
Use of in-bed cycling combined with passive joint activity in acute respiratory failure patients receiving mechanical ventilation
Introduction
Acute respiratory failure (ARF) is one of the most common respiratory diseases in Intensive Care Unit (ICU). Studies have shown that ARF accounts for 32% to 56% of all patients in ICU. In addition, another 35% of patients diagnosed with non-ARF will develop ARF during ICU hospitalization (1,2). ARF can cause labored breathing, carbon dioxide retention and others. Most patients with ARF require mechanical ventilation (MV), but long-term sedation and restraint for patients due to MV may cause many concurrent symptoms, such as ICU acquired weakness (ICU-AW). ICU-AW has been the most common complication in patients receiving MV and can be found in more than 25% of patients receiving MV for more than 7 days. ICU-AW together with delirium, pressure sores, prolonged hospital stay in ICU (3-5) significantly affect the functional recovery and quality of life of patients after discharge. Although these complications are caused by a variety of factors, MV after long-term immobilization is one of the most important reasons (6).
Clinical studies have confirmed that active early activity is a very safe and effective strategy to prevent against complications of MV and is also helpful for physical recovery (7-9). A variety of studies have shown the benefits of early MV. In-bed cycling is an early form of activity used by patients receiving MV in bed. In this activity, the patient’s lower limbs control the speed of the bicycle in ICU (10). In-bed cycling can improve the lower limb muscle strength and reduce the time of MV (11). Some multi-center randomized controlled trials (RCTs) have indicated early in-bed cycling for MV patients in ICU is feasible (12), even in patients with sedation, critical illness, MV and vasoactive treatment (13). However, it also has certain limitations, because this activity can exercise the lower limbs only and thus it cannot be popularized to a certain extent. In this study, we investigated the safety and feasibility of in-bed cycling combined with passive joint activity in ARF patients receiving MV.
Methods
Patients
Patients who underwent MV were recruited from HwaMei Hospital, University of Chinese Academy of Sciences between Jan 2018 and Oct 2018. Inclusion criteria were as follows: (I) the Glasgow Coma Scale (GCS) score was 15 before admission, and patients could communicate via gesture or expression before admission; (II) ARF was the main cause of ICU, and the Barthel index score was above 61 points before admission; (III) MV was administered within 48 h; (IV) MV was administered after admission into ICU; (V) patients were older than 18 years; (VI) patients had the acute physiology and chronic health score (APACHE II score) ≥10 and were voluntary to participate in this study, and informed consent was obtained before study.
Exclusion criteria were as follows: (I) patients were pregnant women; (II) patients had diseases (such as fractures, muscle weakness, suspected nervous system damage) that may cause long-term muscle weakness; (III) patients had the risk for severe bleeding, the platelet count was <50×109/L, and the activated partial thromboplastin time (APTT) was >50 s; (IV) patients had a history of myocardial ischemia, malignant arrhythmia, blood purification treatment and ECMO assist.
Grouping
A total of 112 patients were enrolled into the present study and randomly assigned into control group and intervention group by using a random number table. There were 55 patients in the intervention group and 57 patients in the control group. Among them, 5 patients were excluded due to being transferred to another hospital due to the change in disease condition or discharge from the hospital, and 107 patients were included for final analysis. At the time of admission, all patients received orotracheal intubation. There were 53 patients in the intervention group and 54 patients in the control group. There were no significant differences in the age, gender, disease type, and APACHE II scores between the two groups (P>0.05; Table 1).

Full table
Study design
Patients in the control group received routine treatments in ICU, including turning over every 2 h and releasing both upper limbs for 5 min. Lower extremities were treated with lower extremity pneumatic pump for 20–30 min twice daily, and ventilator clustering care strategy was employed to prevent ventilator-associated pneumonia: raising the bed, shallow sedation, preventing aspiration, and daily assessment of catheter indwelling.
In the intervention group, patients received an in-bed combination with the upper limb passive joint activity strategy and other treatments were the same to those in the control group.
