
The effect of breathing exercises on patients with GERD: a meta-analysis
Introduction
Gastroesophageal reflux disease (GERD) is a frequently-occurring digestive system disorder, and its incidence has been increasing year by year (1). GERD is caused by disorder in the movement of the upper digestive tract and gastric acid reflux in the esophagus, which leads to various injuries and discomfort. There are two main reasons for gastric acid entering the esophagus: firstly, an increase in stomach abdominal cavity pressure cause by, for example, satiety, obesity, or gastric emptying disorder; and, secondly, a weakened anti-reflux mechanism (2). Normally, the gastroesophageal junction (GEJ) valve mechanism can be found between the esophagus and the stomach, consisting of the lower oesophageal sphincter (LES), the crural diaphragm (CD), the angle of His, and the phrenoesophageal membrane, which together form a barrier against gastroesophageal reflux (3).
Proton pump inhibitors (PPIs) are the first choice and classic drug for treating patients with GERD (4). However, symptoms may recur after withdrawal, and there is no significant benefit for patients with refractory GERD (5). Long-term use of PPI drugs holds potential risks for the respiratory, circulatory, and digestive systems (6), particularly in elderly people (7). Therefore, it is necessary to explore other safe and effective treatments.
Recent studies have shown that breathing exercises can enhance the crural diaphragm tension (CDT), strengthen the diaphragm barrier mechanism, reduce acid reflux and subsequent damage, and improve the efficacy of drug therapy (8). The purpose of this article is to explore the efficacy and effect of breathing exercises on GERD through a systematic review and meta-analysis of relevant literature, and to provide reference evidences of breathing exercises as a treatment for GERD patients.
Methods
Literature search
An online search was conducted to identify relevant randomized controlled trials (RCTs) and prospective studies published online on all major English language databases (PubMed, Embase, the Cochrane library, CENTRAL, Web of Science, AMED, and CINAHL).
Generally, the literature retrieval process was carried out as follows: (I) retrieval of relevant systematic reviews and meta-analysis from the Cochrane Library, (II) retrieval and reading of the relevant original literature from the domestic and foreign databases, and analysis and summary of the relevant literature subject words, keywords. The search terms used were:“Gastric Acid Reflux”, “Acid Reflux, Gastric”, “Reflux, Gastric Acid”, “Gastric Acid Reflux Disease”, “Gastro-Esophageal Reflux”, “Gastro Esophageal Reflux”, “Reflux Gastro-Esophageal”, “Gastroesophageal Reflux Disease”, “GERD”, “Reflux Gastroesophageal”, “Esophageal Reflux”, “Gastro-oesophageal Reflux”, “Gastro oesophageal Reflux”, “Reflux Gastro-oesophageal” and “Respiratory Muscle Training”, “Exercise Breathing”, “Muscle Training, Respiratory”, “Training, Respiratory Muscle”, (III) we took into account literature published from the time of database construction to October 1, 2019, and applied the inclusion and exclusion criteria set out below, (IV) we also searched the references and related research of the returned literature to identify any further studies relevant to our meta-analysis.
Inclusion and exclusion criteria
Inclusion criteria
The following inclusion criteria was applied to our literature search:
- Research type: a prospective or RCT of breathing exercises in patients with GERD that was officially published in English before October 1, 2019;
- Research design: the purpose and method of each study were the same or similar, and the RCT study was divided into a respiratory exercise treatment group and a control group. The intervention was to treat the patients with respiratory exercises, while the control group was treated only with conventional drugs or with sham breathing exercises. There was no limit to the frequency and cycle of breathing exercise interventions;
- Subjects: aged ≥18 years, meeting the diagnostic criteria of GERD (9): (i) the patients have symptoms such as typical heartburn, regurgitation and acid regurgitation, which can be combined with atypical symptoms such as chest pain, belching or extra-esophageal symptoms such as cough and asthma, should have been experienced for at least 6 months; (ii) the diagnosis was confirmed by endoscopy or a 24 h esophageal pH-value test; (iii) the patients treated by PPI or acid suppressant effectively, and symptoms recur after withdrawal.The patients with secondary GERD(other factors can cause or aggravate esophagitis, such as surgery, pregnancy, drugs, etc.) should be excluded. Patients have no serious chronic disease or organic disease such as, for example, hypertension, diabetes, upper gastrointestinal ulcer, or hiatus dysfunction;
- Primary outcomes: reflux symptoms, GERD-health-related quality of life, (GERD-HRQL), acid suppressant consumption, and esophageal pressure measurement;
- Research ethics: informed consent was obtained from all participants and the study was approved by the relevant ethics committee.
