
Serum iron levels are negatively correlated with serum triglycerides levels in female university students
IntroductionOther Section
Dyslipidemia is defined as the derangement of 1 or more of the lipoproteins in blood, which includes elevated triglyceride (TG), total cholesterol (TC), and/or low-density lipoprotein cholesterol (LDL-C), or low levels of high-density lipoprotein cholesterol (HDL-C) alone (1). Epidemiology survey found that dyslipidemia is a major risk factor for atherosclerotic cardiovascular disease (CVD), cerebrovascular accident, and peripheral arterial disease (2). Additionally, evidence suggesting that elevated TG-rich lipoproteins represent causal risk factors for low-grade inflammation and all-cause mortality is growing (3). One epidemiology study showed that the prevalence of dyslipidemia was about 43% in China (4). Thus, prevention of dyslipidemia is urgently required for the primary prevention of CVD.
The available evidence indicates that the prevalence of dyslipidemia in students from primary and middle schools is 18.6% (5). Meanwhile, various international studies suggest prevalence of dyslipidemia in university students to be 33.9% for Nepalese students (6), 86.7% for Yemeni students (7), and 25.7% for Chilean students (8). However, there is little research on the prevalence of dyslipidemia among university students in China, and thus its status should be promptly clarified.
Epidemiology research has also found that disruptions in iron homeostasis are linked to a broad spectrum of chronic disease including cardiovascular, malignant, metabolic, and neurodegenerative diseases (9). Therefore, we hypothesized that serum iron might be associated with serum lipids, and few studies examining this relationship have been conducted.
Collectively, this study aimed to explore the relationship between serum iron level and blood lipids. We found that serum iron level was negatively correlated with TG, but was positively correlated HDL-cholesterol, LDL-cholesterol, and TC in female students. The current study suggests that iron supplementation can be a strategy to prevent high serum TG in female students.
MethodsOther Section
Subjects
This cross-sectional study recruited a total of 3,900 university students who participated in a physical examination. Then, we randomly selected a sample of 290 students aged 16–23 years old for this study.
Anthropometric measurements
Height and weight were measured using a method described in our pervious study (10). Briefly, standard stadiometer was used to measure height, while electronic scales were used for measuring weight. Body mass index (BMI) was calculated as weight (kilograms)/height (metres2).
Measurement of blood lipids
First, 10 ml of venous blood was collected. Then, TG, TC, HDL-C, and LDL-C were measured by automatic biochemical analyzer at the school hospital of Wannan Medical College. Dyslipidemia was defined as follows: TC ≥6.22 mmol/L was defined as high TC, LDL-C ≥4.14 mmol/L was defined as high LDL-C, HDL-C <1.04 mmol/L was defined as low HDL-C, and TG ≥2.26 mmol/L was defined as high TG. Serum iron level was measured with the ADVIA 2400 (Siemens Healthcare Diagnostics, Illinois, USA) using colorimetric methods.
Statistical analysis
All data were analyzed using SPSS version 18(Chicago, IL, USA). Descriptive statistics were used for the characteristics (height, weight, BMI, total serum iron level, TC weight, HDL-cholesterol, LDL-cholesterol, TG, and age) of the students included. Mean level of TC, HDL-cholesterol, LDL-cholesterol, TG, and age were compared between male subjects and female subjects. Pearson’s correlation coefficient was used to determine an association between serum iron level and blood lipids, with a value of P<0.05 being considered statistically significant.
ResultsOther Section
General characteristics
A total of 290 students (160 males and 130 females) were recruited in our study. General characteristics of the students are shown in Table 1.
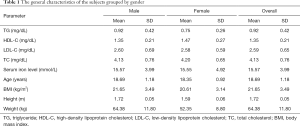
Full table
Prevalence of dyslipidemia among university students
The prevalence of dyslipidemia was 8.8% among male students and 5.4% among female students. The overall prevalence of dyslipidemia was 7.2% among the total students (Table 2).
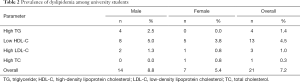
Full table
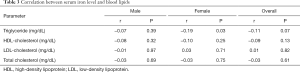
The relationship between serum iron level and blood lipids
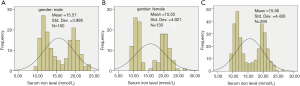
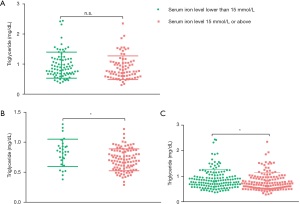
Table 3 showed that the serum iron level was negatively correlated with TG, but was positively correlated HDL-cholesterol, LDL-cholesterol, and TC in female students (P<0.05). No correlation was found between serum iron level and blood lipids in male students and overall students(P>0.05). Then, we determined whether serum iron level had a normal distribution in the study population. Our results showed that distribution of serum iron level displayed two-peak profiles in male students (Figure 1A), female students (Figure 1B), and overall students (Figure 1C). The mean level of serum iron was about 15 mmol/L. Next, we divided the study population into 2 groups according to the level of serum iron (the <15 mmol/L group and the ≥15 mmol/L group). No significant difference of serum TG level was found between male students with serum iron levels lower than 15 mmol/L and male students with serum iron levels 15 mmol/L or above (Figure 2A). Female students (Figure 2B) with serum iron levels lower than 15 mmol/L had a higher level of serum TG than female students with serum iron levels 15 mmol/L or above (P<0.05), which is the same as the results in the overall students (Figure 2C).
