidality. The beneficial effects favored olanzapine over valproic acid (223). Trazodone, doxepin and olanzapine can be used sleep. However, trazodone in one study was ineffective in improving sleep in patients on methadone (224). Quetiapine has been used to reduce craving (225). The drawback to using gabapentin and quetiapine is the known risk with both (226-231).
For nausea, empiric use of ondansetron, prochlorperazine, haloperidol or olanzapine would be reasonable though there are no trials which provide guidance. Loperamide or bismuth have been recommended for diarrhea and dicyclomine for cramps (220). Antidepressants for emerging depression increases the success of tapering (232). Mirtazapine would be a reasonable choice due to few drug interactions, a more rapid onset to antidepressant activity and treatment of insomnia (233).
Cannabis and opioid tapering
There is a popular interest in substituting cannabis for opioids. Both Illinois a and New York allow certain patients on opioids to substitute cannabis for their opioid. The thoughts behind this substitution is that cannabis is a safer analgesic, associated with fewer deaths and is less addictive (234). However, one of the problems with this is that most opioid deaths as recorded from Massachusetts from 2013 through 2015 are not from commercial opioids but the street use of fentanyl by those with addictions. Over 60% are related to heroin and 45% have fentanyl detected by postmortem toxicology frequently not metabolized suggesting that the deaths occur with a couple of minutes after injection. Only 1.3% have an active commercial opioid prescription (235,236). It is unlikely that cannabis substitution for commercial opioids will significantly impact opioid deaths.
There are epidemiologic studies as well as observational studies which suggest that cannabis may in fact be opioid sparing. HIV patients with pain on cannabis have an odds ratio (OR) for the use of opioids of 0.57 (237). From New Mexico, individuals who are started in a cannabis program while on opioids have a 47% reduction in opioid use and a greater chance of being off opioids altogether than those not on cannabis (OR 17.22) (238). In an observational study, cannabis improved quality of life by 45% and reduced opioid use by 65% (239). In a survey of New England cannabis dispensary members, nearly 77% stated that their use of opioids diminished when they started cannabis (240). Two large epidemiology studies found that states with cannabis laws have reduced opioid related deaths and opioid prescriptions (241,242). State implementation of medical marijuana laws was associated with a 5.88% lower rate of opioid prescribing. Moreover, the implementation of cannabis laws was associated with a 6.38% lower rate of opioid prescribing (243).
There are multiple animal studies demonstrating that cannabis may be effective in reducing opioid withdrawal symptoms (244-247). In a study which looked at dronabinol to reduce acute opioid withdrawal symptoms in humans on oxycodone, 5–10 mg was not better than placebo abut 20–30 mg transiently reduced withdrawal symptoms from oxycodone. However, in the same study dronabinol worsened withdrawal related tachycardia (248).
All of these studies provide speculation as to benefits of cannabis in opioid dependent patients. Cannabis may facilitate tapering opioids by improving pain and blunting withdrawal symptoms. Cannabis may block opioid analgesic tolerance and rekindle analgesia in those on opioids who are demonstrating analgesic tolerance. Cannabis may maintain opioid abstinence in those who have been successfully tapered off opioids (239,249). Unfortunately, there are no randomized trials to confirm or deny any of these benefits.
There are also negative studies. In a study which aggregated opioid death rates in 19 states and the District of Columbia compared to 24 states without cannabis laws, there was a 52% increase in opioid deaths in those on cannabis (250). In observational and retrospective studies people on cannabis are more likely to use other illicit substances than those not on cannabis. People on cannabis are more likely to report medical and nonmedical use of opioids, stimulants and sedatives. People on cannabis relative to those not on cannabis have different morbidities which may account for differences. Cannabis may reduce prescription drug use, yet prescription drug use remains significantly high in those on cannabis (242).
There are multiple studies to suggest the cannabis is not helpful in managing opioid withdrawal, analgesia or abstinence. The early use of cannabis (age <18 years) increases the OR 16.5-fold of developing opioid abuse (251). Cannabis is a gateway drug to opioid misuse and addiction. In a group of patients undergoing slow methadone withdrawal, cannabis did not reduce withdrawal symptoms (252). Cannabis does not reduce withdrawal symptoms from heroin (253). Inhaled cannabis does not reduce opioid use and increases non-adherence to opioid prescriptions in a group of patients with chronic low back pain (254). Current use of cannabis with opioids is associated with an increases risk of an OUD (255). Cannabis increases the non-medical use of opioids. Individuals may become destabilized during an attempt to rotate from an opioid to cannabis or when they are combined before tapering (256). Cannabis use is also associated with opioid relapse in abstinence (257).
Therefore, the benefits to cannabis in tapering opioids, withdrawal and abstinence are not established and will not be established until there are randomized trials. There are multiple questions which need to be answered. The type of cannabis, frequency, dose and route of cannabis as to benefits in opioid therapy is completely unknown. Patients are on such a wide variety of phytocannabinoids from dispensaries that little can be learned from existing studies. To our knowledge, there are no studies that are originating from dispensaries to answer these questions and researchers with federal grants do not have access to dispensaries since by federal law, cannabis is a schedule 1 drug with no medicinal value and is illegal to have in possession (258). At the present time, there is more popular enthusiasm about the use of cannabis in opioid dependent individuals than evidence.
There may be a dose dependent benefit to cannabis. Intensity of cannabis use is an issue during abstinence. Intermittent or occasional use rather than daily use improved adherence to maintenance therapy for addiction (259-261). It may be rational to think that intermittent cannabis use would maintain opioid abstinence in those who have chronic pain, but it would require a randomized trial to validate the practice. The variability in reported outcomes regarding cannabis is likely related to the different cannabinoids within the cannabis used in the various studies (262). It is unfortunate that cannabis has been classified as a single “drug” in many studies. In a systematic review of cannabis used to palliating symptoms, the different ratios of THC to cannabidiol influenced responses to various symptoms (263). Cannabis which is predominately cannabidiol reduces harms, risks of addiction, anxiety and depression (264-266). In animal studies, cannabidiol reduced opioid withdrawal symptoms without increasing drug-induced conditioned place preference (244,245,267).
At the present time, there are no randomized controlled trials that provide evidence that cannabis from dispensaries in the United States reduces opioid doses, helps in tapering opioids, and ameliorates withdrawal symptoms and maintains opioid abstinence (268). It is likely that subgroups of individuals at risk for an OUD will also be at risk for a cannabis use disorder. Policies of exchange may in fact be exchanging addiction drugs and promote problems public substance use disorders without the ability to monitor or control use (264). It may be that cannabis in 2019 will be found to have fostered addictions as a gateway drug in the 2020s just as the liberal use of opioids in the 1980s for chronic pain lead to the present opioid crisis (269-271).
Should testosterone be replaced during opioid tapering?
Most potent mu agonists produce a central hypogonadism in men (272). A systematic review found that testosterone replacement reduces pain by 2 points on a numerical rating scale of 0–10. Testosterone replacement improved emotional functioning (273). However, replacement did not improve sleep quality, sexual function, physical functioning, role functioning, or social functioning; very low-quality evidence suggested no association with depressive symptoms. The evidence of benefit is quite low. There is no evidence pro-or con that testosterone replacement improves the success of tapering (273).
Are there benefits to psychosocial support and complementary therapies during opioid tapering?
Providing psychosocial support during tapering, referring patients for exercise and physical rehabilitation, using cognitive behavioral therapies to improve self-efficacy and recommending complementary therapies such as yoga and acupuncture may rationally facilitate opioid tapering (274,275). Individuals with aberrant opioid behaviors are much more likely to be referred for specialty substance use disorder treatment (adjusted OR =7.39) (276). These complementary and supportive therapies are low risk relative to opioid therapy. Employing individuals who have successfully tapered from opioids may provide very good support for patients going through the process (277). Unfortunately, there are few studies that have compared interdisciplinary approaches to standard medical tapering in individuals who do not have aberrant behaviors (278,279). There are limited published long-term outcomes to interdisciplinary programs. One program reported an abstinence rate of 78% at 6 months and a second a similar percentage at 1 year (82,103). However, for stable individuals interdisciplinary care does not improve psychological or physical function or improve return to work with or without opioids to any great extent than tapering alone (82,160). On the other hand, opioids do not impair pain rehabilitation, improvement in pain occurred even without tapering.
There is strong evidence for supportive cognitive behavioral therapy and interdisciplinary care for chronic pain, less supporting evidence for OUD and only weak evidence for interdisciplinary care for medical tapering (277,279-281). On the other hand, psychological support and cognitive behavioral therapies may be needed to address anxiety, mood, depression and provide adapting coping skills for those who may be chemically coping (142).
Medicolegal risks in tapering
Tapering opioids is not risk free. This may be as true in palliative care as in any other specialty. There are wide differences in the practice of universal precautions for patients who are cared for within palliative care. Few palliative care programs have written policies and standards regarding universal precautions (75). The CDC guidelines which includes the practice of universal precautions excluded palliative care. Yet the problems of chemical coping, OUD, addiction and diversion are not less in palliative care (282,283). Mitigating practices should continue during tapering as aberrant opioid behaviors may emerge during the weaning process. Unexpected urine toxicology findings are reported in up to half of patients in palliative care (76,77). Patients can develop worsening mood, depression and psychiatric illness including suicide ideation leading to a successful suicide if patients are not followed closely (71,284).