Exclusion criteria
Studies that met the following criteria were excluded from our met-analysis:
- Redundant or duplicate publication;
- The original document cannot be obtained through various methods;
- A small sample size (N<10);
- Incomplete or contradictory data;
- Inappropriate statistical methods;
- The experimental design and the intervention were vague or combined with other interventions;
- Review, letter, case report, or other non-primary literature.
Screening literature and extracting data
The retrieved studies were imported into EndNote X7 to remove duplication. Two researchers independently screened the literature according to the inclusion criteria and exclusion criteria, and a third researcher participated in the decision-making to settle differences when they occurred.
The text of the selected literature was read in full, and the following data were extracted: basic information (e.g., author and publication year), research objects (e.g., sample size, age, and gender), experimental design (e.g., grouping method, intervention measures, frequency, and intensity.), and outcome indicators.
Evaluating the quality of the literature
The Cochrane 5.1.0 systematic review manual (10) was used to evaluate the studies, including generation of random sequences, allocation concealment, blinding method (for researcher/patients), integrity of the data, selective reporting, and other biases. Each item in the literature was evaluated and classified into “low risk”, “high risk”, or “unclear”, according to the probability of bias. Guided by these standards, the studies were divided into A, B, and C levels, which meant “full compliance”, “partial compliance”, and “complete non-compliance”. C-level studies had high risk for performance bias, we excluded those.
The whole evaluation process was conducted independently by two researchers, with a third researcher to assist with decision-making when differences occurred in the evaluation results.
Statistical methods
The RevMan 5.3 statistical software provided by “www.cochrane.org” was used for the meta-analysis. The chi-square test was used to verify the heterogeneity among the studies, and sensitivity analysis was used to identify the source of heterogeneity as far as possible and eliminate it. A random effects model was used if there was heterogeneity (P≤0.1, I ≥50%). If heterogeneity did not exist (P>0.1, I2<50%), the fixed effects model was used for analysis. Subgroup analysis or descriptive analysis was used for results with significant heterogeneity or different study methods. We use the weighted mean difference (WMD) to analyze statistical data effectiveness for numerical or continuous data, and calculated the 95% confidence interval (95% CI). The difference was statistically significant when P<0.05.
Results
Literature search results
A total of 88 studies were returned via the database search, and 7 were manually identified by other means. After eliminating duplicates, 52 studies remained. The abstract and then the full texts of these studies were carefully read, and 29 and 16 studies were excluded at each stage, respectively. Seven eligible studies were included in our meta-analysis. The Flow chart of literatures screening is shown in Figure 1.
Features of the selected literature
The seven eligible studies were all prospective in nature (11-17) and explored the actual efficacy and possible mechanism of breathing exercises in patients with GERD. These studies were performed in China, Singapore, Australia, Italy, and Brazil, involving 194 GERD patients and 16 healthy volunteers. All of the studies had clear inclusion and exclusion criteria, and patients were diagnosed with GERD according to clear diagnostic criteria through endoscopic examination and symptom assessment. Mainstream diagnostic criteria were used in each region and country, and secondary patients were excluded prior to the research commencing. Generally, the breathing exercise methods in the seven studies were the same or similar, and and they all focused on strengthening diaphragm tension and improving GERD symptoms (11-17) All of the studies evaluated the effect of short-term intervention from four to eight weeks (11-17), and 3 of them evaluated the long-term effect of four to nine months (12,13,16). Four studies recorded the symptoms of gastroesophageal reflux in patients (11-14), four recorded the change in esophageal pressur (13-15,17), two measured esophageal pH-value (14-16), one showed the results of laryngeal endoscopy (11), and one recorded the usage of acid suppression (13).