The ICU critical rehabilitation team was responsible for the quality control in the early rehabilitation activities for mechanically ventilated patients. The team consisted of a lead nurse, an ICU clinician and four ICU nurses, and a rehabilitation doctor was hired as a technical guide. The team members had an experience in ICU for more than 6 years, with strong sense of responsibility. The team was headed by the deputy head nurse of ICU and responsible for coordinating the team. The rehabilitation doctor was responsible for informing the basic knowledge of rehabilitation in the team members, the use of bicycles, the training of passive joint activities of the upper limbs, and related examinations. The four ICU nurses performed rehabilitation training under the guidance of a rehabilitation doctor after passing the examination.
Patient evaluation before use of bicycles
Before use of bicycles, the evaluation team made an early evaluation on the bedside bicycle combined with the upper limb passive joint activity on the basis of the “Traffic Light Evaluation System” in the Expert Consensus (14). On the second day, some medical parameters were evaluated by a doctor in the morning, including: FiO2 <0.5; PEEP <10 cmH2O; f <30 beats/min; SPO2 >90%; PO2/FiO2 >300, no serious acid-base disorders; heart rate: 60–120 beats/min; 65 mmHg < mean arterial pressure <100 mmHg, or maintenance of blood pressure with vasoactive drug at a low dose (<5 µg/kg/min); no history of lower extremity arteriovenous thrombosis and pulmonary embolism; no delirium, normal intracranial pressure; no renal replacement therapy (CRRT). If the patient did not meet one of these criteria, the intervention was suspended and she/he was assessed on the next day.
Activity steps
In-bed cycling combined with upper limb passive joint activity strategy: the bed type used in the activity was German MOTOmed letto2. The in-bed cycling can be set to active mode and passive mode. At the active mode, the activity is controlled by the patient; at the passive mode, the speed should be set. The specific measures were as follows: the patient receiving the early rehabilitation activities was evaluated once daily by the competent doctor. The patient’s mind was evaluated again before the activity. If the patient was calm or clear-minded, the nurse communicated with the patients via speech or body language; if the gesture did not match the patient after communication, the passive mode was used, and the rotation speed in the first day was set at 10 times/min. If the changes in the heart rate and blood pressure during exercise were lower than 20% of the baseline levels, the speed was increased 3–5 times/min on the next day, but it was no longer increased after 20 times/min; if the patient had consciousness, no sedation or no analgesia, the active mode could be used by the members through language, body language or gesture communication. In the active mode, the patient could step on the bicycle in the bed to perform activities. If the speed was higher than 20 times/minute in the active mode, the changes in the heart rate and blood pressure were lower than 20% of the baseline levels and the patient was tolerable, the time of activity was extended appropriately on the next day; if the speed was lower than 8 times/minute in the active mode, and the patient was intolerable to this activity after communication with the patient, the passive mode was used.
When the patient exercised the lower limbs in the bed, the rehabilitation team members performed selective passive ROM exercise on the upper limbs: including elbow flexion-extension 0–90° and wrist palmar flexion—back stretch 0–80°, forearm pronation—0–80° after rotation. Activities were performed 10–15 times at daytime, twice daily. During the passive activities of the upper limb joints, the rehabilitation team members also observed the activity of the bicycles in the lower limbs and the vital signs. The duration of each activity was maintained at 15–30 min.
Activity suspension criteria
When the following conditions occurred during the rehabilitation exercise, the exercise stopped: f >40 beats/min, SPO2 <85%, ventilator man-machine confrontation longer than 10 seconds, breathing distress, sweating, cyanosis, heart rate >140 beats/min, <50 beats/min, or more than 30% or <30% of the baseline level, blood pressure higher or lower than 20% of the pre-recovery blood pressure, discomfort as shown by body language or gestures, new arrhythmia, or change in consciousness.
Medical ethics
This study was approved by the Ethics Committee of our hospital (No. pj-nbey-ky-2018-014-01).