Opioid diversion is not well addressed in the literature. Patients may or may not have addiction who practice diversion. Diversion is frequently to family members and may be a “compassionate” sharing of pain medications during an illness or injury. Physicians need to educate patients and families that such a practice is dangerous and is considered a felony. Unused opioids need to be taken back to drug take back containers located in pharmacies. Alternatively, opioids may be used for income. In this situation, if physicians continue to prescribe, they will be contributing to a felony and contributing to community health risks. If patients are diverting, they obviously do not need the opioid as an analgesic. However, the decision to abruptly stop opioids for diversion should not be based on hear-say but on first-hand evidence. Individuals in hospice relatives who are diverting the patients’ opioids for personal use should not continue to provide the opioid to the patient but insist the patient be transferred to a safe location, usually an extended care facility or inpatient hospice, before continuing opioid therapy.
A legal action can occur as a result of on intentional overdose deaths or suicides. This can lead either to potential civil suits or investigations by licensing medical boards or federal agencies. Opioids are the most common pharmaceutical class involved in malpractice claims resulting in up to 1% of claims (142,285). The most common claim is failure to adequately verify the patient's prior medical history which may have included current drug and alcohol misuse. Though screening should have occurred while patients were on opioids prior to tapering, the emergence of an OUD while tapering force physicians to take a history of drug and alcohol use and a family history of addiction and find that such information was missing prior to initiating opioid therapy. Documentation of risk prior to opioid therapy and universal precautions through the tapering process is important in this regard.
Can primary care physician successfully taper patients?
Most patients with chronic pain on opioids are managed by primary care physicians. Hence many are prescribed opioids in primary care. There has been a decline in the average morphine equivalent daily dosage of Schedule II opioids per primary care physician (286). In a retrospective study which involved family physicians, a guided instruction in tapering opioids led to a 30% reduction in the number of patients taking more than 50 MEDD and 19% reduction in those on greater than 90 MEDD (287). The intervention was not odious but involved a 1-hour lecture on the CDC guidelines and role-playing a tapering protocol conversation.
Conclusions
The evidence for the benefit of tapering opioids is established in multiple studies. The mechanics of tapering have not been well studied. There is no data that pain worsens with tapering in the great majority and not infrequently pain improves with tapering. Quality of life and function also improve. Most patients remain stable psychologically during tapering, but a few develop depression, an OUD or CPD which may require an alternative strategy than simple tapering. Multiple medications are used to manage withdrawal symptoms. The use of cannabis to facilitate opioid tapering and abstinence is controversial and certainly not established. Primary care physicians who manage patients with chronic pain on opioids can successfully taper patients.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Mellar P. Davis) for the series “Opioid Utility the Other Half of Equianalgesia” published in Annals of Palliative Medicine. The article was sent for external peer review organized by the Guest Editor and the editorial office.
Conflicts of Interest: The series “Opioid Utility the Other Half of Equianalgesia” was commissioned by the editorial office without any funding or sponsorship. MPD serves as an unpaid Associate Editor-in-Chief of Annals of Palliative Medicine from Dec 2019 to Nov 2021 and served as the unpaid Guest Editor of the series. The other authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Dowell D, Haegerich TM, Chou R. Prescribing Opioids for Chronic Pain--Reply. JAMA 2016;316:774-5. [Crossref] [PubMed]
- Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain--United States, 2016. JAMA 2016;315:1624-45. [Crossref] [PubMed]
- Nelson DA, Bjarnadottir MV, Wolcott VL, et al. Stated Pain Levels, Opioid Prescription Volume, and Chronic Opioid Use Among United States Army Soldiers. Mil Med 2018;183:e322-9. [Crossref] [PubMed]
- Bartels K, Mayes LM, Dingmann C, et al. Opioid Use and Storage Patterns by Patients after Hospital Discharge following Surgery. PLoS One 2016;11:e0147972. [Crossref] [PubMed]
- Howard R, Englesbe M, Vu J. Opioid Prescription After Surgery-Reply. JAMA Surg 2019;154:675-6. [Crossref] [PubMed]
- Howard R, Fry B, Gunaseelan V, et al. Association of Opioid Prescribing With Opioid Consumption After Surgery in Michigan. JAMA Surg 2019;154:e184234. [Crossref] [PubMed]
- Rodgers J, Cunningham K, Fitzgerald K, et al. Opioid consumption following outpatient upper extremity surgery. J Hand Surg Am 2012;37:645-50. [Crossref] [PubMed]
- Monitto CL, Hsu A, Gao S, et al. Opioid Prescribing for the Treatment of Acute Pain in Children on Hospital Discharge. Anesth Analg 2017;125:2113-22. [Crossref] [PubMed]
- Miller GE, Moriya AS. Any Use and Frequent Use of Opioids among Non-Elderly Adults in 2015-2016, by Socioeconomic Characteristics. Statistical Brief (Medical Expenditure Panel Survey (US)). Rockville (MD), 2001.
- Levy B, Paulozzi L, Mack KA, et al. Trends in Opioid Analgesic-Prescribing Rates by Specialty, U.S., 2007-2012. Am J Prev Med 2015;49:409-13. [Crossref] [PubMed]
- Boudreau D, Von Korff M, Rutter CM, et al. Trends in long-term opioid therapy for chronic non-cancer pain. Pharmacoepidemiol Drug Saf 2009;18:1166-75. [Crossref] [PubMed]
- Welham GC, Mount JK, Gilson AM. Type and Frequency of Opioid Pain Medications Returned for Disposal. Drugs Real World Outcomes 2015;2:129-35. [Crossref] [PubMed]
- Koob GF. Hedonic Homeostatic Dysregulation as a Driver of Drug-Seeking Behavior. Drug Discov Today Dis Models 2008;5:207-15. [Crossref] [PubMed]
- Koob GF, Le Moal M. Review. Neurobiological mechanisms for opponent motivational processes in addiction. Philos Trans R Soc Lond B Biol Sci 2008;363:3113-23. [Crossref] [PubMed]
- Shurman J, Koob GF, Gutstein HB. Opioids, pain, the brain, and hyperkatifeia: a framework for the rational use of opioids for pain. Pain Med 2010;11:1092-8. [Crossref] [PubMed]
- Garland EL, Froeliger BE, Passik SD, et al. Attentional bias for prescription opioid cues among opioid dependent chronic pain patients. J Behav Med 2013;36:611-20. [Crossref] [PubMed]
- Garland EL, Froeliger B, Zeidan F, et al. The downward spiral of chronic pain, prescription opioid misuse, and addiction: cognitive, affective, and neuropsychopharmacologic pathways. Neurosci Biobehav Rev 2013;37:2597-607. [Crossref] [PubMed]
- Ballantyne JC. The brain on opioids. Pain 2018;159 Suppl 1:S24-30. [Crossref] [PubMed]
- Lubman DI, Allen NB, Peters LA, et al. Electrophysiological evidence that drug cues have greater salience than other affective stimuli in opiate addiction. J Psychopharmacol 2008;22:836-42. [Crossref] [PubMed]
- Lubman DI, Allen NB, Peters LA, et al. Electrophysiological evidence of the motivational salience of drug cues in opiate addiction. Psychol Med 2007;37:1203-9. [Crossref] [PubMed]
- Koob GF, Le Moal M. Addiction and the brain antireward system. Annu Rev Psychol 2008;59:29-53. [Crossref] [PubMed]
- Finan PH, Remeniuk B, Dunn KE. The risk for problematic opioid use in chronic pain: What can we learn from studies of pain and reward? Prog Neuropsychopharmacol Biol Psychiatry 2018;87:255-62. [Crossref] [PubMed]
- Moreno E, Quiroz C, Rea W, et al. Functional mu-Opioid-Galanin Receptor Heteromers in the Ventral Tegmental Area. J Neurosci 2017;37:1176-86. [Crossref] [PubMed]
- Cai NS, Quiroz C, Bonaventura J, et al. Opioid-galanin receptor heteromers mediate the dopaminergic effects of opioids. J Clin Invest 2019;129:2730-44. [Crossref] [PubMed]