Full table
DiscussionOther Section
The principal finding of our study was that the prevalence of dyslipidemia was 8.8% among male students and 5.4% among female students. This result suggests that the prevalence of dyslipidemia among university students in our study is lower than that in other countries (11). The difference between our study and other studies may be accounted for by divergent socioeconomic status, behavioral habits, and lifestyles across different countries.
Another central result was that the serum iron level was negatively correlated with TG, but was positively correlated with HDL-cholesterol, LDL-cholesterol, and TC in female students. Elevated TG levels are a biomarker of cardiovascular risk (12). Therefore, it is interesting to find the correlation of serum iron levels with TG among female university students. So far, there has been no direct evidence found between serum iron levels and serum TG levels. One meta-analysis did find that daily iron supplementation effectively improves exercise performance and symptomatic fatigue (13). Cohort studies should be conducted to confirm the relationship between iron supplementation and serum TG among female university students, and even the general female population.
Some limitations of this study should be addressed. First, we only selected a small sample for inclusion, and so large-scale study is still needed to confirm the results. Furthermore, our findings were derived from general health examinations. Thus, we failed to acquire more detailed information like behavior, habits, and diet. These shortcomings notwithstanding, our study describes the general profile of blood lipids of students from a medical university. Of further note, we found that serum iron level was negatively correlated with TG, but was positively correlated with HDL-cholesterol, LDL-cholesterol, and TC in female students. These findings can offer a basis for interventions against dyslipidemia in university students.
ConclusionsOther Section
These findings suggest that the overall prevalence of dyslipidemia in the current sample population was relatively low compared to other countries. Furthermore, the total students lower serum iron level may indicate that high serum TG is a risk factor in female students. Iron supplementation could thus be a measure for preventing high serum TG in female students.
AcknowledgmentsOther Section
Funding: This study was supported by the Natural Science Foundation of the Jiangsu Higher Education Institutions of China (19KJB310007).
FootnoteOther Section
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the ethics committee at Wannan Medical College. Written informed consent was obtained from all subjects.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
ReferencesOther Section
- Joint committee for guideline revision. 2016 Chinese guidelines for the management of dyslipidemia in adults. J Geriatr Cardiol 2018;15:1-29.
- Wild SH, Byrne CD, Tzoulaki I, et al. Metabolic syndrome, haemostatic and inflammatory markers, cerebrovascular and peripheral arterial disease: The Edinburgh Artery Study. Atherosclerosis 2009;203:604-9. [Crossref] [PubMed]
- Nordestgaard BG. Triglyceride-Rich Lipoproteins and Atherosclerotic Cardiovascular Disease: New Insights From Epidemiology, Genetics, and Biology. Circ Res 2016;118:547-63. [Crossref] [PubMed]
- Opoku S, Gan Y, Fu W, et al. Prevalence and risk factors for dyslipidemia among adults in rural and urban China: findings from the China National Stroke Screening and prevention project (CNSSPP). BMC Public Health 2019;19:1500. [Crossref] [PubMed]
- Li Y, Luo J, Ma J, et al. Prevalence of dyslipidemia and its influential factors in 2 028 students from primary and middle schools in Changsha. Zhong Nan Da Xue Xue Bao Yi Xue Ban 2017;42:673-80. [PubMed]
- Nepal G, Tuladhar ET, Acharya K, et al. Dyslipidemia and Associated Cardiovascular Risk Factors among Young Nepalese University Students. Cureus 2018;10:e2089. [PubMed]
- Al-Duais MA, Al-Awthan YS. Prevalence of dyslipidemia among students of a Yemeni University. J Taibah Univ Med Sci 2019;14:163-71. [PubMed]
- Morales G, Guillen-Grima F, Munoz S, et al. Rev Med Chil 2017;145:299-308. [Cardiovascular risk factors among first and third year university students]. [Crossref] [PubMed]
- Basuli D, Stevens RG, Torti FM, et al. Epidemiological associations between iron and cardiovascular disease and diabetes. Front Pharmacol 2014;5:117. [PubMed]
- He L, Qian Y, Ren X, et al. Total serum calcium level may have adverse effects on serum cholesterol and triglycerides among female university faculty and staffs. Biol Trace Elem Res 2014;157:191-4. [Crossref] [PubMed]
- Gonzalez Sandoval CE, Diaz Burke Y, Mendizabal-Ruiz AP, et al. Nutr Hosp 2014;29:315-21. [Prevalence of obesity and altered lipid profile in university students]. [PubMed]
- Budoff M. Triglycerides and Triglyceride-Rich Lipoproteins in the Causal Pathway of Cardiovascular Disease. Am J Cardiol 2016;118:138-45. [Crossref] [PubMed]
- Joy JM, Lowery RP, Wilson JM, et al. The effects of 8 weeks of whey or rice protein supplementation on body composition and exercise performance. Nutr J 2013;12:86. [Crossref] [PubMed]