Three of the RCTs were designed in parallel (13,15,16). Both the experimental and control groups received PPI or acid suppressant before starting the experiment to ensure the initial disease severity of the subjects was roughly similar, and refractory GERD patients were excluded. In the study of Sun et al., five patients were lost during long-term follow-up (13). The characteristics of the selected studies are shown in Table 1.
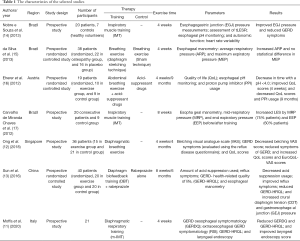
Full table
Methodological quality of the selected studies
The blinding method was described in detail in two studies, but not in the rest. According to the Cochrane 5.1.0 systematic review manual, six RCT studies were grade B and two were grade A. In these RCT studies, there was no statistically significant difference between the experimental and control groups in terms of age, gender, body weight, body mass index. The methodological quality of the selected studies is shown in Table 2.
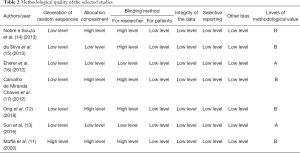
Full table
Meta-analysis results of breathing exercises on anti-reflux barrier in patients with GERD
Three RCTS reported the effects of breathing exercises on LES pressure in patients with GERD (13,15,16). There was no significant heterogeneity between the studies (P=0.62, I2=0%), and the fixed effects model was adopted. The results showed that breathing exercises had an effect on LES stress in GERD patients, with a statistically significant difference [WMD =1.36, 95% CI: (0.82, 1.91), P<0.01], as shown in Figure 2. The data used in the meta-analysis were calculated and converted from the original data.
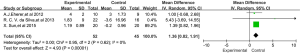
Sun et al. (13) showed that GERD symptoms improved in the experimental group after breathing exercises. Further investigation revealed that CDT and GEJ pressure in the experimental group were enhanced, which may be the mechanism of breathing exercises in the treatment of GERD.
Discussion
Methodological quality of the selected studies
All of the studies included in this meta-analysis performed prospective efficacy studies on breathing exercises as an auxiliary treatment method. We evaluated the literature focusing on seven areas: generation of random sequences, allocation concealment, integrity of the data, blinding method, selective reporting, and other bias. Out of the three RCTs included (13,15,16), da Silva et al. (15) did not describe the blinding method for the researcher, but the other two RCTs had complete records, and their methodological quality level was A (13,16).
The effects of breathing exercises on reflux symptoms in patients with GERD
The evaluation criteria of GERD symptoms and the quality of life use the universal and simple objective evaluation and self-scoring system in these literatures (18). Minor modifications were made to for each study according to the specific conditions for the smaller heterogeneity. According to the analysis results, the short-term effect of breathing exercises on reflux symptoms and quality of life in patients was found to be similar to the findings of some selected studies (11-14), but their long-term efficacy is controversial (16). There are two reasons for this: firstly, the sample size was small and the rate of losing to follow-up was high in the long term, which fails to give an accurate reflection the real situation; and secondly, Some patients have difficulty maintaining long-term high-quality breathing exercise, and cannot guarantee the quality of exercise.