- Koob GF. Neural substrates of opioid tolerance and dependence. NIDA Res Monogr 1987;76:46-52. [PubMed]
- Koob GF. Neural mechanisms of drug reinforcement. Ann N Y Acad Sci 1992;654:171-91. [Crossref] [PubMed]
- Koob GF. Drugs of abuse: anatomy, pharmacology and function of reward pathways. Trends Pharmacol Sci 1992;13:177-84. [Crossref] [PubMed]
- Koob GF. Neurobiological mechanisms in cocaine and opiate dependence. Res Publ Assoc Res Nerv Ment Dis 1992;70:79-92. [PubMed]
- Koob GF. Alcoholism: allostasis and beyond. Alcohol Clin Exp Res 2003;27:232-43. [Crossref] [PubMed]
- Koob GF. Neurobiological substrates for the dark side of compulsivity in addiction. Neuropharmacology 2009;56 Suppl 1:18-31. [Crossref] [PubMed]
- Hernandez G, Hamdani S, Rajabi H, et al. Prolonged rewarding stimulation of the rat medial forebrain bundle: neurochemical and behavioral consequences. Behav Neurosci 2006;120:888-904. [Crossref] [PubMed]
- Koob GF, Volkow ND. Neurobiology of addiction: a neurocircuitry analysis. Lancet Psychiatry 2016;3:760-73. [Crossref] [PubMed]
- Kenny PJ, Koob GF, Markou A. Conditioned facilitation of brain reward function after repeated cocaine administration. Behav Neurosci 2003;117:1103-7. [Crossref] [PubMed]
- Ballantyne JC, Sullivan MD, Koob GF. Refractory dependence on opioid analgesics. Pain 2019;160:2655-60. [Crossref] [PubMed]
- Pierce RC, Wolf ME. Psychostimulant-induced neuroadaptations in nucleus accumbens AMPA receptor transmission. Cold Spring Harb Perspect Med 2013;3:a012021. [Crossref] [PubMed]
- Lüscher C, Malenka RC. Drug-evoked synaptic plasticity in addiction: from molecular changes to circuit remodeling. Neuron 2011;69:650-63. [Crossref] [PubMed]
- Kalivas PW. The glutamate homeostasis hypothesis of addiction. Nat Rev Neurosci 2009;10:561-72. [Crossref] [PubMed]
- Nugent FS, Penick EC, Kauer JA. Opioids block long-term potentiation of inhibitory synapses. Nature 2007;446:1086-90. [Crossref] [PubMed]
- Kauer JA, Malenka RC. Synaptic plasticity and addiction. Nat Rev Neurosci 2007;8:844-58. [Crossref] [PubMed]
- Polter AM, Barcomb K, Chen RW, et al. Constitutive activation of kappa opioid receptors at ventral tegmental area inhibitory synapses following acute stress. Elife 2017. [Crossref] [PubMed]
- Wee S, Koob GF. The role of the dynorphin-kappa opioid system in the reinforcing effects of drugs of abuse. Psychopharmacology (Berl) 2010;210:121-35. [Crossref] [PubMed]
- Rorick-Kehn LM, Witcher JW, Lowe SL, et al. Determining pharmacological selectivity of the kappa opioid receptor antagonist LY2456302 using pupillometry as a translational biomarker in rat and human. Int J Neuropsychopharmacol 2014. [Crossref] [PubMed]
- Rorick-Kehn LM, Witkin JM, Statnick MA, et al. LY2456302 is a novel, potent, orally-bioavailable small molecule kappa-selective antagonist with activity in animal models predictive of efficacy in mood and addictive disorders. Neuropharmacology 2014;77:131-44. [Crossref] [PubMed]
- Karp JF, Butters MA, Begley AE, et al. Safety, tolerability, and clinical effect of low-dose buprenorphine for treatment-resistant depression in midlife and older adults. J Clin Psychiatry 2014;75:e785-93. [Crossref] [PubMed]
- Cordery SF, Taverner A, Ridzwan IE, et al. A non-rewarding, non-aversive buprenorphine/naltrexone combination attenuates drug-primed reinstatement to cocaine and morphine in rats in a conditioned place preference paradigm. Addict Biol 2014;19:575-86. [Crossref] [PubMed]
- Butler S. Buprenorphine-Clinically useful but often misunderstood. Scand J Pain 2013;4:148-52. [Crossref] [PubMed]
- Cao JL, Vialou VF, Lobo MK, et al. Essential role of the cAMP-cAMP response-element binding protein pathway in opiate-induced homeostatic adaptations of locus coeruleus neurons. Proc Natl Acad Sci U S A 2010;107:17011-6. [Crossref] [PubMed]
- Kalso E, Edwards JE, Moore RA, et al. Opioids in chronic non-cancer pain: systematic review of efficacy and safety. Pain 2004;112:372-80. [Crossref] [PubMed]
- Sullivan MD. Who gets high-dose opioid therapy for chronic non-cancer pain? Pain 2010;151:567-68. [Crossref] [PubMed]
- Antoniou T, Ala-Leppilampi K, Shearer D, et al. "Like being put on an ice floe and shoved away": A qualitative study of the impacts of opioid-related policy changes on people who take opioids. Int J Drug Policy 2019;66:15-22. [Crossref] [PubMed]
- Faour M, Anderson JT, Haas AR, et al. Prolonged Preoperative Opioid Therapy Associated With Poor Return to Work Rates After Single-Level Cervical Fusion for Radiculopathy for Patients Receiving Workers' Compensation Benefits. Spine (Phila Pa 1976) 2017;42:E104-10. [Crossref] [PubMed]
- Steenstra IA, Busse JW, Tolusso D, et al. Predicting time on prolonged benefits for injured workers with acute back pain. J Occup Rehabil 2015;25:267-78. [Crossref] [PubMed]
- Kidner CL, Mayer TG, Gatchel RJ. Higher opioid doses predict poorer functional outcome in patients with chronic disabling occupational musculoskeletal disorders. J Bone Joint Surg Am 2009;91:919-27. [Crossref] [PubMed]
- Janakiram C, Fontelo P, Huser V, et al. Opioid Prescriptions for Acute and Chronic Pain Management Among Medicaid Beneficiaries. Am J Prev Med 2019;57:365-73. [Crossref] [PubMed]
- Brennan MJ, Gudin JA. The prescription opioid conundrum: 21st century solutions to a millennia-long problem. Postgrad Med 2020;132:17-27. [Crossref] [PubMed]
- Shah R, Chou LN, Kuo YF, et al. Long-Term Opioid Therapy in Older Cancer Survivors: A Retrospective Cohort Study. J Am Geriatr Soc 2019;67:945-52. [Crossref] [PubMed]
- Bennett MI, Kaasa S, Barke A, et al. The IASP classification of chronic pain for ICD-11: chronic cancer-related pain. Pain 2019;160:38-44. [Crossref] [PubMed]
- Schreier AM, Johnson LA, Vohra NA, et al. Post-Treatment Symptoms of Pain, Anxiety, Sleep Disturbance, and Fatigue in Breast Cancer Survivors. Pain Manag Nurs 2019;20:146-51. [Crossref] [PubMed]
- Merlin JS, Patel K, Thompson N, et al. Managing Chronic Pain in Cancer Survivors Prescribed Long-Term Opioid Therapy: A National Survey of Ambulatory Palliative Care Providers. J Pain Symptom Manage 2019;57:20-7. [Crossref] [PubMed]
- Leysen L, Adriaenssens N, Nijs J, et al. Chronic Pain in Breast Cancer Survivors: Nociceptive, Neuropathic, or Central Sensitization Pain? Pain Pract 2019;19:183-95. [Crossref] [PubMed]
- Whitney CA, Dorfman CS, Shelby RA, et al. Reminders of cancer risk and pain catastrophizing: relationships with cancer worry and perceived risk in women with a first-degree relative with breast cancer. Fam Cancer 2019;18:9-18. [Crossref] [PubMed]
- Zhi WI, Chen P, Kwon A, et al. Chemotherapy-induced peripheral neuropathy (CIPN) in breast cancer survivors: a comparison of patient-reported outcomes and quantitative sensory testing. Breast Cancer Res Treat 2019;178:587-95. [Crossref] [PubMed]
- Coffeen U, Sotomayor-Sobrino MA, Jimenez-Gonzalez A, et al. Chemotherapy-induced neuropathic pain characteristics in Mexico's National Cancer Center pain clinic. J Pain Res 2019;12:1331-9. [Crossref] [PubMed]
- Kanzawa-Lee GA, Knoerl R, Donohoe C, et al. Mechanisms, Predictors, and Challenges in Assessing and Managing Painful Chemotherapy-Induced Peripheral Neuropathy. Semin Oncol Nurs 2019;35:253-60. [Crossref] [PubMed]
- Ward K, Ramzan A, Sheeder J, et al. Persistent opioid use after radiation therapy in opioid-naive cervical cancer survivors. Int J Gynecol Cancer 2019;29:1105-9. [Crossref] [PubMed]
- Davis MP, Mehta Z. Opioids and Chronic Pain: Where Is the Balance? Curr Oncol Rep 2016;18:71. [Crossref] [PubMed]
- Paice JA, Portenoy R, Lacchetti C, et al. Management of Chronic Pain in Survivors of Adult Cancers: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol 2016;34:3325-45. [Crossref] [PubMed]
- Paice JA. Cancer Pain Management: Strategies for Safe and Effective Opioid Prescribing. J Natl Compr Canc Netw 2016;14:695-7. [Crossref] [PubMed]
- Paice JA. Managing Pain in Patients and Survivors: Challenges Within the United States Opioid Crisis. J Natl Compr Canc Netw 2019;17:595-8. [PubMed]
- Paice JA. Pain in Cancer Survivors: How to Manage. Curr Treat Options Oncol 2019;20:48. [Crossref] [PubMed]
- Goodlev ER, Discala S, Darnall BD, et al. Managing Cancer Pain, Monitoring for Cancer Recurrence, and Mitigating Risk of Opioid Use Disorders: A Team-Based, Interdisciplinary Approach to Cancer Survivorship. J Palliat Med 2019;22:1308-17. [Crossref] [PubMed]
