
A case report of a woman after childbirth with a dehisced abdominal wound as well as fat liquefaction and large skin necrosis
Introduction
The high-frequency electric knife is a common apparatus in surgical operations, especially abdominal surgery. An abdominal binder is a wide belt that surrounds the abdomen, which is also often used after laparotomy (1). A systematic review showed that abdominal binders could reduce post-operative emotional distress, but their effect on postoperative pain after laparotomy remains unclear (2). However, a randomized control trial demonstrated that abdominal binders were useful in pain management instead of pain-killer (3). At the same time, patients after cesarean section in China think the abdominal binder has the characteristic of shaping.
Ignoring the many benefits of the high-frequency electric knife and an abdominal binder such as easy operation, pain management, and shaping, etc., they also have many disadvantages of poor healing rates and high infection. So, they may extraordinarily delay abdominal incision healing (4). The reference number 4 is related to the high-frequency electric knife—there is no citation about the abdominal binder in this study.
In this case report, the dehisced abdominal wound, as well as fat liquefaction and large skin necrosis, was caused by both the high-frequency electric knife and an abdominal binder. We used negative pressure wound therapy (NPWT) to treat the patient with a satisfactory result. No earlier cases have been issued in China. And it is different from a former case of a gravid patient with a dehisced abdominal wound (5). So, the case is very worthwhile to report.
Case presentation
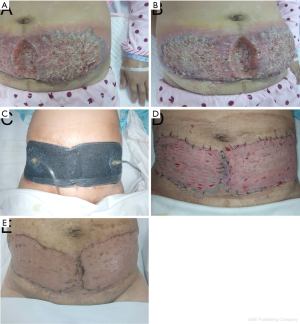
In August 2016, a 40-year-old woman with a temperature of 38.9 °C after cesarean delivery was admitted to our hospital because of abdominal fat liquefaction with large skin necrosis for 6 days (Figure 1A,B). There was a long and deep skin incision defect with the size of about 5 cm × 12 cm long and 4cm deep in the abdominal site, and large skin necrosis both sides along to the axillary front line with wound size of 18 cm × 55 cm, which area had a large number of yellow liquid leakage and obvious swelling.
After admitted, the wound tissue and secretion were cultured: no growth of bacteria and fungi; blood tests and biochemical were detected: white blood cell 36.43×109/L, hemoglobin 100 g/L, platelet 544×109/L, C protein 76.41 mg/L, 46.4 g/L of total proteins, albumin 23.5 g/L, alkaline phosphatase 152 U/L.
The 2nd day after admitted, the wound debridement was operated on, which some fat degenerated and a large number of yellow-white fluid exudation with little granulation tissue growing up. Complete removal of liquefaction necrosis of the tissue was managed through vacuum sealing drainage (VSD). After the treatment of postoperative, we started her on intravenous meropenem (0.5 g every 8 h) combining with teicoplanin (0.2 g every 8 h), and an amount of intravenous nutritional support. After the operation, the patient got an elevated temperature of 38.1–38.4 °C with intermittent fever.
On the 6th day, a little bit of yellow exudate was found on the right abdomen, then the next day in the operating room, some residual liquefactive and necrotic tissues and yellow liquid leakage were debrided extensively using vacuum-assisted closure (VAC) treatment. Body temperature fell gradually to normal postoperative, and we stop using the teicoplanin.
On the 14th day, the wound with granulation tissue was fresh and red; therefore, autologous skin grafting combining with VAC was performed, changing meropenem to cefminox sodium (2 g every 8 h) intravenously. Removing the VAC device in 5 days, grafted skin survived (Figure 1C,D), so we changed cefminox to mezlocillin sodium (2.5 g every 8 h) and used conventional wound dressing until the 25th day. On the 25th day, the patient recovered from the wound and gone back home (Figure 1E).
Discussion
The high-frequency electric knife and abdominal binder are often used in abdominal surgery, owing to their straightforward operation, pain management, and the like. Some studies showed that abdominal binders could reduce post-operative emotional distress and pain.
In this case, the patient is 155 cm high, 54 kg weight, and 22.48 kg/m2 for BMI (Body mass index), belonging to normal ranges, but abdominal fat is much thicker. Reviewing the patient’s history, we consider early using an abdominal binder, which could squeeze abdominal fat, and using a high-frequency electric knife during surgery, may lead to adipose cells burst (6), releasing large fatty acids along both abdominal sides with penetration under the abdominal binder. For long-term soaking, a local physician and the patient treated improperly following skin necrosis, resulting in enormous inflammatory cell factors released, causing Domino effect. So, we supposed the case of fat liquefaction with large skin necrosis resulted from adipose hypertrophy caused by using an electric knife and an abdominal binder.