Observations
The time of MV, ICU stay, and Barthel index score before being transferred was recorded. Incidence of ICU acquired debilitation in two groups was observed: ICU-AW was assessed on the limb muscle strength of the patient with a scale developed by the British Medical Research Council (MRC) (15). Three groups of muscles were selected for each limb (bilateral upper limbs: raising the arm, flexing the forearm, straightening the wrist; bilateral lower limbs: flexing the leg, straightening the knee joint, flexing the foot to the dorsal side) for evaluation. The muscle strength was divided into 6 grades: 0 to 5, and grade 5 muscle strength represents normal muscle strength. The muscle strength of 6 pairs of muscle groups was added, the score ranged from 0 to 60: 0 represents quadriplegia and 60 is indicative of normal muscle strength; The MRC lower than 48 was used for the diagnosis of ICU-AW. The muscle strength assessment was performed on the day of being transferred out of ICU. Adverse events were also recorded.
Statistical analysis
Data were analyzed with SPSS version 20.0. The categorical data were compared using χ2 test; the quantitative data are expressed as mean ± standard deviation and compared with t-test. A value of P<0.05 was considered statistically significant.
Results
Adverse events in two groups
In the early period of activity, only one patient in the intervention group experienced a decrease in the SPO2 from 97% to 87% with tachypnea. The SPO2 and respiration returned normal after activity discontinuation and 2-min oxygen inhalation. No serious adverse events (such as accidental extubation and patient injury) occurred in both groups during the intervention.
Related indicators in two groups
As shown in Table 2, the average time of MV in the intervention group was significantly shorter than in the control group, and the ICU stay was also markedly shorter than in the control group. Moreover, the major Barthel index in the intervention group was significantly higher than in the control group, suggesting that the self-care ability of patients in the intervention group is improved.

Full table
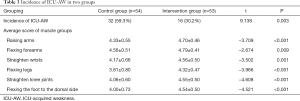
Incidence of ICU-AW in two groups
As shown in Table 3, the incidence of ICU-AW in the intervention group was 30.2%, and 59.3% in the control group, showing significant difference. It is indicated that the incidence of ICU-AW in patients receiving MV was reduced by using the bed bicycle combined with passive upper limb joint activities. Moreover, the muscle strength scores in the intervention group were significantly better than in the control group in the raising arms, flexing forearms, straightening wrists, flexing bilateral lower limbs, straightening knees and flexing feet to the dorsal side.
Full table
Discussion
The lower in-bed cycling combined with the upper limb passive joint activity is safe and feasible for MV patients
It has been reported that early rehabilitation of mechanically ventilated patients is a very effective strategy for preventing against ventilator-related complications and promoting physical rehabilitation (16). However, the early rehabilitation of these patients is still limited by many factors in clinical practice, and the safety and the feasibility of early activities have been a major concern. In ICU, the environment is special, there is no escort, the disease condition is also particular, and there are many catheters and monitoring equipment on the patient’s body. Therefore, several medical personnel are needed for the early rehabilitation activities such as bedside sitting, standing, and even walking for mechanically ventilated patients. It is also necessary to take into account the tolerance of intubated patients. Currently, the rehabilitation activity is hard to perform due to the shortage of nursing staff in China, which significantly limits the development and promotion of this procedure. In addition, there are many medical disputes, the doctor-patient relationship is delicate, and nurses are usually stressed. Safety of patients is still a major concern in clinical practice (17). The early rehabilitation activities implemented in this study ranged from passive to active, from weak to strong, and from short to long, following the principle of step-by-step rehabilitation. First of all, the patient received a double lower limb bicycle exercise and passive upper joint activities without changing the lying position, which saves the human resources in assisting the activities and ensures the early rehabilitation safety. Secondly, the selective double upper limb passive joint activity exercise was employed. The motion of shoulder joint is restrained for the bedridden patients, the passive movement of the shoulder joint can not be done when the patient is in a supine position, thereby ensuring the safety. Third, in the rehabilitation activities, if the patient is in a calm state, the rehabilitation nurse can communicate with the patients via body language or gestures, which will increase the cooperation and safety of patients. During the intervention in this study, only one patient in the intervention group received early activity. The SPO2 decreased and the respiratory rate increased. The patient returned normal after the activity discontinuation. These results demonstrate the feasibility and safety of this intervention.