- Khatcheressian JL, Hurley P, Bantug E, et al. Breast cancer follow-up and management after primary treatment: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol 2013;31:961-5. [Crossref] [PubMed]
- Salani R, Nagel CI, Drennen E, et al. Recurrence patterns and surveillance for patients with early stage endometrial cancer. Gynecol Oncol 2011;123:205-7. [Crossref] [PubMed]
- Meyerhardt JA, Mangu PB, Flynn PJ, et al. Follow-up care, surveillance protocol, and secondary prevention measures for survivors of colorectal cancer: American Society of Clinical Oncology clinical practice guideline endorsement. J Clin Oncol 2013;31:4465-70. [Crossref] [PubMed]
- Tan PD, Barclay JS, Blackhall LJ. Do Palliative Care Clinics Screen for Substance Abuse and Diversion? Results of a National Survey. J Palliat Med 2015;18:752-7. [Crossref] [PubMed]
- Childers JW, King LA, Arnold RM. Chronic Pain and Risk Factors for Opioid Misuse in a Palliative Care Clinic. Am J Hosp Palliat Care 2015;32:654-9. [Crossref] [PubMed]
- Barclay JS, Owens JE, Blackhall LJ. Screening for substance abuse risk in cancer patients using the Opioid Risk Tool and urine drug screen. Support Care Cancer 2014;22:1883-8. [Crossref] [PubMed]
- Fürst CJ, Lindqvist O, Tishelman C. Towards a basic drug kit for the dying patient. Curr Opin Support Palliat Care 2012;6:386-90. [Crossref] [PubMed]
- Curtis HJ, Croker R, Walker AJ, et al. Opioid prescribing trends and geographical variation in England, 1998-2018: a retrospective database study. Lancet Psychiatry 2019;6:140-50. [Crossref] [PubMed]
- Neprash HT, Barnett ML. Association of Primary Care Clinic Appointment Time With Opioid Prescribing. JAMA Netw Open 2019;2:e1910373. [Crossref] [PubMed]
- Bicket MC, Murimi IB, Mansour O, et al. Association of new opioid continuation with surgical specialty and type in the United States. Am J Surg 2019;218:818-27. [Crossref] [PubMed]
- Townsend CO, Kerkvliet JL, Bruce BK, et al. A longitudinal study of the efficacy of a comprehensive pain rehabilitation program with opioid withdrawal: comparison of treatment outcomes based on opioid use status at admission. Pain 2008;140:177-89. [Crossref] [PubMed]
- Pergolizzi JV Jr, Rosenblatt M, Mariano DJ, et al. Tapering opioid therapy: clinical strategies. Pain Manag 2018;8:409-13. [Crossref] [PubMed]
- Darnall BD, Humphreys KN. An experimental method for assessing whether marijuana use reduces opioid use in patients with chronic pain. Addiction 2018;113:1552-3. [Crossref] [PubMed]
- Campbell G, Bruno R, Darke S, et al. Associations of borderline personality with pain, problems with medications and suicidality in a community sample of chronic non-cancer pain patients prescribed opioids for pain. Gen Hosp Psychiatry 2015;37:434-40. [Crossref] [PubMed]
- Larson MJ, Paasche-Orlow M, Cheng DM, et al. Persistent pain is associated with substance use after detoxification: a prospective cohort analysis. Addiction 2007;102:752-60. [Crossref] [PubMed]
- Zhou K, Jia P, Bhargava S, et al. Opioid tapering in patients with prescription opioid use disorder: A retrospective study. Scand J Pain 2017;17:167-73. [Crossref] [PubMed]
- Elman I, Borsook D. The failing cascade: Comorbid post traumatic stress- and opioid use disorders. Neurosci Biobehav Rev 2019;103:374-83. [Crossref] [PubMed]
- Lei Y, Xi C, Li P, et al. Association between childhood maltreatment and non-medical prescription opioid use among Chinese senior high school students: The moderating role of gender. J Affect Disord 2018;235:421-7. [Crossref] [PubMed]
- Heffernan K, Cloitre M, Tardiff K, et al. Childhood trauma as a correlate of lifetime opiate use in psychiatric patients. Addict Behav 2000;25:797-803. [Crossref] [PubMed]
- Austin AE, Shanahan ME, Zvara BJ. Association of childhood abuse and prescription opioid use in early adulthood. Addict Behav 2018;76:265-9. [Crossref] [PubMed]
- Kendler KS, Bulik CM, Silberg J, et al. Childhood sexual abuse and adult psychiatric and substance use disorders in women: an epidemiological and cotwin control analysis. Arch Gen Psychiatry 2000;57:953-9. [Crossref] [PubMed]
- Merikangas KR, Stolar M, Stevens DE, et al. Familial transmission of substance use disorders. Arch Gen Psychiatry 1998;55:973-9. [Crossref] [PubMed]
- Fareed A, Eilender P, Haber M, et al. Comorbid posttraumatic stress disorder and opiate addiction: a literature review. J Addict Dis 2013;32:168-79. [Crossref] [PubMed]
- Lagisetty PA, Lin LA, Ganoczy D, et al. Opioid Prescribing After Opioid-related Inpatient Hospitalizations by Diagnosis: A Cohort Study. Med Care 2019;57:815-21. [Crossref] [PubMed]
- Murphy L, Babaei-Rad R, Buna D, et al. Guidance on opioid tapering in the context of chronic pain: Evidence, practical advice and frequently asked questions. Can Pharm J (Ott) 2018;151:114-20. [Crossref] [PubMed]
- Heiwe S, Lonnquist I, Kallmen H. Potential risk factors associated with risk for drop-out and relapse during and following withdrawal of opioid prescription medication. Eur J Pain 2011;15:966-70. [Crossref] [PubMed]
- Scherrer JF, Salas J, Sullivan MD, et al. Impact of adherence to antidepressants on long-term prescription opioid use cessation. Br J Psychiatry 2018;212:103-11. [Crossref] [PubMed]
- Krumova EK, Bennemann P, Kindler D, et al. Low pain intensity after opioid withdrawal as a first step of a comprehensive pain rehabilitation program predicts long-term nonuse of opioids in chronic noncancer pain. Clin J Pain 2013;29:760-9. [Crossref] [PubMed]
- Tennant FS Jr, Rawson RA. Outpatient treatment of prescription opioid dependence: comparison of two methods. Arch Intern Med 1982;142:1845-7. [Crossref] [PubMed]
- Blondell RD, Ashrafioun L, Dambra CM, et al. A Clinical Trial Comparing Tapering Doses of Buprenorphine with Steady Doses for Chronic Pain and Co-existent Opioid Addiction. J Addict Med 2010;4:140-6. [Crossref] [PubMed]
- Vowles KE, Ashworth J. Is opioid withdrawal necessary within comprehensive pain rehabilitation programs? Pain 2011;152:1948-50. [Crossref] [PubMed]
- Huffman KL, Sweis GW, Gase A, et al. Opioid use 12 months following interdisciplinary pain rehabilitation with weaning. Pain Med 2013;14:1908-17. [Crossref] [PubMed]
- Zale EL, Dorfman ML, Hooten WM, et al. Tobacco smoking, nicotine dependence, and patterns of prescription opioid misuse: results from a nationally representative sample. Nicotine Tob Res 2015;17:1096-103. [Crossref] [PubMed]
- Manhapra A, Arias AJ, Ballantyne JC. The conundrum of opioid tapering in long-term opioid therapy for chronic pain: A commentary. Subst Abus 2018;39:152-61. [Crossref] [PubMed]
- Sullivan MD, Ballantyne JC. What are we treating with long-term opioid therapy? Arch Intern Med 2012;172:433-4. [Crossref] [PubMed]
- Garland EL, Brown SM, Howard MO. Thought suppression as a mediator of the association between depressed mood and prescription opioid craving among chronic pain patients. J Behav Med 2016;39:128-38. [Crossref] [PubMed]
- McPherson S, Lederhos Smith C, Dobscha SK, et al. Changes in pain intensity after discontinuation of long-term opioid therapy for chronic noncancer pain. Pain 2018;159:2097-104. [Crossref] [PubMed]
- Fishbain DA, Pulikal A. Does Opioid Tapering in Chronic Pain Patients Result in Improved Pain or Same Pain vs Increased Pain at Taper Completion? A Structured Evidence-Based Systematic Review. Pain Med 2019;20:2179-97. [Crossref] [PubMed]
- Nilsen HK, Stiles TC, Landro NI, et al. Patients with problematic opioid use can be weaned from codeine without pain escalation. Acta Anaesthesiol Scand 2010;54:571-9. [Crossref] [PubMed]
- Ralphs JA, Williams AC, Richardson PH, et al. Opiate reduction in chronic pain patients: a comparison of patient-controlled reduction and staff controlled cocktail methods. Pain 1994;56:279-88. [Crossref] [PubMed]
- Baron MJ, McDonald PW. Significant pain reduction in chronic pain patients after detoxification from high-dose opioids. J Opioid Manag 2006;2:277-82. [Crossref] [PubMed]
- Hooten WM. Commentary: the paradox of analgesic medication elimination. Pain Med 2009;10:797-8. [Crossref] [PubMed]