Yang et al. (19) showed a positive correlation between anxiety and depression in GERD patients and disease severity. The symptoms of anxiety and depression and diseases in patients often interact with each other, and may affect patients’ life and work due to repeated long-term symptoms such as acid regurgitation, belching, and heartburn, causing anxiety and depression, while long-term anxiety and depression may also cause over-sensitivity and aggravate symptoms. Self-assessment of anxiety and depression is subjective and uncertain to some extent, and short-term breathing exercises may not work, resulting in differences in outcomes.
The effects of breathing exercises on acid suppressant consumption in patients with GERD
PPIs can be used to diagnose GERD and to treat and relieve symptoms (20). It is easy to calculate the consumption of antacids or the proportion of people who stop taking them as objective indicators of disease severity. In the included studies, the patients used PPIs (such as: Rabeprazole) to control their symptoms, and before the experiment, all patients received routine PPI drugs treatment to ensure each had similar disease severity and to eliminate refractory GERD patients (21). Long-term breathing exercises had a greater effect than short-term observations (13,16).
The effects of breathing exercises on the anti-reflux barrier in patients with GERD
The function of anti-reflux barrier at the lower end of the esophagus is weakened in GERD patients, so gastric acid may enter the esophagus and cause damage to the esophageal mucosa (22). The CD is a skeletal muscle, which can be strengthened through physical exercise like other striated muscles. Although this is a variety of different exercises, their goal is always to strengthen these muscles and to enhance their anti-reflux mechanisms. Different studies have measured strength in different ways and breathing exercises have been shown to improve CD tension, although the effect of strengthen LES and EGJ is still controversial (13,16).
In addition to improving the function of the anti-reflux barrier, breathing exercises may also have other mechanisms, such as reducing the frequency of one-time esophageal relaxation and increasing the rate of gastric emptying (14). At present, many research conclusions are still controversial, so larger sample sizes and more refined clinical trials are needed to explore the efficacy and specific mechanisms of breathing exercises in the treatment of GERD.
Limitations
This study has a number of limitations. Firstly, the included literature included RCTs and general prospective studies, which showed differences in the methods of breathing exercises, and so their results may be uncertain to some extent. Secondly, there was a lack of effective monitoring of the patients in the studies, and the quality of the exercises they were carrying out cannot be guaranteed. Thirdly, only seven studies were included, and the total sample size of these studies was also small. Furthermore, every study was published in English, and there is therefore a possibility that literature in other languages was omitted. Finally, these studies came from different countries and regions, with differences in race and levels of physical fitness, and this may have affected the final results.
Conclusions
This study showed that breathing exercises can help GERD patients reduce the symptoms of gastroesophageal reflux, improve their quality of life, and decrease acid suppression usage, and that their specific mechanism may be to strengthen the anti-reflux barrier function. Therefore, GERD patients may experience better therapeutic effects through treatment with general drug therapy in conjunction with professional breathing exercises.
Acknowledgments
Funding: This study was supported financially by Medicine and Health Science and Technology Plan Projects in Zhejiang Province (NO: 2020RC108).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Richter JE, Rubenstein JH. Presentation and epidemiology of gastroesophageal reflux disease. Gastroenterology 2018;154:267-76. [Crossref] [PubMed]
- Ness-Jensen E, Hveem K, El-Serag H, et al. Lifestyle Intervention in Gastroesophageal Reflux Disease. Clin Gastroenterol Hepatol 2016;14:175-82.e1-3.