The lower in-bed cycling combined with the upper limb passive joint activity can reduce the time of MV
After MV and respiratory support for patients with ARF, sedation or physical constraintion, a “sleep” state is often employed to reduce oxygen consumption. However, the maintenance of muscle function depends on the exercise and normal contraction. When the muscle is immobilized or has no load after prolonged bed-rest, there will be atrophy and contraction dysfunction of the skeletal muscle and diaphragm muscle, which may cause the respiratory muscle weakness and ventilation dependence, thereby prolonging the time of MV time and forming a vicious circle. Healthy people who remain immobilized will lose 1.3 to 3 percent of their muscle strength each day. Absolute bed-rest will cause a 10% reduction in the muscle strength (18). Therefore, early rehabilitation is essential for mechanically ventilated patients who can not move. In this study, both lower limbs, the diaphragm, the intercostal muscles and the abdominal muscles are also excised with the current excise strategy, which may be beneficial for the patient’s breath. In addition, the cough and sputum increased during rehabilitation activities in the intervention group, which in turn reduced the incidence of atelectasis and lung infection, and ultimately improved the respiratory muscles and respiratory synergy. This prevents alveolar collapse, increases pulmonary ventilation, and ultimately shortens the time of MV, which is consistent with previous findings (19).
The lower in-bed cycling combined with the upper limb passive joint activity can reduce the incidence of ICU-AW and improve self-care ability
Long-term MV in bedridden patients can also limit the range of joint motion, cause the fibrosis of joint capsules and ligaments, and decrease synovial fluid in the joint cavity, which in turn leads to fixed contracture of the joint (20). Furthermore, the synthesis of muscle protein decreases, causing limb edema, neuromuscular dysfunction, and ultimate a decline in the self-care ability and the occurrence of ICU-AW. In this study, ICU rehabilitation nurses assisted the movements of the elbow joint, wrist joint, forearm and other parts of the upper limbs, and thus the biceps, triceps, and forearm pronator muscle were exclised. These muscles can actively contract and relax, and prevent muscular atrophy and joint stiffness. Through the joint activity training of the upper limbs, the muscle strength scores in the intervention group after extubation were significantly improved as compared to those in the control group. Moreover, during the movements of the lower limbs in the bed, the quadriceps, quadrigular muscles, soleus muscle and gastrocnemius muscles were also passively or actively excised to prevent lower limb muscle strength decline and foot drop phenomenon. Our results showed the incidence of ICU-AW in the intervention group was significantly lower than in the control group, and the Barthel index as well as the MRC muscle strength scores was significantly higher than in the control group (P<0.001). In the early rehabilitation activities, patients receiving MV for respiratory failure gradually completed the transitional exercise before the extubation, and their self-care ability was also improved after being transferred out of ICU, which is helpful for the following recovery.