- Darnall BD, Ziadni MS, Stieg RL, et al. Patient-Centered Prescription Opioid Tapering in Community Outpatients With Chronic Pain. JAMA Intern Med 2018;178:707-8. [Crossref] [PubMed]
- Frank JW, Levy C, Matlock DD, et al. Patients' Perspectives on Tapering of Chronic Opioid Therapy: A Qualitative Study. Pain Med 2016;17:1838-47. [Crossref] [PubMed]
- Lovejoy TI, Morasco BJ, Demidenko MI, et al. Reasons for discontinuation of long-term opioid therapy in patients with and without substance use disorders. Pain 2017;158:526-34. [Crossref] [PubMed]
- Sullivan MD, Turner JA, DiLodovico C, et al. Prescription opioid taper support for outpatients with chronic pain: a randomized controlled trial. J Pain 2017;18:308-318. [Crossref] [PubMed]
- Mark TL, Parish W. Opioid medication discontinuation and risk of adverse opioid-related health care events. J Subst Abuse Treat 2019;103:58-63. [Crossref] [PubMed]
- Krebs EE, Gravely A, Nugent S, et al. Effect of Opioid vs Nonopioid Medications on Pain-Related Function in Patients With Chronic Back Pain or Hip or Knee Osteoarthritis Pain: The SPACE Randomized Clinical Trial. JAMA 2018;319:872-82. [Crossref] [PubMed]
- Chapman CR, Fosnocht D, Donaldson GW. Resolution of acute pain following discharge from the emergency department: the acute pain trajectory. J Pain 2012;13:235-41. [Crossref] [PubMed]
- Weissman DE, Haddox JD. Opioid pseudoaddiction--an iatrogenic syndrome. Pain 1989;36:363-6. [Crossref] [PubMed]
- Kiepek N, Hancock L, Toppozini D, et al. Facilitating medical withdrawal from opiates in rural Ontario. Rural Remote Health 2012;12:2193. [PubMed]
- Pergolizzi JV, Varrassi G, Paladini A, et al. Stopping or Decreasing Opioid Therapy in Patients on Chronic Opioid Therapy. Pain Ther 2019;8:163-76. [Crossref] [PubMed]
- Kennedy LC, Binswanger IA, Mueller SR, et al. "Those Conversations in My Experience Don't Go Well": A Qualitative Study of Primary Care Provider Experiences Tapering Long-term Opioid Medications. Pain Med 2018;19:2201-11. [Crossref] [PubMed]
- Matthias MS, Johnson NL, Shields CG, et al. "I'm Not Gonna Pull the Rug out From Under You": Patient-Provider Communication About Opioid Tapering. J Pain 2017;18:1365-73. [Crossref] [PubMed]
- Passik SD. Issues in long-term opioid therapy: unmet needs, risks, and solutions. Mayo Clin Proc 2009;84:593-601. [Crossref] [PubMed]
- Hutchinson K, Moreland AM. Exploring beliefs and practice of opioid prescribing for persistent non-cancer pain by general practitioners. Eur J Pain 2007;11:93-8. [Crossref] [PubMed]
- García MC, Heilig CM, Lee SH, et al. Opioid Prescribing Rates in Nonmetropolitan and Metropolitan Counties Among Primary Care Providers Using an Electronic Health Record System - United States, 2014-2017. MMWR Morb Mortal Wkly Rep 2019;68:25-30. [Crossref] [PubMed]
- Sherman KJ, Walker RL, Saunders K, et al. Doctor-Patient Trust Among Chronic Pain Patients on Chronic Opioid Therapy after Opioid Risk Reduction Initiatives: A Survey. J Am Board Fam Med 2018;31:578-87. [Crossref] [PubMed]
- Penney LS, Ritenbaugh C, DeBar LL, et al. Provider and patient perspectives on opioids and alternative treatments for managing chronic pain: a qualitative study. BMC Fam Pract 2017;17:164. [Crossref] [PubMed]
- Peppin JF. The marginalization of chronic pain patients on chronic opioid therapy. Pain Physician 2009;12:493-498. [PubMed]
- Hooten WM, Dvorkin J, Warner NS, et al. Characteristics of physicians who prescribe opioids for chronic pain: a meta-narrative systematic review. J Pain Res 2019;12:2261-89. [Crossref] [PubMed]
- Perez HR, Buonora M, Cunningham CO, et al. Opioid Taper Is Associated with Subsequent Termination of Care: a Retrospective Cohort Study. J Gen Intern Med 2020;35:36-42. [Crossref] [PubMed]
- Holliday SM, Hayes C, Dunlop AJ, et al. Does brief chronic pain management education change opioid prescribing rates? A pragmatic trial in Australian early-career general practitioners. Pain 2017;158:278-88. [Crossref] [PubMed]
- McCalmont JC, Jones KD, Bennett RM, et al. Does familiarity with CDC guidelines, continuing education, and provider characteristics influence adherence to chronic pain management practices and opioid prescribing? J Opioid Manag 2018;14:103-16. [Crossref] [PubMed]
- Henry SG, Paterniti DA, Feng B, et al. Patients' experience with opioid tapering: a conceptual model with recommendations for clinicians. J Pain 2019;20:181-91. [Crossref] [PubMed]
- Kostopoulos D. Non-prescription medication providers fight the opioid crisis with use of diagnostic testing. J Bodyw Mov Ther 2019;23:581-2. [Crossref] [PubMed]
- Casey DE Jr. Why don't physicians (and patients) consistently follow clinical practice guidelines? JAMA Intern Med 2013;173:1581-3. [Crossref] [PubMed]
- Kirane H, Drits E, Ahn S, et al. Addressing the opioid crisis: An assessment of clinicians' training experience, practices, and attitudes within a large healthcare organization. J Opioid Manag 2019;15:193-204. [Crossref] [PubMed]
- White R, Hayes C, Boyes AW, et al. General practitioners and management of chronic noncancer pain: a cross-sectional survey of influences on opioid deprescribing. J Pain Res 2019;12:467-75. [Crossref] [PubMed]
- Coluzzi F, Taylor R Jr, Pergolizzi JV Jr, et al. Good clinical practice guide for opioids in pain management: the three Ts - titration (trial), tweaking (tailoring), transition (tapering). Braz J Anesthesiol 2016;66:310-7. [Crossref] [PubMed]
- Berna C, Kulich RJ, Rathmell JP. Tapering Long-term Opioid Therapy in Chronic Noncancer Pain: Evidence and Recommendations for Everyday Practice. Mayo Clin Proc 2015;90:828-42. [Crossref] [PubMed]
- Singh J, Basu D. Ultra-rapid opioid detoxification: current status and controversies. J Postgrad Med 2004;50:227-32. [PubMed]
- Gomes T, Mamdani MM, Dhalla IA, et al. Opioid dose and drug-related mortality in patients with nonmalignant pain. Arch Intern Med 2011;171:686-91. [Crossref] [PubMed]
- Fishbain DA, Rosomoff HL, Cutler R. Opiate detoxification protocols. A clinical manual. Ann Clin Psychiatry 1993;5:53-65. [Crossref] [PubMed]
- Bienek N, Maier C, Kaisler M, et al. Intensity of Withdrawal Symptoms During Opioid Taper in Patients with Chronic Pain-Individualized or Fixed Starting Dosage? Pain Med 2019;20:2438-49. [Crossref] [PubMed]
- Collins ED, Kleber HD, Whittington RA, et al. Anesthesia-assisted vs buprenorphine- or clonidine-assisted heroin detoxification and naltrexone induction: a randomized trial. JAMA 2005;294:903-13. [Crossref] [PubMed]
- Maani CV, DeSocio PA, Jansen RK, et al. Use of ultra rapid opioid detoxification in the treatment of US military burn casualties. J Trauma 2011;71:S114-9. [Crossref] [PubMed]
- Monterubbianesi MC, Capuccini J, Ferioli I, et al. High opioid dosage rapid detoxification of cancer patient in palliative care with the Raffaeli model. J Opioid Manag 2012;8:292-8. [Crossref] [PubMed]
- Spadotto V, Zorzi A, Elmaghawry M, et al. Heart failure due to 'stress cardiomyopathy': a severe manifestation of the opioid withdrawal syndrome. Eur Heart J Acute Cardiovasc Care 2013;2:84-7. [Crossref] [PubMed]
- Rivera JM, Locketz AJ, Fritz KD, et al. "Broken heart syndrome" after separation (from OxyContin). Mayo Clin Proc 2006;81:825-8. [Crossref] [PubMed]
- Geller AS. Patient and Public Safety Maximized by Rapid Opioid Taper. JAMA Intern Med 2017;177:895-6. [Crossref] [PubMed]
- Gowing L, Farrell M, Ali R, et al. Alpha(2)-adrenergic agonists for the management of opioid withdrawal. Cochrane Database Syst Rev 2016.CD002024. [PubMed]
- Hegmann KT, Weiss MS, Bowden K, et al. ACOEM practice guidelines: opioids and safety-sensitive work. J Occup Environ Med. 2014;56:e46-53. [Crossref] [PubMed]
- Sakamoto A, Takayama H, Mamiya K, et al. Opioid withdrawal presenting only nausea during tapering of oxycodone after celiac plexus block: a case report. Ann Palliat Med. 2016;5:67-70. [PubMed]
- Paice JA. Risk Assessment and Monitoring of Patients with Cancer Receiving Opioid Therapy. Oncologist 2019;24:1294-8. [Crossref] [PubMed]
- Holliday S, Hayes C, Dunlop A. Opioid use in chronic non-cancer pain--part 2: prescribing issues and alternatives. Aust Fam Physician 2013;42:104-11. [PubMed]