- Herbella FA, Patti MG. Gastroesophageal reflux disease: From pathophysiology to treatment. World J Gastroenterol 2010;16:3745-9. [Crossref] [PubMed]
- Brunner S, Fass R, Gerson LB. Value of the Proton Pump Inhibitor (PPI) Test for Patients with GERD, NCCP, and Extra-Esophageal GERD: A Meta-Analysis: 433. Am J Gastroenterol 2016;111:S194. [Crossref]
- Scarpellini E, Ang D, Pauwels A, et al. Management of refractory typical GERD symptoms. Nat Rev Gastroenterol Hepatol 2016;13:281-94. [Crossref] [PubMed]
- Laine L, Nagar A. Long-term PPI use: balancing potential harms and documented benefits. Am J Gastroenterol 2016;111:913-5. [Crossref] [PubMed]
- Devitt J, Lyon C, Swanson SB, et al. What are the risks of long-term PPI use for GERD symptoms in patients > 65 years? J Fam Pract 2019;68:E18-9. [PubMed]
- Casale M, Sabatino L, Moffa A, et al. Breathing training on lower esophageal sphincter as a complementary treatment of gastroesophageal reflux disease (GERD): a systematic review. Eur Rev Med Pharmacol Sci 2016;20:4547-52. [PubMed]
- Gyawali CP, Kahrilas PJ, Savarino E, et al. Modern diagnosis of GERD: the Lyon Consensus. Gut 2018;67:1351-62. [Crossref] [PubMed]
- Shuster JJ. Review: Cochrane handbook for systematic reviews for interventions, Version 5.1.0, published 3/2011. Higgins JP, Green S, editors. Research Synthesis Methods 2011;2:126-30.
- Moffa A, Oliveto G, Matteo FD, et al. Modified inspiratory muscle training (m-IMT) as promising treatment for gastro-oesophageal reflux disease (GERD). Acta Otorrinolaringol Esp 2020;71:65-9. [Crossref] [PubMed]
- Ong AM, Chua LT, Khor CJ, et al. Diaphragmatic Breathing Reduces Belching and Proton Pump Inhibitor Refractory Gastroesophageal Reflux Symptoms. Clin Gastroenterol Hepatol 2018;16:407-16.e2. [Crossref] [PubMed]
- Sun X, Shang W, Wang Z, et al. Short-term and long-term effect of diaphragm biofeedback training in gastroesophageal reflux disease: an open-label, pilot, randomized trial. Dis Esophagus 2016;29:829-36. [Crossref] [PubMed]
- Nobre e Souza MÂ, Lima MJ, Martins GB, et al. Inspiratory muscle training improves antireflux barrier in GERD patients. Am J Physiol Gastrointest Liver Physiol 2013;305:G862-7. [Crossref] [PubMed]
- da Silva RC, de Sá CC, Pascual-Vaca ÁO, et al. Increase of lower esophageal sphincter pressure after osteopathic intervention on the diaphragm in patients with gastroesophageal reflux. Dis Esophagus 2013;26:451-6. [Crossref] [PubMed]
- Eherer AJ, Netolitzky F, Hogenauer C, et al. Positive effect of abdominal breathing exercise on gastroesophageal reflux disease: a randomized, controlled study. Am J Gastroenterol 2012;107:372-8. [Crossref] [PubMed]
- Carvalho de Miranda Chaves R, Suesada M, et al. Respiratory physiotherapy can increase lower esophageal sphincter pressure in GERD patients. Respir Med 2012;106:1794-9. [Crossref] [PubMed]
- Velanovich V. The development of the GERD-HRQL symptom severity instrument. Dis Esophagus 2007;20:130-4. [Crossref] [PubMed]
- Yang XJ, Jiang HM, Hou XH, et al. Anxiety and depression in patients with gastroesophageal reflux disease and their effect on quality of life. World J Gastroenterol 2015;21:4302-9. [Crossref] [PubMed]
- Gasiorowska A, Fass R. The proton pump inhibitor (PPI) test in GERD: does it still have a role? J Clin Gastroenterol 2008;42:867-74. [Crossref] [PubMed]
- Fass R, Gasiorowska A. Refractory GERD: what is it? Curr Gastroenterol Rep 2008;10:252-7. [Crossref] [PubMed]
- Pandolfino JE, Kim H, Ghosh SK, et al. High-resolution manometry of the EGJ: an analysis of crural diaphragm function in GERD. Am J Gastroenterol 2007;102:1056-63. [Crossref] [PubMed]