With the improvement of people's living standards in China, more patients come into view of keeping a decent shape. So, it should avoid using the electric knife to reduce fat necrosis occur. And it should be emphasized and noted of patients with abdominal obesity when using the electric knife. Besides, people tend to think an abdominal binder could reduce pain and anxiety, but the other studies did not find that (7,8). At the same time, because of its significant role in shaping, the binder has been becoming immensely popular among young women after laparotomy. However, we should keep an eye on postoperative dehisced incision as well as fat liquefaction that sometimes occurs.
In recent years, NPWT (NPWT is the general term of VSD and VAC) has been used for various wounds, including closed incisions, acute and chronic wounds, and burns, which has become an increasing popular and common method and could significantly accelerate wound healing, compared with standard dressings (9). NPWT could prompt removal of fat necrosis as well as exudation and completely removal of the pro-inflammatory mediators, reducing contamination, edema, and inflammation (10). And NPWT also could increase skin blood flow, eliminate gaps, and fix the wound, thus promoting healing and creating advantages for skin grafts (10).
In this case, fat liquefaction with large skin necrosis is seen. Clinical physicians should give belly fat hypertrophy in pregnant women's attention. And we must increase awareness of incision fat liquefaction, fully preparing for the perioperative period, and taking measures to reduce and avoid the occurrence of the postoperative dehisced incision as well as fat liquefaction. This case highlights the need for early detection, diagnosis, treatment of postoperative dehisced incision as well as fat liquefaction and promotes wound healing.
Acknowledgments
Funding: This work was supported by the Key research and development project of Jiangxi provincial science and technology department (20171ACG70004 to Guanghua Guo).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The ethical review committee approved this study of The First Affiliated Hospital of Nanchang University. Consent for publication was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cheifetz O, Lucy SD, Overend TJ, et al. The effect of abdominal support on functional outcomes in patients following major abdominal surgery: a randomized controlled trial. Physiother Can 2010;62:242-53. [Crossref] [PubMed]
- Rothman JP, Gunnarsson U, Bisgaard T. Abdominal binders may reduce pain and improve physical function after major abdominal surgery - a systematic review. Dan Med J 2014;61:A4941. [PubMed]
- Ghana S, Hakimi S, Mirghafourvand M, et al. The Effects of Abdominal Binder on Wound Healing and Consumed Pain Medications After Cesarean Section: A Randomized Control Trial. Iran Red Crescent Med J 2017;19:e44119. [Crossref]
- Ji GW, Wu YZ, Wang X, et al. Experimental and clinical study of influence of high-frequency electric surgical knives on healing of abdominal incision. World J Gastroenterol 2006;12:4082-5. [Crossref] [PubMed]
- Asukai K, Kashiwazaki M, Koizumi K, et al. A case report of a 19-week gravid patient with a dehisced abdominal wound and treated with V.A.C. ATS(®) Therapy System. Int Wound J 2016;13:992-5. [Crossref] [PubMed]
- Neira R, Arroyave J, Ramirez H, et al. Fat liquefaction: effect of low-level laser energy on adipose tissue. Plast Reconstr Surg 2002;110:912-22; discussion 923-5. [Crossref] [PubMed]
- Gillier CM, Sparks JR, Kriner R, et al. A randomized controlled trial of abdominal binders for the management of postoperative pain and distress after cesarean delivery. Int J Gynaecol Obstet 2016;133:188-91. [Crossref] [PubMed]
- Myers JR, Gillier CM, Kriner RM, et al. The use of abdominal binders in patients undergoing cesarean delivery: a prospective randomized controlled trial. Obstet Gynecol 2014;123:160S-S.
- Li PY, Yang D, Liu D, et al. Reducing Surgical Site Infection with Negative-Pressure Wound Therapy After Open Abdominal Surgery: A Prospective Randomized Controlled Study. Scand J Surg 2017;106:189-95. [Crossref] [PubMed]
- Kilpadi DV, Cunningham MR. Evaluation of closed incision management with negative pressure wound therapy (CIM): hematoma/seroma and involvement of the lymphatic system. Wound Repair Regen 2011;19:588-96. [Crossref] [PubMed]