- Hahn KL. Strategies to prevent opioid misuse, abuse, and diversion that may also reduce the associated costs. Am Health Drug Benefits 2011;4:107-14. [PubMed]
- Hooten WM, Townsend CO, Sletten CD, et al. Treatment outcomes after multidisciplinary pain rehabilitation with analgesic medication withdrawal for patients with fibromyalgia. Pain Med 2007;8:8-16. [Crossref] [PubMed]
- Rome JD, Townsend CO, Bruce BK, et al. Chronic noncancer pain rehabilitation with opioid withdrawal: comparison of treatment outcomes based on opioid use status at admission. Mayo Clin Proc 2004;79:759-68. [Crossref] [PubMed]
- Madlung-Kratzer E, Spitzer B, Brosch R, et al. A double-blind, randomized, parallel group study to compare the efficacy, safety and tolerability of slow-release oral morphine versus methadone in opioid-dependent in-patients willing to undergo detoxification. Addiction 2009;104:1549-57. [Crossref] [PubMed]
- Senay EC, Dorus W, Goldberg F, et al. Withdrawal from methadone maintenance. Rate of withdrawal and expectation. Arch Gen Psychiatry 1977;34:361-7. [Crossref] [PubMed]
- Busse JW, Craigie S, Juurlink DN, et al. Guideline for opioid therapy and chronic noncancer pain. CMAJ 2017;189:E659-66. [Crossref] [PubMed]
- Mattick RP, Breen C, Kimber J, et al. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev 2014.CD002207. [PubMed]
- Treillet E, Laurent S, Hadjiat Y. Practical management of opioid rotation and equianalgesia. J Pain Res 2018;11:2587-601. [Crossref] [PubMed]
- Rennick A, Atkinson T, Cimino NM, et al. Variability in Opioid Equivalence Calculations. Pain Med 2016;17:892-8. [PubMed]
- Fudin J, Pratt Cleary J, Schatman ME. The MEDD myth: the impact of pseudoscience on pain research and prescribing-guideline development. J Pain Res 2016;9:153-6. [PubMed]
- Bhimji K. Opioid rotation from methadone: fraught with difficulties. J Pain Symptom Manage 2005;29:334-5. [Crossref] [PubMed]
- Walker PW, Palla S, Pei BL, et al. Switching from methadone to a different opioid: what is the equianalgesic dose ratio? J Palliat Med 2008;11:1103-8. [Crossref] [PubMed]
- Zedler B, Xie L, Wang L, et al. Development of a Risk Index for Serious Prescription Opioid-Induced Respiratory Depression or Overdose in Veterans' Health Administration Patients. Pain Med 2015;16:1566-79. [Crossref] [PubMed]
- Chou R. 2009 Clinical Guidelines from the American Pain Society and the American Academy of Pain Medicine on the use of chronic opioid therapy in chronic noncancer pain: what are the key messages for clinical practice? Pol Arch Med Wewn 2009;119:469-77. [PubMed]
- Tallgren M, Olkkola KT, Seppala T, et al. Pharmacokinetics and ventilatory effects of oxycodone before and after liver transplantation. Clin Pharmacol Ther 1997;61:655-61. [Crossref] [PubMed]
- Tegeder I, Lotsch J, Geisslinger G. Pharmacokinetics of opioids in liver disease. Clin Pharmacokinet 1999;37:17-40. [Crossref] [PubMed]
- Vozoris NT, Wang X, Fischer HD, et al. Incident opioid drug use and adverse respiratory outcomes among older adults with COPD. Eur Respir J 2016;48:683-93. [Crossref] [PubMed]
- Solassol I, Caumette L, Bressolle F, et al. Inter- and intra-individual variability in transdermal fentanyl absorption in cancer pain patients. Oncol Rep 2005;14:1029-36. [PubMed]
- Solassol I, Bressolle F, Caumette L, et al. Inter- and intraindividual variabilities in pharmacokinetics of fentanyl after repeated 72-hour transdermal applications in cancer pain patients. Ther Drug Monit 2005;27:491-8. [Crossref] [PubMed]
- Weiss RD, Potter JS, Fiellin DA, et al. Adjunctive counseling during brief and extended buprenorphine-naloxone treatment for prescription opioid dependence: a 2-phase randomized controlled trial. Arch Gen Psychiatry 2011;68:1238-46. [Crossref] [PubMed]
- Cheatle MD. The Impact of Prescription Drug Monitoring Programs and Prescribing Guidelines on Opioid Prescribing Behaviors: A Time for Institutional and Regulatory Changes. Pain Med 2017;18:823-4. [Crossref] [PubMed]
- Banta-Green CJ, Merrill JO, Doyle SR, et al. Measurement of opioid problems among chronic pain patients in a general medical population. Drug Alcohol Depend 2009;104:43-9. [Crossref] [PubMed]
- Demidenko MI, Dobscha SK, Morasco BJ, et al. Suicidal ideation and suicidal self-directed violence following clinician-initiated prescription opioid discontinuation among long-term opioid users. Gen Hosp Psychiatry 2017;47:29-35. [Crossref] [PubMed]
- Kertesz SG, Satel SL, DeMicco J, et al. Opioid discontinuation as an institutional mandate: Questions and answers on why we wrote to the Centers for Disease Control and Prevention. Subst Abus 2019;40:4-6. [Crossref] [PubMed]
- Kertesz SG, Satel SL, DeMicco J, et al. Opioid discontinuation as an institutional mandate: Questions and answers on why we wrote to the Centers for Disease Control and Prevention. Subst Abus 2019.1-3.
- Frank JW, Lovejoy TI, Becker WC, et al. Patient Outcomes in Dose Reduction or Discontinuation of Long-Term Opioid Therapy: A Systematic Review. Ann Intern Med 2017;167:181-91. [Crossref] [PubMed]
- Dowell D, Haegerich T, Chou R. No Shortcuts to Safer Opioid Prescribing. N Engl J Med 2019;380:2285-7. [Crossref] [PubMed]
- Artenie AA, Bruneau J. The authors respond to "Opioid agonist dosage adequacy from clinical and patient perspectives: further considerations". CMAJ 2019;191:E1085. [Crossref] [PubMed]
- Artenie AA, Minoyan N, Jacka B, et al. Opioid agonist treatment dosage and patient-perceived dosage adequacy, and risk of hepatitis C infection among people who inject drugs. CMAJ 2019;191:E462-8. [Crossref] [PubMed]
- Fiellin DA, Schottenfeld RS, Cutter CJ, et al. Primary care-based buprenorphine taper vs maintenance therapy for prescription opioid dependence: a randomized clinical trial. JAMA Intern Med 2014;174:1947-54. [Crossref] [PubMed]
- Gowing L, Ali R, White JM. Buprenorphine for the management of opioid withdrawal. Cochrane Database Syst Rev 2009.CD002025. [PubMed]
- Fredheim OM, Moksnes K, Borchgrevink PC, et al. Clinical pharmacology of methadone for pain. Acta Anaesthesiol Scand 2008;52:879-89. [Crossref] [PubMed]
- Kampman K, Jarvis M. American Society of Addiction Medicine (ASAM) National Practice Guideline for the Use of Medications in the Treatment of Addiction Involving Opioid Use. J Addict Med 2015;9:358-67. [Crossref] [PubMed]
- Webster L, Gruener D, Kirby T, et al. Evaluation of the Tolerability of Switching Patients on Chronic Full mu-Opioid Agonist Therapy to Buccal Buprenorphine. Pain Med 2016;17:899-907. [PubMed]
- Veilleux JC, Colvin PJ, Anderson J, et al. A review of opioid dependence treatment: pharmacological and psychosocial interventions to treat opioid addiction. Clin Psychol Rev 2010;30:155-66. [Crossref] [PubMed]
- George O, Le Moal M, Koob GF. Allostasis and addiction: role of the dopamine and corticotropin-releasing factor systems. Physiol Behav 2012;106:58-64. [Crossref] [PubMed]
- Ahmed SH, Kenny PJ, Koob GF, et al. Neurobiological evidence for hedonic allostasis associated with escalating cocaine use. Nat Neurosci 2002;5:625-6. [Crossref] [PubMed]
- Koob GF, Le Moal M. Drug addiction, dysregulation of reward, and allostasis. Neuropsychopharmacology 2001;24:97-129. [Crossref] [PubMed]
- Berland DW, Malinoff HL, Weiner MA, et al. When opioids fail in chronic pain management: the role for buprenorphine and hospitalization. Am J Ther 2013;20:316-21. [Crossref] [PubMed]
- Foster B, Twycross R, Mihalyo M, et al. Buprenorphine. J Pain Symptom Manage 2013;45:939-49. [Crossref] [PubMed]
- Northrup TF, Stotts AL, Green C, et al. Opioid withdrawal, craving, and use during and after outpatient buprenorphine stabilization and taper: a discrete survival and growth mixture model. Addict Behav 2015;41:20-8. [Crossref] [PubMed]
- Moss C, Bossano C, Patel S, et al. Weaning from long-term opioid therapy. Clin Obstet Gynecol 2019;62:98-109. [Crossref] [PubMed]
- Jones JD, Madera G, Comer SD. The reinforcing and subjective effects of intravenous and intranasal buprenorphine in heroin users. Pharmacol Biochem Behav 2014;122:299-306. [Crossref] [PubMed]
- Jones JD, Sullivan MA, Vosburg SK, et al. Abuse potential of intranasal buprenorphine versus buprenorphine/naloxone in buprenorphine-maintained heroin users. Addict Biol 2015;20:784-98. [Crossref] [PubMed]