Conclusions
In summary, the in-bed cycling combined with passive limb joint activities can effectively shorten the time of MV and ICU stay, restore the muscle strength, reduce the occurrence of ICU-AW and improve the quality of life in MV patients with ARF. However, there are several limitations in this study: only relevant parameters during the hospitalization were investigated; the patients were not followed up after discharge, so the following recovery of limb mobility or related complications were still unclear. More RCTs with elegant design are needed to confirm our findings.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the Ethics Committee of our hospital (No. pj-nbey-ky-2018-014-01), and informed consent was obtained before study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hruska P. Early Mobilization of Mechanically Ventilated Patients. Crit Care Nurs Clin North Am 2016;28:413-24. [Crossref] [PubMed]
- Netto AB, Taly AB, Kulkarni GB, et al. Complications in mechanically ventilated patients of Guillain-Barre syndrome and their prognostic value. J Neurosci Rural Pract 2017;8:68-73. [Crossref] [PubMed]
- Fan E, Zanni JM, Dennison CR, et al. Critical illness neuromyopathy and muscle weakness in patients in the intensive care unit. AACN Adv Crit Care 2009;20:243-53. [PubMed]
- Hermans G, Van Mechelen H, Clerckx B, et al. Acute outcomes and 1-year mortality of intensive care unit-acquired weakness. A cohort study and propensity-matched analysis. Am J Respir Crit Care Med 2014;190:410-20. [Crossref] [PubMed]
- Puthucheary ZA, Rawal J, McPhail M, et al. Acute skeletal muscle wasting in critical illness. JAMA 2013;310:1591-600. [Crossref] [PubMed]
- de Jonghe B, Lacherade JC, Sharshar T, et al. Intensive care unit-acquired weakness: risk factors and prevention. Crit Care Med 2009;37:S309-15. [Crossref] [PubMed]
- Needham DM, Korupolu R, Zanni JM, et al. Early physical medicine and rehabilitation for patients with acute respiratory failure: a quality improvement project. Arch Phys Med Rehabil 2010;91:536-42. [Crossref] [PubMed]
- Sricharoenchai T, Parker AM, Zanni JM, et al. Safety of physical therapy interventions in critically ill patients: a single-center prospective evaluation of 1110 intensive care unit admissions. J Crit Care 2014;29:395-400. [Crossref] [PubMed]
- Wang N, Cai X, Liu Z. Progress in early activity in the ICU. J Nurs Training 2018;33:1082-6.
- Kho ME, Molloy AJ, Clarke FJ, et al. TryCYCLE: A Prospective Study of the Safety and Feasibility of Early In-Bed Cycling in Mechanically Ventilated Patients. PLoS One 2016;11:e0167561. [Crossref] [PubMed]
- Machado ADS, Pires-Neto RC, Carvalho MTX, et al. Effects that passive cycling exercise have on muscle strength, duration of mechanical ventilation, and length of hospital stay in critically ill patients: a randomized clinical trial. J Bras Pneumol 2017;43:134-9. [Crossref] [PubMed]
- Kho ME, Molloy AJ, Clarke FJ, et al. Multicentre pilot randomised clinical trial of early in-bed cycle ergometry with ventilated patients. BMJ Open Respir Res 2019;6:e000383. [Crossref] [PubMed]
- Camargo Pires-Neto R, Fogaca Kawaguchi YM, Sayuri Hirota A, et al. Very early passive cycling exercise in mechanically ventilated critically ill patients: physiological and safety aspects--a case series. PLoS One 2013;8:e74182. [Crossref] [PubMed]
- Hodgson CL, Stiller K, Needham DM, et al. Expert consensus and recommendations on safety criteria for active mobilization of mechanically ventilated critically ill adults. Crit Care 2014;18:658. [Crossref] [PubMed]
- Stevens RD, Marshall SA, Cornblath DR, et al. A framework for diagnosing and classifying intensive care unit-acquired weakness. Crit Care Med 2009;37:S299-308. [Crossref] [PubMed]
- Yu L, Chen C, Jiang J. Nursing research progress of mechanical ventilation patients' early mobility in ICU. Chinese Journal of Modern Nursing 2017;23:2692-6.
- Guo H, Qi X, Li Y, et al. A literature review on working environment of nurses in China. Modern Clinical Nursing 2018;17:75-9.
- Fan E. Critical illness neuromyopathy and the role of physical therapy and rehabilitation in critically ill patients. Respir Care 2012;57:933-44; discussion 944-6. [Crossref] [PubMed]
- Dou Y, Pan C, Guo L, et al. Effectiveness of early in-bed cycling exercise on recovery of mechanically ventilated ICU patients. Journal of Nursing Science 2018;33:20-3.
- Clavet H, Hebert PC, Fergusson D, et al. Joint contracture following prolonged stay in the intensive care unit. CMAJ 2008;178:691-7. [Crossref] [PubMed]