- Jones JD, Manubay JM, Mogali S, et al. Abuse liability of intravenous buprenorphine vs. buprenorphine/naloxone: Importance of absolute naloxone amount. Drug Alcohol Depend 2017;179:362-9. [Crossref] [PubMed]
- Sigmon SC, Dunn KE, Saulsgiver K, et al. A randomized, double-blind evaluation of buprenorphine taper duration in primary prescription opioid abusers. JAMA Psychiatry 2013;70:1347-54. [Crossref] [PubMed]
- Kosten TR, Baxter LE. Review article: Effective management of opioid withdrawal symptoms: A gateway to opioid dependence treatment. Am J Addict 2019;28:55-62. [Crossref] [PubMed]
- Gorodetzky CW, Walsh SL, Martin PR, et al. A phase III, randomized, multi-center, double blind, placebo controlled study of safety and efficacy of lofexidine for relief of symptoms in individuals undergoing inpatient opioid withdrawal. Drug Alcohol Depend 2017;176:79-88. [Crossref] [PubMed]
- Farrell M. Opiate withdrawal. Addiction 1994;89:1471-5. [Crossref] [PubMed]
- Fishbain DA, Goldberg M, Rosomoff RS, et al. Atypical withdrawal syndrome (organic delusional syndrome) secondary to oxycodone detoxification. J Clin Psychopharmacol 1988;8:441-2. [Crossref] [PubMed]
- Cowan DT, Wilson-Barnett J, Griffiths P, et al. A randomized, double-blind, placebo-controlled, cross-over pilot study to assess the effects of long-term opioid drug consumption and subsequent abstinence in chronic noncancer pain patients receiving controlled-release morphine. Pain Med 2005;6:113-21. [Crossref] [PubMed]
- Mattick RP, Hall W. Are detoxification programmes effective? Lancet 1996;347:97-100. [Crossref] [PubMed]
- Younger J, Barelka P, Carroll I, et al. Reduced cold pain tolerance in chronic pain patients following opioid detoxification. Pain Med 2008;9:1158-63. [Crossref] [PubMed]
- Hooten WM, Mantilla CB, Sandroni P, et al. Associations between heat pain perception and opioid dose among patients with chronic pain undergoing opioid tapering. Pain Med 2010;11:1587-98. [Crossref] [PubMed]
- Wang H, Akbar M, Weinsheimer N, et al. Longitudinal observation of changes in pain sensitivity during opioid tapering in patients with chronic low-back pain. Pain Med 2011;12:1720-6. [Crossref] [PubMed]
- Sandhu H, Underwood M, Furlan AD, et al. What interventions are effective to taper opioids in patients with chronic pain? BMJ 2018;362:k2990. [Crossref] [PubMed]
- Gowing L, Ali R, White JM, et al. Buprenorphine for managing opioid withdrawal. Cochrane Database Syst Rev 2017;2:CD002025. [PubMed]
- Ayanga D, Shorter D, Kosten TR. Update on pharmacotherapy for treatment of opioid use disorder. Expert Opin Pharmacother 2016;17:2307-18. [Crossref] [PubMed]
- Pergolizzi JV Jr, Annabi H, Gharibo C, et al. The Role of Lofexidine in Management of Opioid Withdrawal. Pain Ther 2019;8:67-78. [Crossref] [PubMed]
- Akhurst JS. Lofexidine in opiate withdrawal: a safety and usage survey. Pharmacoepidemiol Drug Saf 2000;9:43-7. [Crossref] [PubMed]
- Lofexidine (Lucemyra) for opioid withdrawal. Med Lett Drugs Ther 2018;60:115-7. [PubMed]
- Jasinski DR, Johnson RE, Kocher TR. Clonidine in morphine withdrawal. Differential effects on signs and symptoms. Arch Gen Psychiatry 1985;42:1063-6. [Crossref] [PubMed]
- Sigmon SC, Bisaga A, Nunes EV, et al. Opioid detoxification and naltrexone induction strategies: recommendations for clinical practice. Am J Drug Alcohol Abuse 2012;38:187-99. [Crossref] [PubMed]
- Kristensen Ø, Lolandsmo T, Isaksen A, et al. Treatment of polydrug-using opiate dependents during withdrawal: towards a standardisation of treatment. BMC Psychiatry 2006;6:54. [Crossref] [PubMed]
- Klein LR, Cole JB, Driver BE, et al. An open-label randomized trial of intramuscular olanzapine versus oral clonidine for symptomatic treatment of opioid withdrawal in the emergency department. Clin Toxicol (Phila) 2019;57:697-702. [Crossref] [PubMed]
- Zarghami M, Sheikhmoonesi F, Ala S, et al. A comparative study of beneficial effects of Olanzapine and sodium valproate on aggressive behavior of patients who are on methadone maintenance therapy: a randomized triple blind clinical trial. Eur Rev Med Pharmacol Sci 2013;17:1073-81. [PubMed]
- Stein MD, Kurth ME, Sharkey KM, et al. Trazodone for sleep disturbance during methadone maintenance: a double-blind, placebo-controlled trial. Drug Alcohol Depend 2012;120:65-73. [Crossref] [PubMed]
- Pinkofsky HB, Hahn AM, Campbell FA, et al. Reduction of opioid-withdrawal symptoms with quetiapine. J Clin Psychiatry 2005;66:1285-8. [Crossref] [PubMed]
- Vento AE, Kotzalidis GD, Cacciotti M, et al. Quetiapine Abuse Fourteen Years Later: Where Are We Now? A Systematic Review. Subst Use Misuse 2020;55:304-13. [Crossref] [PubMed]
- Evoy KE, Teng C, Encarnacion VG, et al. Comparison of Quetiapine Abuse and Misuse Reports to the FDA Adverse Event Reporting System With Other Second-Generation Antipsychotics. Subst Abuse 2019;13:1178221819844205. [Crossref] [PubMed]
- Buttram ME, Kurtz SP, Ellis MS, et al. Gabapentin prescribed during substance abuse treatment: The perspective of treatment providers. J Subst Abuse Treat 2019;105:1-4. [Crossref] [PubMed]
- Blackmer J, Lindahl E, Strahl A, et al. Regulating gabapentin as a drug of abuse: A survey study of Kentucky community pharmacists. J Am Pharm Assoc 2003;2019:379-82. [PubMed]
- Tharp AM, Hobron K, Wright T. Gabapentin-related Deaths: Patterns of Abuse and Postmortem Levels. J Forensic Sci 2019;64:1105-11. [Crossref] [PubMed]
- Chiappini S, Schifano F. Is There a Potential of Misuse for Quetiapine? Literature Review and Analysis of the European Medicines Agency/European Medicines Agency Adverse Drug Reactions' Database. J Clin Psychopharmacol 2018;38:72-9. [Crossref] [PubMed]
- Scherrer JF, David Schneider F, Lustman PJ. Opioid analgesics and chronic non-cancer pain: a prescription for research in primary care. Fam Pract 2016;33:569-71. [Crossref] [PubMed]
- Stein MD, Kurth ME, Anderson BJ, et al. A Pilot Crossover Trial of Sleep Medications for Sleep-disturbed Methadone Maintenance Patients. J Addict Med 2019. [Epub ahead of print]. [Crossref] [PubMed]
- Voelker R. States Move to Substitute Opioids With Medical Marijuana to Quell Epidemic. JAMA 2018;320:2408-10. [Crossref] [PubMed]
- Walley AY, Bernson D, Larochelle MR, et al. The Contribution of Prescribed and Illicit Opioids to Fatal Overdoses in Massachusetts, 2013-2015. Public Health Rep 2019;134:667-74. [Crossref] [PubMed]
- Raffa RB, Pergolizzi JV Jr, LeQuang JA, et al. The fentanyl family: A distinguished medical history tainted by abuse. J Clin Pharm Ther 2018;43:154-8. [Crossref] [PubMed]
- Sohler NL, Starrels JL, Khalid L, et al. Cannabis Use is Associated with Lower Odds of Prescription Opioid Analgesic Use Among HIV-Infected Individuals with Chronic Pain. Subst Use Misuse 2018;53:1602-7. [Crossref] [PubMed]
- Vigil JM, Stith SS, Adams IM, et al. Associations between medical cannabis and prescription opioid use in chronic pain patients: A preliminary cohort study. PLoS One 2017;12:e0187795. [Crossref] [PubMed]
- Boehnke KF, Litinas E, Clauw DJ. Medical Cannabis Use Is Associated With Decreased Opiate Medication Use in a Retrospective Cross-Sectional Survey of Patients With Chronic Pain. J Pain 2016;17:739-44. [Crossref] [PubMed]
- Piper BJ, DeKeuster RM, Beals ML, et al. Substitution of medical cannabis for pharmaceutical agents for pain, anxiety, and sleep. J Psychopharmacol 2017;31:569-75. [Crossref] [PubMed]
- Bradford AC, Bradford WD, Abraham A, et al. Association Between US State Medical Cannabis Laws and Opioid Prescribing in the Medicare Part D Population. JAMA Intern Med 2018;178:667-72. [Crossref] [PubMed]
- Bachhuber MA, Arnsten JH, Cunningham CO, et al. Does Medical Cannabis Use Increase or Decrease the Use of Opioid Analgesics and Other Prescription Drugs? J Addict Med 2018;12:259-61. [Crossref] [PubMed]
- Wen H, Hockenberry JM. Association of Medical and Adult-Use Marijuana Laws With Opioid Prescribing for Medicaid Enrollees. JAMA Intern Med 2018;178:673-9. [Crossref] [PubMed]
- de Carvalho CR, Takahashi RN. Cannabidiol disrupts the reconsolidation of contextual drug-associated memories in Wistar rats. Addict Biol 2017;22:742-51. [Crossref] [PubMed]
- Izzo AA, Borrelli F, Capasso R, et al. Non-psychotropic plant cannabinoids: new therapeutic opportunities from an ancient herb. Trends Pharmacol Sci 2009;30:515-27. [Crossref] [PubMed]
- Campos AC, Guimaraes FS. Evidence for a potential role for TRPV1 receptors in the dorsolateral periaqueductal gray in the attenuation of the anxiolytic effects of cannabinoids. Prog Neuropsychopharmacol Biol Psychiatry 2009;33:1517-21. [Crossref] [PubMed]
- Seeman P. Cannabidiol is a partial agonist at dopamine D2High receptors, predicting its antipsychotic clinical dose. Transl Psychiatry 2016;6:e920. [Crossref] [PubMed]
- Lofwall MR, Babalonis S, Nuzzo PA, et al. Opioid withdrawal suppression efficacy of oral dronabinol in opioid dependent humans. Drug Alcohol Depend 2016;164:143-50. [Crossref] [PubMed]
- Lucas P. Cannabis as an adjunct to or substitute for opiates in the treatment of chronic pain. J Psychoactive Drugs 2012;44:125-33. [Crossref] [PubMed]
- Bleyer A, Barnes B. Opioid death rate acceleration in jurisdictions legalizing marijuana use. JAMA Intern Med 2018;178:1280-1. [Crossref] [PubMed]
- Lynskey MT, Vink JM, Boomsma DI. Early onset cannabis use and progression to other drug use in a sample of Dutch twins. Behav Genet 2006;36:195-200. [Crossref] [PubMed]
- Epstein DH, Preston KL. No evidence for reduction of opioid-withdrawal symptoms by cannabis smoking during a methadone dose taper. Am J Addict 2015;24:323-8. [Crossref] [PubMed]
- Nava F, Manzato E, Lucchini A. Chronic cannabis use does not affect the normalization of hypothalamic-pituitary-adrenal (HPA) axis induced by methadone in heroin addicts. Prog Neuropsychopharmacol Biol Psychiatry 2007;31:1089-94. [Crossref] [PubMed]
- Shmagel A, Krebs E, Ensrud K, et al. Illicit Substance Use in US Adults With Chronic Low Back Pain. Spine (Phila Pa 1976) 2016;41:1372-7. [Crossref] [PubMed]
- Maher DP, Carr DB, Hill K, et al. Cannabis for the Treatment of Chronic Pain in the Era of an Opioid Epidemic: A Symposium-Based Review of Sociomedical Science. Pain Med 2019;20:2311-23. [Crossref] [PubMed]
- Choo EK, Feldstein Ewing SW, Lovejoy TI. Opioids Out, Cannabis In: Negotiating the Unknowns in Patient Care for Chronic Pain. JAMA 2016;316:1763-4. [Crossref] [PubMed]
- Wasserman DA, Weinstein MG, Havassy BE, et al. Factors associated with lapses to heroin use during methadone maintenance. Drug Alcohol Depend 1998;52:183-92. [Crossref] [PubMed]
- Andreae MH, Rhodes E, Bourgoise T, et al. An Ethical Exploration of Barriers to Research on Controlled Drugs. Am J Bioeth 2016;16:36-47. [Crossref] [PubMed]
- Epstein DH, Preston KL. Does cannabis use predict poor outcome for heroin-dependent patients on maintenance treatment? Past findings and more evidence against. Addiction 2003;98:269-79. [Crossref] [PubMed]
- Church SH, Rothenberg JL, Sullivan MA, et al. Concurrent substance use and outcome in combined behavioral and naltrexone therapy for opiate dependence. Am J Drug Alcohol Abuse 2001;27:441-52. [Crossref] [PubMed]
- Raby WN, Carpenter KM, Rothenberg J, et al. Intermittent marijuana use is associated with improved retention in naltrexone treatment for opiate-dependence. Am J Addict 2009;18:301-8. [Crossref] [PubMed]
- Bidwell LC, Mueller R. A Novel Observational Method for Assessing Acute Responses to Cannabis: Preliminary Validation Using Legal Market Strains. Cannabis Cannabinoid Res 2018;3:35-44. [Crossref] [PubMed]
- Casarett DJ, Beliveau JN, Arbus MS. Benefit of Tetrahydrocannabinol versus Cannabidiol for Common Palliative Care Symptoms. J Palliat Med 2019;22:1180-4. [Crossref] [PubMed]
- Walsh Z, Gonzalez R, Crosby K, et al. Medical cannabis and mental health: A guided systematic review. Clin Psychol Rev 2017;51:15-29. [Crossref] [PubMed]
- Ren Y, Whittard J, Higuera-Matas A, et al. Cannabidiol, a nonpsychotropic component of cannabis, inhibits cue-induced heroin seeking and normalizes discrete mesolimbic neuronal disturbances. J Neurosci 2009;29:14764-9. [Crossref] [PubMed]
- Iffland K, Grotenhermen F. An update on safety and side effects of cannabidiol: a review of clinical data and relevant animal studies. Cannabis Cannabinoid Res 2017;2:139-54. [Crossref] [PubMed]
- Thomas A, Baillie GL, Phillips AM, et al. Cannabidiol displays unexpectedly high potency as an antagonist of CB1 and CB2 receptor agonists in vitro. Br J Pharmacol 2007;150:613-23. [Crossref] [PubMed]
- Nugent SM, Kansagara D. The Effects of Cannabis Among Adults With Chronic Pain. Ann Intern Med 2018;168:525. [Crossref] [PubMed]
- Mayet A, Legleye S, Falissard B, et al. Cannabis use stages as predictors of subsequent initiation with other illicit drugs among French adolescents: use of a multi-state model. Addict Behav 2012;37:160-6. [Crossref] [PubMed]
- Hall WD, Lynskey M. Is cannabis a gateway drug? Testing hypotheses about the relationship between cannabis use and the use of other illicit drugs. Drug Alcohol Rev 2005;24:39-48. [Crossref] [PubMed]
- Banister SD, Arnold JC, Connor M, et al. Dark Classics in Chemical Neuroscience: Delta(9)-Tetrahydrocannabinol. ACS Chem Neurosci 2019;10:2160-75. [Crossref] [PubMed]
- Rajagopal A, Vassilopoulou-Sellin R, Palmer JL, et al. Hypogonadism and sexual dysfunction in male cancer survivors receiving chronic opioid therapy. J Pain Symptom Manage 2003;26:1055-61. [Crossref] [PubMed]
- AminiLari M, Manjoo P, Craigie S, et al. Hormone replacement therapy and opioid tapering for opioid-induced hypogonadism among patients with chronic noncancer pain: a systematic review. Pain Med 2019;20:301-13. [Crossref] [PubMed]
- Uebelacker LA, Van Noppen D, Tremont G, et al. A pilot study assessing acceptability and feasibility of hatha yoga for chronic pain in people receiving opioid agonist therapy for opioid use disorder. J Subst Abuse Treat 2019;105:19-27. [Crossref] [PubMed]
- Deng G, Mao JJ. Acupuncture to Reduce Opioid Consumption in Patients with Pain: Getting to the Right Points. Pain Med 2019;20:207-8. [Crossref] [PubMed]
- Lovejoy TI, Morasco BJ, Demidenko MI, et al. Clinician referrals for non-opioid pain care following discontinuation of long-term opioid therapy differ based on reasons for discontinuation. J Gen Intern Med 2018;33:24-30. [Crossref] [PubMed]
- Amato L, Minozzi S, Davoli M, et al. Psychosocial and pharmacological treatments versus pharmacological treatments for opioid detoxification. Cochrane Database Syst Rev 2011.CD005031. [PubMed]
- Windmill J, Fisher E, Eccleston C, et al. Interventions for the reduction of prescribed opioid use in chronic non-cancer pain. Cochrane Database Syst Rev. 2013.CD010323. [PubMed]
- Eccleston C, Fisher E, Thomas KH, et al. Interventions for the reduction of prescribed opioid use in chronic non-cancer pain. Cochrane Database Syst Rev 2017;11:CD010323. [PubMed]
- Lamb SE, Hansen Z, Lall R, et al. Group cognitive behavioural treatment for low-back pain in primary care: a randomised controlled trial and cost-effectiveness analysis. Lancet 2010;375:916-23. [Crossref] [PubMed]
- Naylor MR, Naud S, Keefe FJ, et al. Therapeutic Interactive Voice Response (TIVR) to reduce analgesic medication use for chronic pain management. J Pain 2010;11:1410-9. [Crossref] [PubMed]
- Carmichael AN, Morgan L, Del Fabbro E. Identifying and assessing the risk of opioid abuse in patients with cancer: an integrative review. Subst Abuse Rehabil 2016;7:71-9. [PubMed]
- Rauenzahn S, Sima A, Cassel B, et al. Urine drug screen findings among ambulatory oncology patients in a supportive care clinic. Support Care Cancer 2017;25:1859-64. [Crossref] [PubMed]
- Cornish R, Macleod J, Strang J, et al. Risk of death during and after opiate substitution treatment in primary care: prospective observational study in UK General Practice Research Database. BMJ 2010;341:c5475. [Crossref] [PubMed]
- Fitzgibbon DR, Rathmell JP, Michna E, et al. Malpractice claims associated with medication management for chronic pain. Anesthesiology 2010;112:948-56. [Crossref] [PubMed]
- Shields LBE, Johnson TA, Murphy JP, et al. Decline in primary care providers' prescribing of Schedule II opioids following the implementation of federal and state guidelines. J Opioid Manag 2019;15:111-8. [Crossref] [PubMed]
- Austin RC, Fusco CW, Fagan EB, et al. Teaching Opioid Tapering Through Guided Instruction. Fam Med 2019;51:434-7. [Crossref] [PubMed]


